| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| 5g |
|
||
| 10g |
|
||
| Other Sizes |
|

| 体外研究 (In Vitro) |
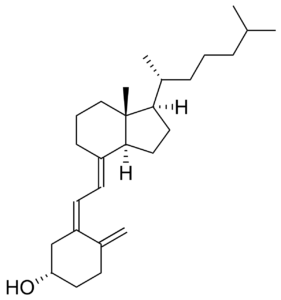
维生素 D3 是维生素 D 的体内非活性分子。为了激活维生素 D3,它要经历两个羟基化过程。 25-羟化酶 (CYP27A1) 和可能的其他酶(例如 CYP2R1)在肝脏中羟化维生素 D3,产生循环激素原 25-羟基维生素 D3 [25(OH)D3][1]。肾脏使用 1-α-羟化酶进行第二次羟基化,产生 1,25-二羟基胆钙化醇或骨化三醇,即维生素 D 的生物活性形式[1]。维生素 D3(2-10 μM;24-48 小时)显示出抗增殖作用,该作用取决于时间和剂量。用10 μM维生素D3处理后,62% (IK)、52% (RL-95-2) 和55% (Hec-1A) 的活力在72小时后达到最低点。然而,暴露 24 小时后,活细胞没有明显减少[2]。胆钙化醇(10 μM;24-48 小时)可显着增加核 VDR 染色,并导致 IK 细胞局部激活 VDR[1]。
|
|---|---|
| 体内研究 (In Vivo) |
胆钙化醇(口服管饲;5 mg/kg;7 天)只会增加肝脏中 CCl4 的毒性,如血浆 ALT 和 AST(肝损伤的两个生化指标)水平升高所示。虽然小鼠肾钙含量没有显着差异,但它显着提高了小鼠肾钙水平[3]。
|
| 动物实验 |
Male ddY mice on CCl4 toxicity[3]
5 mg/kg Oral gavage; 5 mg/kg; 7 days |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Cholecalciferol is readily absorbed from the small intestine if fat absorption is normal. Moreover, bile is necessary for absorption as well. In particular, recent studies have determined aspects about the absorption of vitamin D, like the fact that a) the 25-hydroxyvitamin D metabolite of cholecalciferol is absorbed to a greater extent than the nonhydroxy form of cholecalciferol, b) the quantity of fat with which cholecalciferol is ingested does not appear to largely affect its bioavailability, and c) age does not apparently effect vitamin D cholecalciferol. It has been observed that administered cholecalciferol and its metabolites are excreted primarily in the bile and feces. Studies have determined that the mean central volume of distribution of administered cholecalciferol supplementation in a group of 49 kidney transplant patients was approximately 237 L. Studies have determined that the mean clearance value of administered cholecalciferol supplementation in a group of 49 kidney transplant patients was approximately 2.5 L/day. Readily absorbed from small intestine (proximal or distal); cholecalciferol may be absorbed more rapidly and completely than ergocalciferol. Elimination: Biliary/renal. /Vitamin D and analogs/ Many vitamin D analogs are readily absorbed from the GI tract following oral administration if fat absorption is normal. The presence of bile is required for absorption of ergocalciferol and the extent of GI absorption may be decreased in patients with hepatic, biliary, or GI disease (e.g., Crohn's disease, Whipple's disease, sprue). Because vitamin D is fat soluble, it is incorporated into chylomicrons and absorbed via the lymphatic system; approximately 80% of ingested vitamin D appears to be absorbed systemically through this mechanism, principally in the small intestine. Although some evidence suggested that intestinal absorption of vitamin D may be decreased in geriatric adults, other evidence did not show clinically important age-related alterations in GI absorption of the vitamin in therapeutic doses. It currently is not known whether aging alters the GI absorption of physiologic amounts of vitamin D. /Vitamin D analogs/ After absorption, ergocalciferol and cholecalciferol enter the blood via chylomicrons of lymph and then associate mainly with a specific alpha-globulin (vitamin D-binding protein). The hydroxylated metabolites of ergocalciferol and cholecalciferol also circulate associated with the same alpha-globulin. 25-Hydroxylated ergocalciferol and cholecalciferol are stored in fat and muscles for prolonged periods. Once vitamin D enters systemic circulation from lymph via the thoracic duct or from skin, it accumulates in the liver within a few hours. For more Absorption, Distribution and Excretion (Complete) data for CHOLECALCIFEROL (7 total), please visit the HSDB record page. Metabolism / Metabolites Within the liver, cholecalciferol is hydroxylated to calcifediol (25-hydroxycholecalciferol) by the enzyme vitamin D-25-hydroxylase. At the kidney, calcifediol subsequently serves as a substrate for 1-alpha-hydroxylase, yielding calcitriol (1,25-dihydroxycholecalciferol), the biologically active form of vitamin D3. Metabolic activation of cholecalciferol and ergocalciferol occurs in 2 steps, the first in the liver and the second in the kidneys. Metabolic activation of calcifediol occurs in the kidneys; dihydrotachysterol, alfacalcidol and doxercalciferol are activated in the