| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| 5g |
|
||
| Other Sizes |
|
| 靶点 |
SGLT-2 ( IC50 = 3.1 nM ); SGLT-5 ( IC50 = 1.1 μM ); SGLT-6 ( IC50 = 2 μM ); SGLT-1 ( IC50 = 8.3 μM ); SGLT-4 ( IC50 = 11 μM )
|
|---|---|
| 体外研究 (In Vitro) |
体外活性:恩格列净对 hSGLT-2 的选择性是 hSGLT-1 的 >2500 倍(IC50 8300 nM),对 hSGLT-4 的选择性 >3500 倍,对 hSGLT-5 的选择性 >350 倍(IC50=1100) nM),选择性比 hSGLT-6 高 600 倍以上。恩格列净浓度高达 10 μM 时,未观察到 GLUT1 的相关抑制作用。在动力学结合实验中,[3H]-empagliflozin 在没有葡萄糖的情况下对 SGLT-2 显示出高亲和力,平均 Kd 为 57 nM,并且显示 [3H]-empagliflozin 与 SGLT-2 结合的半衰期在没有葡萄糖的情况下为 59 分钟。它与 SGLT-2 的结合与葡萄糖竞争。激酶测定:过表达hSGLT-1、-2、-4、-5或-6或rSGLT-1或-2的稳定细胞系用于钠依赖性单糖转运抑制测定。将细胞在 200 μL 摄取缓冲液(10 mM HEPES、137 mM NaCl、5.4 mM KCl、2.8 mM CaCl2、1.2 mM MgCl2、50 μg/ml 庆大霉素、0.1% BSA)中于 37°C 预孵育 25 分钟。在摄取实验开始前 15 分钟添加不同浓度的 10 μM 细胞松弛素 B 和测试化合物。通过在0.1 mM AMG(或相应的非放射性单糖)中添加0.6 μCi [14C]标记的单糖(即[14C]标记的AMG、葡萄糖、果糖、甘露糖或肌醇)来启动摄取反应。 37°C 孵育 60 分钟 (hSGLT-5)、90 分钟 (hSGLT-4) 或 4 小时 (hSGLT-2) 后,用 300 μL PBS 洗涤细胞 3 次,然后在 0.1 N NaOH 中间歇裂解摇动5分钟。将裂解物与 200 μL MicroScint 40 混合并摇动 15 分钟,然后在 TopCount NXT 中计数放射性。对于 SGLT-4 和 SGLT-5 测定,在添加摄取缓冲液之前,将细胞在预处理缓冲液(含有氯化胆碱而不是氯化钠的摄取缓冲液)中预孵育 25 分钟。细胞测定:当用一组过表达 SGLT-1、2、4、5 和 6 的人类细胞系进行测试时,恩格列净治疗在低剂量下比葡萄糖竞争性地结合 SGLT-2。在人近端肾小管细胞 (PTC) 细胞系 HK2 细胞中,恩格列净治疗 72 小时可抑制 SGLT-2 的表达,进而逆转高糖诱导的 TLR4 表达、NF-κB 结合、IL-6 分泌、AP-1 结合和CIV 表达。
|
| 体内研究 (In Vivo) |
狗体内恩格列净的暴露量很高,给予 5 mg/kg 恩格列净 24 小时后测得的血浆浓度比 IC50 高 100 倍以上。 ZDF 大鼠中恩格列净的总血浆清除率为 43 mL/min/kg,而狗中的总清除率为 1.8 mL/min/kg。 Empagliflozin 在 ZDF 大鼠和狗中的 Cmax 分别为 167 nM 和 17254 nM。 ZDF 大鼠和狗的终末消除半衰期分别为 1.5 小时和 6.3 小时。恩格列净在 ZDF 大鼠中的生物利用度为 33.2%,而在狗中则更高,为 89.0%。恩格列净长期治疗可改善糖尿病大鼠的血糖控制和代谢综合征特征。
Empagliflozin 是一种强效、选择性的钠葡萄糖共转运蛋白-2抑制剂,正在开发用于治疗2型糖尿病。本系列研究旨在评估单剂量或多剂量Empagliflozin 对Zucker糖尿病脂肪大鼠的体内药理作用。单剂量Empagliflozin导致尿葡萄糖排泄量的剂量依赖性增加和血糖水平的降低。多次给药(5周)后,与赋形剂相比,1 mg/kg和3 mg/kg恩帕列净的空腹血糖水平分别降低了26%和39%。5周后,1 mg/kg和3 mg/kg的恩帕列净使HbA1c水平分别降低了0.3%和1.1%(从基线7.9%开始),而赋形剂则提高了1.1%。高胰岛素血症正常血糖钳夹表明,与赋形剂相比,多次服用恩帕列净后胰岛素敏感性有所改善。这些发现支持恩帕列净治疗2型糖尿病的发展。[2] Empagliflozin 在ZDF大鼠和比格犬体内的药代动力学[1] 表3总结了大鼠和狗的药代动力学参数。在狗中实现了高暴露量的Empagliflozin ,在给予5mg/kg的Empagiflozin后24小时测得的血浆浓度比IC50高出100倍以上(数据未显示)。尽管大鼠中恩帕列净的CL和BA仅为中度,但也达到了可接受的暴露量(表3)。因此,在比格犬和ZDF大鼠中,低剂量口服恩帕列净可以实现远高于SGLT-2 IC50的血浆浓度。 |
| 酶活实验 |
该钠依赖性单糖转运抑制测定使用过度表达 hSGLT-1、-2、-4、-5 或 -6 或 rSGLT-1 或 -2 的稳定细胞系。细胞在 200 μL 摄取缓冲液(10 mM HEPES、137 mM NaCl、5.4 mM KCl、2.8 mM CaCl2、1.2 mM MgCl2、50 μg /ml 庆大霉素,0.1% BSA)。在摄取实验开始前半小时,添加不同浓度的10μM细胞松弛素B和测试化合物。添加 0.6 μCi [14C] 标记的单糖,例如 [14C] 标记的 AMG、葡萄糖、果糖、甘露糖或肌醇,至 0.1 mM AMG(或相应的非放射性单糖)启动摄取反应。将细胞在 37°C 下孵育 60 分钟 (hSGLT-5)、90 分钟 (hSGLT-4) 或 4 小时 (hSGLT-2),然后用 300 μL PBS 洗涤 3 次,并在 0.1 N NaOH 中裂解 5 次。分钟,同时间歇摇晃。将裂解物与 200 μL MicroScint 40 混合并摇动 15 分钟后,使用 TopCount NXT 测量放射性。在添加摄取缓冲液之前,在 SGLT-4 和 SGLT-5 测试中,将细胞在预处理缓冲液(摄取缓冲液中含有氯化胆碱而不是 NaCl)中预孵育 25 分钟。
