| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| Other Sizes |
|
| 靶点 |
DNA synthesis; STAT1
|
||
|---|---|---|---|
| 体外研究 (In Vitro) |
体外活性:氟达拉滨有效抑制 RPMI 8226 细胞的增殖,IC50 为 1.54 μg/mL。 Fludarabine 对 MM.1S 和 MM.1R 细胞的 IC50 分别为 13.48 μg/mL 和 33.79 μg/mL。相比之下,U266 细胞对氟达拉滨具有耐药性,IC50 为 222.2 μg/mL。氟达拉滨治疗导致细胞周期 G1 期细胞数量增加,同时细胞周期 S 期细胞数量以时间依赖性方式减少。氟达拉滨诱导细胞周期阻滞并引发 MM 细胞凋亡。 Fludarabine 触发 caspase-8、-9 和 -3、-7 的时间依赖性裂解,然后是 PARP 裂解。氟达拉滨以时间依赖性方式增加 Bax 的表达,而 Bak 的表达不改变。暴露于氟达拉滨 12 小时后,RPMI 8226 细胞表现出膜电位损失,其中 61.05% 的细胞表达罗丹明 123 的低荧光,而未经处理的对照细胞中只有 8.62% 的细胞表达低荧光。为了提高溶解度,氟达拉滨被配制为单磷酸盐(F-ara-AMP,福达拉滨),在静脉输注后立即定量地去磷酸化为母体核苷。细胞内部发生再磷酸化,生成氟腺嘌呤阿糖苷三磷酸 (F-ara-ATP),它是 F-ara-A 的主要细胞毒性代谢物。氟达拉滨还可以诱导单核细胞的促炎刺激,通过 ICAM-1 表达增加和 IL-8 释放来评估。氟达拉滨不影响卵巢癌细胞系的生长,但它会显着且剂量依赖性地抑制黑色素瘤细胞系的增殖。细胞测定:用氟达拉滨或对照、地塞米松敏感 (MM.1S) 和耐药 (MM.1R) 人 MM 细胞系、RPMI8226 和 U266 细胞系(5 × 105 个细胞)处理后,在磷酸盐缓冲盐水中洗涤两次(PBS) 并用 70% 冰冷乙醇固定,然后离心并悬浮于含有 100 μg/mL RNase A 的 PBS 中。37 ℃ 孵育 30 分钟后,将样品重悬于 25 μg/mL 碘化丙啶中。流式细胞术在 FACSCalibur 自动化系统上进行。根据制造商的说明,通过Annexin V-FITC细胞凋亡检测试剂盒测定细胞凋亡。对于 TUNEL(末端脱氧核苷酸转移酶介导的脱氧尿苷三磷酸缺口末端标记)测定,使用原位细胞死亡检测试剂盒通过流式细胞术分析细胞。
|
||
| 体内研究 (In Vivo) |
用 PBS 处理的肿瘤在 25 天内迅速生长至其初始体积的约 10 倍,而在 40 mg/kg 的氟达拉滨中,肿瘤的增长不到 5 倍。 40 mg/kg Fludarabine 对 RPMI8226 肿瘤生长具有显着的抗肿瘤作用。第 10 天用 40 mg/kg 氟达拉滨治疗的 RPMI8226 肿瘤细胞凋亡细胞增加。 Fludarabine 可有效抑制 SCID 小鼠中的 RPMI8226 骨髓瘤异种移植物。[1]
|
||
| 酶活实验 |
氟达拉滨是一种核苷类似物,由于其对淋巴细胞的强细胞毒性活性,已成功用于治疗低级别淋巴细胞恶性肿瘤,最近也用于干细胞移植的非清髓性预备方案。在本文中,我们发现氟达拉滨也可以诱导单核细胞的促炎刺激,通过增加ICAM-1的表达和IL-8的释放来评估。为了研究其中的机制,我们使用了MAPK和NF-kappaB途径的选择性抑制剂,这两种途径都与ICAM-1和IL-8的调节有关。我们的研究结果表明氟达拉滨的作用是通过激活ERK介导的,并且不依赖于p38、JNK或NF-kappaB途径。通过Western blotting分析,我们证实了氟达拉滨诱导ERK的快速激活,持续至少30分钟。此外,氟达拉滨对单核细胞的促炎激活在很大程度上被自由基清除剂n -乙酰半胱氨酸共同给予减弱,这表明活性氧参与了氟达拉滨的作用。最后,我们发现氟达拉滨不仅在单核细胞中,而且在慢性淋巴细胞白血病的非增殖淋巴细胞中诱导转录因子AP-1的激活。体内氟达拉滨的一些副作用可能归因于细胞活化/分化,而不是诱导细胞凋亡。[3]
|
||
| 细胞实验 |
氟达拉滨或对照处理的人 MM 细胞系 RPMI8226 和 U266(5 × 105 细胞)对地塞米松敏感 (MM.1S) 和耐药 (MM.1R),并用70% 冰冷乙醇,离心,悬浮于含有 100 μg/mL RNase A 的 PBS 中。37 ℃ 孵育 30 分钟后,在 25 μg/mL 碘化丙啶中进行采样。 FACSCalibur 自动化系统用于进行流式细胞术。按照制造商的说明,使用膜联蛋白 V-FITC 细胞凋亡检测试剂盒来鉴定细胞凋亡。原位细胞死亡检测试剂盒辅助流式细胞术用于分析细胞,进行 TUNEL(末端脱氧核苷酸转移酶介导的脱氧尿苷三磷酸缺口末端标记)测定。
|
||
| 动物实验 |
|
||
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Bioavailability is 55% following oral administration. 117-145 mL/min [patients with B-cell CLL receiving IV administration of a single dose of 40 mg/m^2. ... To compare the pharmacokinetics of sc & iv fludarabine in patients with lupus nephritis. ... Open-label, randomized, crossover trial conducted with a phase I-II trial. ... Government research hospital. ... Five patients with lupus nephritis. ... Fludarabine 30 mg/m2/day was administered either sc or as a 0.5-hr iv infusion for 3 consecutive days. All patients received oral cyclophosphamide 0.5 