liver. Normal combined (ie, 25-hydroxyvitamin D) plasma concentrations of 25-hydroxycholecalciferol (calcifediol) and 25-hydroxyergocalciferol, which are the major circulating metabolites of cholecalciferol and ergocalciferol, have been reported to range from 8-80 ng/mL, depending on the assay used, and vary with exposure to UV light. A commonly reported range for the lower limit of normal is 8-15 ng/mL, depending on geographic location (eg, Southern California would be higher than Massachusetts). In the liver, ergocalciferol and cholecalciferol are converted in the mitochondria to their 25-hydroxy derivatives by the enzyme vitamin D 25-hydroxylase. Vitamin D 25-hydroxylase activity is regulated in the liver by concentrations of vitamin D and its metabolites; therefore, increases in the systemic circulation of the 25-hydroxy metabolites following exposure to sunlight or ingestion of vitamin D are relatively modest compared with cumulative production or intake of the vitamin. Serum concentrations of nonhydroxylated vitamin D are short-lived as a result of storage in fat or metabolism in the liver. In the kidneys, these metabolites are further hydroxylated at the 1 position by the enzyme vitamin D 1-hydroxylase to their active forms, 1,25-dihydroxycholecalciferol (calcitriol) and 1,25-dihydroxyergocalciferol. ... Activity of the vitamin D 1-hydroxylase enzyme requires molecular oxygen, magnesium ion, and malate and is regulated principally by PTH in response to serum concentrations of calcium and phosphate, and perhaps by circulating concentrations of 1,25-dihydroxyergocalciferol and 1,25-dihydroxycholecalciferol. Other hormones (ie, cortisol, estrogens, prolactin, and growth hormone) also may influence the metabolism of cholecalciferol and ergocalciferol. The hepatic enzyme system responsible for 25-hydroxylation of vitamin D /(vitamin D-25 hydroxylase)/ is associated with the microsomal and mitochondrial fractions of homogenates and requires NADPH (nicotinamide adenine dinucleotide phosphate, reduced form) and molecular oxygen. ... The enzyme system /in kidney/ responsible for 1-hydroxylation of 25-OHD (25-hydroxycholecalciferol) /(25-OHD-1-alpha-hydroxylase)/ is associated with mitochondria in the proximal tubules. It is a mixed function oxidase and requires molecular oxygen and NADPH as cofactors. Cytochrome P450, a flavoprotein, and ferredoxin are components of the enzyme complex. Within the liver, cholecalciferal is hydroxylated to calcidiol (25-hydroxycholecalciferol) by the enzyme 25-hydroxylase. Within the kidney, calcidiol serves as a substrate for 1-alpha-hydroxylase, yielding calcitriol (1,25-dihydroxycholecalciferol), the biologically active form of vitamin D3. Half Life: Several weeks Biological Half-Life At this time, there have been resources that document the half-life of cholecalciferol as being about 50 days while other sources have noted that the half-life of calcitriol (1,25-dihydroxyvitamin D3) is approximately 15 hours while that of calcidiol (25-hydroxyvitamin D3) is about 15 days. Moreover, it appears that the half-lives of any particular administration of vitamin d can vary due to variations in vitamin d binding protein concentrations and genotype in particular individuals. The Vitamin /D/ disappears from plasma with a half-life of 19 to 25 hr but is stored in fat depots for prolonged periods. ... The 25-hydroxy derivative has a biological half-life of 19 days ... The plasma half-life of calcitriol /(1,25-dihydroxy-vitamin D)/ is estimated to be between 3 and 5 days in human beings ... |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
The first step involved in the activation of vitamin D3 is a 25-hydroxylation which is catalysed by the 25-hydroxylase in the liver and then by other enzymes. The mitochondrial sterol 27-hydroxylase catalyses the first reaction in the oxidation of the side chain of sterol intermediates. The active form of vitamin D3 (calcitriol) binds to intracellular receptors that then function as transcription factors to modulate gene expression. Like the receptors for other steroid hormones and thyroid hormones, the vitamin D receptor has hormone-binding and DNA-binding domains. The vitamin D receptor forms a complex with another intracellular receptor, the