使用[3H]标记的Empagliflozin 进行放射性配体结合分析 在室温下,在96孔板中,在存在或不存在20 mM葡萄糖和指示浓度的[3H]-Empagliflozin的情况下,在含有137 mM NaCl的10 mM 4-(2-羟乙基)-1-哌嗪乙磺酸(HEPES)缓冲液(pH 7.4)中对膜(60µg/孔)进行了2小时的测定。通过浸渍有0.5%聚乙烯亚胺并用0.9%NaCl溶液预湿的GF/B滤板快速过滤来停止培养,并使用Harvester Filtermate 96用0.9%NaCl溶液(4°C)洗涤四次。将滤板干燥2小时,并向每个孔中加入50µl Microscint 20。使用TopCount NXT测量过滤器上保留的放射性。同时,通过将放射性配体结合研究中每孔添加的相同量的[3H]-Empagliflozin和4 ml Ultima Gold Scintilator添加到5 ml小瓶中,并使用Tricarb 2900TR进行测量,来确定测定中使用的实际活性量。在30µM达格列嗪存在的情况下,测定了非特异性[3H]-Empagliflozin-结合 在存在或不存在20mM葡萄糖的情况下测定动力学结合参数(更多细节见支持信息)。Graphpad Prism 5.0用于使用单结合位点模型的非线性回归计算平衡解离常数(Kd),并通过使用“先结合后解离”非线性回归的全局拟合程序计算缔合速率常数(Kon)和解离速率常数值。 |
| 细胞实验 |
在一组过表达 SGLT-1、2、4、5 和 6 的人类细胞系上进行的测试表明,恩格列净治疗在低剂量下比葡萄糖竞争性地结合 SGLT-2。在人近端肾小管细胞 (PTC) 细胞中在 HK2 细胞系中,Empagliflozin 处理 72 小时可抑制 SGLT-2 的表达,进而逆转高糖诱导的 TLR4 表达、NF-κB 结合、IL-6 分泌、AP-1 结合和 CIV 表达。
钠/葡萄糖协同转运蛋白2(SGLT2)抑制剂是用于治疗糖尿病患者的口服降糖药。SGLT2抑制剂通过抑制近端肾小管细胞(PTC)中的主要葡萄糖转运蛋白SGLT2来阻断过滤葡萄糖的再吸收,从而导致糖尿和血糖降低。我们研究了SGLT2抑制剂Empagliflozin 的肾脏保护作用,以确定阻断葡萄糖进入肾PTC是否会减少细胞对高糖的炎症和纤维化反应。我们使用了人类PTC的体外模型。将HK2细胞(人肾PTC系)暴露于对照5 mM、高糖(HG)30 mM或促纤维化细胞因子转化生长因子β(TGFβ1;0.5 ng/ml)中,在存在和不存在Empagliflozin的情况下,持续72小时。评估SGLT1和2的表达以及各种炎症/纤维化标志物。染色质免疫沉淀试验用于确定磷酸化smad3与SGLT2基因启动子区的结合。我们的数据显示,TGFβ1而非HG增加了SGLT2的表达,这是通过磷酸化smad3发生的。HG诱导Toll样受体-4的表达,增加核因子κB(NF-κB)和激活蛋白1的核脱氧核糖核酸结合,诱导IV型胶原表达和白细胞介素-6分泌,所有这些都被恩帕列净减弱。Empagliflozin 没有减少高迁移率族蛋白1诱导的NF-κB,表明其作用与糖毒性的降低特异性相关。HG或恩帕列净对SGLT1和GLUT2的表达没有显著影响。总之,恩帕列净通过阻断葡萄糖转运减少HG诱导的炎症和纤维化标志物,并且没有诱导SGLT1/GLUT2表达的代偿性增加。尽管HG本身在我们的模型中不调节SGLT2的表达,但TGFβ通过磷酸化smad3增加SGLT2表达[3]。 |
| 动物实验 |
Mice: Male C57BL/6J mice (10 weeks of age) are used. The mice in the experimental group receive 3 or 10 mg/kg of Empagliflozin orally once a day for 8 days via oral gavage; the vehicle group receives the same volume of HEC alone.
Compounds and Dosing[2] Empagliflozin [BI 10773] was administered by oral gavage using 0.5% hydroxyethylcellulose as a vehicle. The compound was moistened with Polysorbat 80 (polyoxyethylene sorbitan monooleate) before solution in vehicle (final concentration: 0.015%).[2] Animal Studies [2] Male Zucker diabetic fatty (ZDF) rats (ZDF-Leprfa/Crl) were housed in groups at controlled temperature and humidity conditions, with a 12-h light/dark cycle, and ad libitum access to food [diet 2437, containing 4.5% sucrose] and water. Urinary glucose excretion (UGE) and blood glucose levels were assessed in ZDF rats (10 and 13 weeks old, respectively) after single doses of Empagliflozin . Food was withdrawn during the experiments. Urine was collected for 24 h after dosing with 1 or 3 mg/kg Empagliflozin or vehicle using metabolic cages. Blood samples were obtained by tail bleed at 0.5, 1, 2, 3, 4, 5 and 7 h after dosing with 0.1, 0.3, 1 or 3 mg/kg Empagliflozin or vehicle. Glucose homeostasis was investigated in a 5-week study in 12-week-old ZDF rats given multiple, once-daily doses of Empagliflozin . Blood samples (tail bleed) were taken from overnight fasted animals 16 h after dosing with 0.3, 