retinoid-X receptor, and that heterodimer is what binds to DNA. In most cases studied, the effect is to activate transcription, but situations are also known in which vitamin D suppresses transcription. Calcitriol increases the serum calcium concentrations by: increasing GI absorption of phosphorus and calcium, increasing osteoclastic resorption, and increasing distal renal tubular reabsorption of calcium. Calcitriol appears to promote intestinal absorption of calcium through binding to the vitamin D receptor in the mucosal cytoplasm of the intestine. Subsequently, calcium is absorbed through formation of a calcium-binding protein. Protein Binding The protein binding documented for cholecalciferol is 50 to 80%. Specifically, in the plasma, vitamin D3 (from either diet or the skin) is bound to vitamin D-binding protein (DBP) produced in the liver, for transport to the liver. Ultimately, the form of vitamin D3 reaching the liver is 25-hydroxylated, and such 25-hydroxycholecalciferol is bound to DBP (α2-globulin) whilst circulating in the plasma. Toxicity Data LC50 (rat) = 130-380 ppm/4hr Interactions Corticosteroids counteract the effects of vitamin D analogs. /Vitamin D analogs/ Concurrent administration of thiazide diuretics and pharmacologic doses of vitamin D analogs in patients with hypoparathyroidism may result in hypercalcemia which may be transient and self-limited or may require discontinuance of vitamin D analogs. Thiazide-induced hypercalcemia in hypoparathyroid patients is probably caused by increased release of calcium from bone. /Vitamin D analogs/ Excessive use of mineral oil may interfere with intestinal absorption of vitamin D analogs. /Vitamin D analogs/ Orlistat may result in decreased GI absorption of fat-soluble vitamins such as vitamin D analogs. At least 2 hours should elapse between (before or after) any orlistat dose and vitamin D analog administration ... . /Vitamin D analogs/ For more Interactions (Complete) data for CHOLECALCIFEROL (6 total), please visit the HSDB record page. |
| 参考文献 | |
| 其他信息 |
Therapeutic Uses
Bone Density Conservation Agents; Vitamins MEDICATION (VET): Nutritional factor (Antirachitic) Therapeutic doses of specific vitamin D analogs are used in the treatment of chronic hypocalcemia, hypophosphatemia, rickets, and osteodystrophy associated with various medical conditions including chronic renal failure, familial hypophosphatemia, and hypoparathyroidism (postsurgical or idiopathic, or pseudohypoparathyroidism). Some analogs have been found to reduct elevated parathyroid hormone concentrations in patients with renal osteodystrophy associated with hyperparathyroidism. Theoretically, any of the vitamin D analogs may be used for the above conditions, However, because of their pharmacologic properties, some may be more useful in certain situations than others. Alfacalcidol, calcitriol, and dihydrotachysterol are usually preferred in patients with renal failure since these patients have impaired ability to synthesize calcitriol from cholecalciferol and ergocalciferol; therefore, the response is more predictable. In addition, their shorter half-lives may make toxicity easier to manage (hypercalcemia reverses more quickly). Ergocalciferol may not be the preferred agent in the treatment of familial hypophosphatemia or hypoparathyroidism because the large doses needed are associated with a risk of overdose and hypercalcemia; dihydrotachysterol and calcitriol may be preferred. /Included in US product labeling/ Drug Warnings Studies have shown that the elderly may have an increased need for vitamin D due to a possible decrease in the capacity of the skin to produce previtamin D3 or a decrease in exposure to the sun or impaired renal function or impaired vitamin D absorption. Doses of vitamin D analogs that do not exceed the physiologic requirement are usually nontoxic. However, some infants and patients with sarcoidosis or hypoparathyroidism may have increased sensitivity to vitamin D analogs. /Vitamin D analogs/ Acute or chronic administration of excessive doses of vitamin D analogs or enhanced responsiveness to physiologic amounts of ergocalciferol or cholecalciferol may lead to hypervitaminosis D manifested by hypercalcemia. /Vitamin D analogs/ Decreased renal function without hypercalcemia has also been reported in patients with hypoparathyroidism after long-term vitamin D analog therapy. Before therapy with vitamin D analogs is initiated, serum phosphate concentrations must be controlled. To avoid ectopic calcification, the serum calcium (in mg/dL) times phosphorus (in mg/dL) should not be allowed to exceed 70. Because administration of vitamin D analogs may increase phosphate absorption, patients with renal failure may require adjustment in the dosage of aluminum-containing antacids used to decrease phosphate absorption. /Vitamin D analogs/ For more Drug Warnings (Complete) data for CHOLECALCIFEROL (10 total), please visit the HSDB record page. Pharmacodynamics The in vivo synthesis of the predominant two biologically active metabolites of vitamin D occurs in two steps. The first hydroxylation of vitamin D3 cholecalciferol (or D2) occurs in the liver to yield 25-hydroxyvitamin D while the second hydroxylation happens in the kidneys to give 1, 25-dihydroxyvitamin D. These vitamin D metabolites subsequently facilitate the active absorption of calcium and phosphorus in the small intestine, serving to increase serum calcium and phosphate levels sufficiently to allow bone mineralization. Conversely, these vitamin D metabolites also assist in mobilizing calcium and phosphate from bone and likely increase the reabsorption of calcium and perhaps also of phosphate via the renal tubules. There exists a period of 10 to 24 hours between the administration of cholecalciferol and the initiation of its action in the body due to the necessity of synthesis of the active vitamin D metabolites in the liver and kidneys. It is parathyroid hormone that is responsible for the regulation of such metabolism at the level of the kidneys. |
| 分子式 |
C27H44O
|
|---|---|
| 分子量 |
384.6377
|
| 精确质量 |
384.339
|
| 元素分析 |
C, 84.31; H, 11.53; O, 4.16
|
| CAS号 |
67-97-0
|
| 相关CAS号 |
Vitamin D3-d7;1627523-19-6;3-epi-Vitamin D3;57651-82-8;Vitamin D3-13C3;Vitamin D3-d3;80666-48-4;Vitamin D3-13C5
|
| PubChem CID |
5280795
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
1.0±0.1 g/cm3
|
| 沸点 |
496.4±24.0 °C at 760 mmHg
|
| 熔点 |
83-86 °C(lit.)
|
| 闪点 |
214.2±15.1 °C
|
| 蒸汽压 |
0.0±2.9 mmHg at 25°C
|
| 折射率 |
1.523
|
| LogP |
9.72
|
| tPSA |
20.23
|
| 氢键供体(HBD)数目 |
1
|
| 氢键受体(HBA)数目 |
1
|
| 可旋转键数目(RBC) |
6
|
| 重原子数目 |
28
|
| 分子复杂度/Complexity |
610
|
| 定义原子立体中心数目 |
5
|
| SMILES |
O([H])[C@@]1([H])C([H])([H])C([H])([H])C(=C([H])[H])/C(/C1([H])[H])=C(/[H])\C(\[H])=C1/C([H])([H])C([H])([H])C([H])([H])[C@@]2(C([H])([H])[H])[C@@]/1([H])C([H])([H])C([H])([H])[C@]2([H])[C@]([H])(C([H])([H])[H])C([H])([H])C([H])([H])C([H])([H])C([H])(C([H])([H])[H])C([H])([H])[H]
|
| InChi Key |
QYSXJUFSXHHAJI-YRZJJWOYSA-N
|
| InChi Code |
InChI=1S/C27H44O/c1-19(2)8-6-9-21(4)25-15-16-26-22(10-7-17-27(25,26)5)12-13-23-18-24(28)14-11-20(23)3/h12-13,19,21,24-26,28H,3,6-11,14-18H2,1-2,4-5H3/b22-12+,23-13-/t21-,24+,25-,26+,27-/m1/s1
|
| 化学名 |
(1S,3Z)-3-[(2E)-2-[(1R,3aS,7aR)-7a-methyl-1-[(2R)-6-methylheptan-2-yl]-2,3,3a,5,6,7-hexahydro-1H-inden-4-ylidene]ethylidene]-4-methylidenecyclohexan-1-ol
|
| 别名 |
Activated 7-dehydrocholesterol; Cholecalciferol; Calciol; Vitamin D3; Colecalciferol; Arachitol; Ricketon; Trivitan; Vigorsan; Deparal; Vigantol
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: (1). 本产品在运输和储存过程中需避光。 (2). 请将本产品存放在密封且受保护的环境中(例如氮气保护),避免吸湿/受潮。 (3). 该产品在溶液状态不稳定,请现配现用。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ~100 mg/mL (~259.98 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.08 mg/mL (5.41 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 20.8 mg/mL澄清DMSO储备液加入400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: 2.08 mg/mL (5.41 mM) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 悬浊液; 超声助溶。 例如,若需制备1 mL的工作液,可将 100 μL 20.8 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.08 mg/mL (5.41 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.5998 mL | 12.9992 mL | 25.9983 mL | |
| 5 mM | 0.5200 mL | 2.5998 mL | 5.1997 mL | |
| 10 mM | 0.2600 mL | 1.2999 mL | 2.5998 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Comparison Between Effect of Vitamin D Versus Dexmedetomidine in Patients with Head Trauma Using Interleukin 6
CTID: NCT06565338
Phase: Status: Completed
Date: 2024-11-04
|