1 or 3 mg/kg Empagliflozin or vehicle. Oral glucose tolerance tests (OGTTs) were performed on days 2 and 37. Overnight fasted animals were challenged with 2 g/kg glucose 16 h after administration of 3 mg/kg Empagliflozin . Blood samples were taken before and 0.25, 0.5, 1, 1.5, 2 and 3 h after glucose load. Hyperinsulinaemic–Euglycaemic Clamp [2] Animals from the 5-week study were subjected to a hyperinsulinaemic–euglycaemic clamp 4 days after last dose [basal fasting blood glucose levels: 11.8 ± 0.8 mM (vehicle) and 9.0 ± 0.5 mM (3 mg/kg Empagliflozin )]. Indwelling catheters were inserted in the right jugular vein (for insulin/glucose infusion) and in the right carotid artery (for blood sampling). Overnight fasted rats received a primed-continuous infusion of insulin at 48 mU/kg/min (10 ml/h) for 5 min, followed by 4.8 mU/kg/min (1 ml/h) for up to 120 min. Isotopically labelled glucose was infused at 10 mg/kg/min during the prime phase and at 1 mg/kg/min during the continuous phase [d-Glucose-(13C6), 99 atom% 13C]. After the prime phase, a variable infusion of a 7.5% (w/v) glucose solution was administered to clamp the blood glucose concentration at 5 mM. The rate of endogenous glucose appearance, Ra, was calculated using the formula: Ra = GIR*/SA–GIR, where GIR* = glucose infusion rate of (13C)-glucose; SA = specific activity of (13C)-glucose in blood during steady state [(13C)-glucose / ([12C]-glucose + [13C]-glucose)]; and GIR = total glucose infusion rate [(12C)-glucose + (13C)-glucose]. The rate of endogenous glucose disappearance, Rd, was calculated as Rd = GIR +Ra. Pharmacokinetics and pharmacodynamics of Empagliflozin in beagle dogs and ZDF rats [1] Animals were fasted overnight before and for 2 (rats) or 4 (dogs) h after dosing, and serial blood samples taken up to 24 or 48 h after dosing from rats and dogs, respectively. See the Supporting Information for details of dosing. Pharmacokinetic parameters were calculated by non-compartmental methods as follows. Area under the plasma concentration-time curve (AUC0−t) to the last quantifiable time point was calculated using the linear trapezoidal method. AUC0−t was extrapolated to infinity (AUC0−∞) using log-linear regression of the terminal portion of the individual curves to estimate the terminal elimination half-life (t½). Area under the moment curve (AUMC0−∞) was calculated in a manner similar to AUC0−∞. Mean residence time was calculated as AUMC0−∞/AUC0−∞, total plasma clearance (CL) as dose/AUC0−∞, and steady state volume of distribution (Vss) as (Dose × AUMC0−∞)/(AUC0−∞× AUC0−∞). Apparent bioavailability (BA) was calculated as (oral AUC0−∞/oral dose)/(intravenous AUC0−∞/intravenous dose) × 100. Maximum concentration (Cmax) and time of maximum concentration (tmax) are also reported. Individual and mean pharmacokinetic parameters were calculated using Kinetica version 4.41 or ToxKin™ version 3. The means and standard deviations (SDs) of the plasma concentrations were calculated using Microsoft Excel 2002 or ToxKin™. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Following oral administration, peak plasma concentrations are reached in approximately 1.5 hours (Tmax). At steady-state, plasma AUC and Cmax were 1870 nmol·h/L and 259 nmol/L, respectively, following therapy with empagliflozin 10mg daily and 4740 nmol·h/L and 687 nmol/L, respectively, following therapy with empagliflozin 25mg daily. Administration with food does not significantly affect the absorption of empagliflozin. After oral administration of radiolabeled empagliflozin approximately 41.2% of the administered dose was found eliminated in feces and 54.4% eliminated in urine. The majority of radioactivity in the feces was due to unchanged parent drug while approximately half of the radioactivity in urine was due to unchanged parent drug. The estimated apparent steady-state volume of distribution is 73.8 L. Apparent oral clearance was found to be 10.6 L/h based on a population pharmacokinetic analysis. Metabolism / Metabolites Empagliflozin undergoes minimal metabolism. It is primarily metabolized via glucuronidation by 5'-diphospho-glucuronosyltransferases 2B7, 1A3, 1A8, and 1A9 to yield three glucuronide metabolites: 2-O-, 3-O-, and 6-O-glucuronide. No metabolite represented more than 10% of total drug-related material. Biological Half-Life The apparent terminal elimination half-life was found to be 12.4 h based on population pharmacokinetic analysis. |
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation No information is available on the clinical use of empagliflozin during breastfeeding. Empagliflozin is an uncharged molecule that is 86% protein bound in plasma, so it is unlikely to pass into breastmilk in clinically important amounts. The manufacturer does not recommend empagliflozin during breastfeeding because of a theoretical risk to the infant's developing kidney. An alternate drug may be preferred, especially while nursing a newborn or preterm infant. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding Empagliflozin is approximately 86.2% protein-bound in plasma. |
| 参考文献 | |
| 其他信息 |
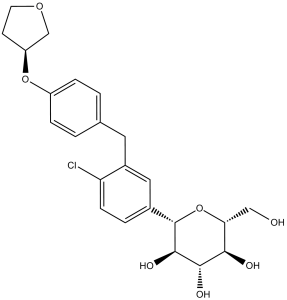
Empagliflozin is a C-glycosyl compound consisting of a beta-glucosyl residue having a (4-chloro-3-{4-[(3S)-tetrahydrofuran-3-yloxy]benzyl}phenyl group at the anomeric centre. A sodium-glucose co-transporter 2 inhibitor used as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. It has a role as a sodium-glucose transport protein subtype 2 inhibitor and a hypoglycemic agent. It is a C-glycosyl compound, an aromatic ether, a tetrahydrofuryl ether and a member of monochlorobenzenes.
Empagliflozin is an inhibitor of sodium-glucose co-transporter-2 (SGLT2), the transporters primarily responsible for the reabsorption of glucose in the kidney. It is used clinically as an adjunct to diet and exercise, often in combination with other drug therapies, for the management of type 2 diabetes mellitus. The first known inhibitor of SGLTs, phlorizin, was isolated from the bark of apple trees in 1835 and researched extensively into the 20th century, but was ultimately deemed inappropriate for clinical use given its lack of specificity and significant gastrointestinal side effects. Attempts at overcoming these limitations first saw the development of O-glucoside analogs of phlorizin (e.g. [remogliflozin etabonate]), but these molecules proved relatively pharmacokinetically unstable. The development of C-glucoside phlorizin analogs remedied the issues observed in the previous generation, and led to the FDA approval of [canagliflozin] in 2013 and both [dapagliflozin] and empagliflozin in 2014. As the most recently approved of the "flozin" drugs, empagliflozin carries the highest selectivity for SGLT2 over SGLT1 (approximately 2700-fold). Empagliflozin was further approved by the EMA in March 2022 and Health Canada in April 2022, making it the first and only approved treatment in Europe and Canada for adults with symptomatic chronic heart failure regardless of ejection fraction. Empagliflozin is a Sodium-Glucose Cotransporter 2 Inhibitor. The mechanism of action of empagliflozin is as a Sodium-Glucose Transporter 2 Inhibitor. Empagliflozin is an orally available competitive inhibitor of sodium-glucose co-transporter 2 (SGLT2; SLC5A2) with antihyperglycemic activity. Upon oral administration, empagliflozin selectively and potently inhibits SGLT2 in the kidneys, thereby suppressing the reabsorption of glucose in the proximal tubule. Inhibition of SGLT2 increases urinary glucose excretion by the kidneys, resulting in a reduction of plasma glucose levels in an insulin-independent manner. Inhibition of SGLT2 in the kidneys also suppresses the renal reabsorption of 1,5-anhydroglucitol (1,5AG). This lowers serum 1,5AG and neutrophil 1,5-anhydroglucitol-6-phosphate (1,5AG6P) levels, which may improve neutropenia and neutrophil dysfunction in patients with glycogen storage disease type Ib (GSD Ib). SGLT2, a transport protein exclusively expressed in the proximal renal tubules, mediates approximately 90% of renal glucose reabsorption from tubular fluid. See also: Empagliflozin; METformin Hydrochloride (component of); Empagliflozin; Linagliptin (component of) ... View More ... Drug Indication Empagliflozin is indicated as an adjunct to diet and exercise to improve glycemic control in patients aged 10 years and older with type 2 diabetes. It is used either alone or in combination with [metformin] or [linagliptin]. It is also indicated to reduce the risk of cardiovascular death in adult patients with both type 2 diabetes mellitus and established cardiovascular disease, either alone or as a combination product with metformin. An extended-release combination product containing empagliflozin, metformin, and linagliptin was approved by the FDA in January 2020 for the improvement of glycemic control in adults with type 2 diabetes mellitus when used adjunctively with diet and exercise. Empagliflozin is also approved to reduce the risk of cardiovascular mortality and hospitalization due to heart failure in adult patients with heart failure, either alone or in combination with metformin. It is also indicated in adults to reduce the risk of sustained decline in eGFR, end-stage kidney disease, cardiovascular death, and hospitalization in adults with chronic kidney disease at risk of progression. Empagliflozin is not approved for use in patients with type 1 diabetes. Type 2 diabetes mellitusJardiance is indicated for the treatment of adults with insufficiently controlled type 2 diabetes mellitus as an adjunct to diet and exerciseas monotherapy when metformin is considered in addition to other medicinal products for the treatment of diabetesFor study results with respect to combinations of therapies, effects on glycaemic control, and cardiovascular and renal events, and the populations studied, see sections 4. 4, 4. 5 and 5. 1. of the annex. Heart failureJardiance is indicated in adults for the treatment of symptomatic chronic heart failure.  Chronic kidney diseaseJardiance is indicated in adults for the treatment of chronic kidney disease.  Treatment of type II diabetes mellitus Treatment of ischaemic heart disease Treatment of type I diabetes mellitus Treatment of chronic kidney disease Prevention of cardiovascular events in patients with chronic heart failure Mechanism of Action The vast majority of glucose filtered through the glomerulus is reabsorbed within the proximal tubule, primarily via SGLT2 (sodium-glucose linked co-transporter-2) which is responsible for ~90% of the total glucose reabsorption within the kidneys. Na+/K+-ATPase on the basolateral membrane of proximal tubular cells utilize ATP to actively pump Na+ ions into the interstitium surrounding the tubule, establishing a Na+ gradient within the tubular cell. SGLT2 on the apical membrane of these cells then utilize this gradient to facilitate secondary active co-transport of both Na+ and glucose out of the filtrate, thereby reabsorbing glucose back into the blood – inhibiting this co-transport, then, allows for a marked increase in glucosuria and decrease in blood glucose levels. Empagliflozin is a potent inhibitor of renal SGLT2 transporters located in the proximal tubules of the kidneys and works to lower blood glucose levels via an increase in glucosuria. Empagliflozin also appears to exert cardiovascular benefits - specifically in the prevention of heart failure - independent of its blood glucose-lowering effects, though the exact mechanism of this benefit is not precisely understood. Several theories have been posited, including the potential inhibition of Na+/H+ exchanger (NHE) 1 in the myocardium and NHE3 in the proximal tubule, reduction of pre-load via diuretic/natriuretic effects and reduction of blood pressure, prevention of cardiac fibrosis via suppression of pro-fibrotic markers, and reduction of pro-inflammatory adipokines. Aims: Empagliflozin is a selective sodium glucose cotransporter-2 (SGLT-2) inhibitor in clinical development for the treatment of type 2 diabetes mellitus. This study assessed pharmacological properties of empagliflozin in vitro and pharmacokinetic properties in vivo and compared its potency and selectivity with other SGLT-2 inhibitors. Methods: [(14)C]-alpha-methyl glucopyranoside (AMG) uptake experiments were performed with stable cell lines over-expressing human (h) SGLT-1, 2 and 4. Two new cell lines over-expressing hSGLT-5 and hSGLT-6 were established and [(14)C]-mannose and [(14)C]-myo-inositol uptake assays developed. Binding kinetics were analysed using a radioligand binding assay with [(3)H]-labelled empagliflozin and HEK293-hSGLT-2 cell membranes. Acute in vivo assessment of pharmacokinetics was performed with normoglycaemic beagle dogs and Zucker diabetic fatty (ZDF) rats. Results: Empagliflozin has an IC(50) of 3.1 nM for hSGLT-2. Its binding to SGLT-2 is competitive with glucose (half-life approximately 1 h). Compared with other SGLT-2 inhibitors, empagliflozin has a high degree of selectivity over SGLT-1, 4, 5 and 6. Species differences in SGLT-1 selectivity were identified. Empagliflozin pharmacokinetics in ZDF rats were characterised by moderate total plasma clearance (CL) and bioavailability (BA), while in beagle dogs CL was low and BA was high. Conclusions: Empagliflozin is a potent and competitive SGLT-2 inhibitor with an excellent selectivity profile and the highest selectivity window of the tested SGLT-2 inhibitors over hSGLT-1. Empagliflozin represents an innovative therapeutic approach to treat diabetes. [1] |
| 分子式 |
C23H27CLO7
|
|---|---|
| 分子量 |
450.91
|
| 精确质量 |
450.144
|
| 元素分析 |
C, 61.26; H, 6.04; Cl, 7.86; O, 24.84
|
| CAS号 |
864070-44-0
|
| 相关CAS号 |
Empagliflozin-d4; 2749293-95-4
|
| PubChem CID |
11949646
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
1.4±0.1 g/cm3
|
| 沸点 |
664.5±55.0 °C at 760 mmHg
|
| 闪点 |
355.7±31.5 °C
|
| 蒸汽压 |
0.0±2.1 mmHg at 25°C
|
| 折射率 |
1.628
|
| LogP |
3.38
|
| tPSA |
108.61
|
| 氢键供体(HBD)数目 |
4
|
| 氢键受体(HBA)数目 |
7
|
| 可旋转键数目(RBC) |
6
|
| 重原子数目 |
31
|
| 分子复杂度/Complexity |
558
|
| 定义原子立体中心数目 |
6
|
| SMILES |
O[C@@H]1[C@@H](O)[C@H](O)[C@@H](CO)O[C@H]1C1C=CC(Cl)=C(CC2C=CC(O[C@@H]3COCC3)=CC=2)C=1
|
| InChi Key |
OBWASQILIWPZMG-QZMOQZSNSA-N
|
| InChi Code |
InChI=1S/C23H27ClO7/c24-18-6-3-14(23-22(28)21(27)20(26)19(11-25)31-23)10-15(18)9-13-1-4-16(5-2-13)30-17-7-8-29-12-17/h1-6,10,17,19-23,25-28H,7-9,11-12H2/t17-,19+,20+,21-,22+,23-/m0/s1
|
| 化学名 |
(2S,3R,4R,5S,6R)-2-[4-chloro-3-[[4-[(3S)-oxolan-3-yl]oxyphenyl]methyl]phenyl]-6-(hydroxymethyl)oxane-3,4,5-triol
|
| 别名 |
BI1-0773; CE0108; CS0940; PB23119; 864070-44-0; JARDIANCE; Empagliflozin (BI 10773); UNII-HDC1R2M35U; VA10802; AJ93046; BI10773; BI-10773; BI 10773; Empagliflozin; trade name: Jardiance
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 5 mg/mL (11.09 mM) in 0.5%HPMC (这些助溶剂从左到右依次添加,逐一添加), 悬浮液;超声助溶。
配方 2 中的溶解度: ≥ 2.87 mg/mL (6.36 mM) (饱和度未知) in 5% DMSO + 40% PEG300 + 5% Tween80 + 50% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.87 mg/mL (6.36 mM) (饱和度未知) in 5% DMSO + 95% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: ≥ 2.08 mg/mL (4.61 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将100 μL 20.8 mg/mL澄清的DMSO储备液加入400 μL PEG300中,混匀;再向上述溶液中加入50 μL Tween-80,混匀;然后加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 5 中的溶解度: ≥ 2.08 mg/mL (4.61 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将100μL 20.8mg/mL澄清的DMSO储备液加入到900μL 20%SBE-β-CD生理盐水中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 配方 6 中的溶解度: ≥ 2.08 mg/mL (4.61 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 20.8 mg/mL 澄清 DMSO 储备液加入到 900 μL 玉米油中并混合均匀。 配方 7 中的溶解度: 15% Captisol: 15 mg/mL 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.2177 mL | 11.0887 mL | 22.1774 mL | |
| 5 mM | 0.4435 mL | 2.2177 mL | 4.4355 mL | |
| 10 mM | 0.2218 mL | 1.1089 mL | 2.2177 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT05262764 | Active Recruiting |
Drug: JARDIANCE® | Heart Failure | Boehringer Ingelheim | April 1, 2022 | N/A |
| NCT05350202 | Active Recruiting |
Drug: Empagliflozin | Heart Failure | Boehringer Ingelheim | December 15, 2022 | N/A |
| NCT03437330 | Active Recruiting |
Drug: Empagliflozin (Jardiance®) Drug: Insulin Glargine (Lantus®) |
Type2 Diabetes Mellitus | University Hospital Tuebingen | October 27, 2021 | Phase 4 |
| NCT03363464 | Active Recruiting |
Drug: Empagliflozin Drug: DPP-4 inhibitor |
Diabetes Mellitus, Type 2 | Boehringer Ingelheim | October 16, 2017 | N/A |
| NCT03193684 | Active Recruiting |
Drug: Empagliflozin 25 MG Drug: Control |
Hepatic Glucose Metabolism | The University of Texas Health Science Center at San Antonio |
May 20, 2018 | Phase 4 |