g/m2 on the first day of each cycle. ... Plasma samples were collected before & 0.5, 1, 1.5, 2, 4, 8, & 24 hrs after the first dose. Urine was collected at 6-hr intervals for 24 hrs. Plasma & urine were analyzed for fluoro-arabinofuranosyladenine (F-ara-A), fludarabine's main metabolite, using high-performance liquid chromatography. Compartmental techniques were used to determine the pharmacokinetics of F-ara-A; a linear two-compartment model best described them. Comparison of the pharmacokinetics between sc & iv admin was done by using a Wilcoxon signed rank test. No significant differences were found between sc & iv admin in median (interquartile range) maximum concns of 0.51 (0.38-0.56) & 0.75 (0.52-0.91) mg/L, respectively, or in fitted area under the concn-time curves from 0-24 hrs of 4.65 (4.17-4.98) & 4.55 (3.5-4.94) mg x hr/L, respectively. Bioavailability of F-ara-A after sc dosing was approx 105% of the bioavailability after iv admin. Differences in renal clearance & % of dose excreted in urine for sc & iv admin were nonsignificant. No injection site reactions were seen with subcutaneous dosing. ... Sc & iv admin of fludarabine appear to have similar pharmacokinetics in patients with lupus nephritis. Sc injection may offer a convenient alternative to iv admin. Biological Half-Life 20 hours |
||
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
In clinical trials, serum enzymes elevations occurred in only a small proportion of patients treated with fludarabine for leukemia. The role of fludarabine as opposed to other antineoplastics used in antileukemic regimens was not always clear from these studies. Cases of clinically apparent liver injury due to fludarabine have been reported to occur, but few details were available and most patients were receiving other cancer chemotherapeutic agents. Fludarabine is immunosuppressive and decreases total white blood cell counts and specifically lymphocyte counts and CD8 T cells. As a consequence, fludarabine therapy has been linked to cases of reactivation of chronic hepatitis B, including instances of reverse seroconversion marked by development of HBsAg and active disease in a patient who had resolved hepatitis B before chemotherapy, as shown by presence of anti-HBc without HBsAg. Reactivation typically occurs after 3 to 6 courses of anticancer mediations and most commonly 2 to 4 months after completing chemotherapy. The frequency and severity of reactivation after fludarabine therapy has led to recommendations that patients be screened for HBsAg and anti-HBc before treatment, and give prophylaxis with antiviral therapy using an oral nucleoside with potent activity against HBV, such as lamivudine, tenofovir or entecavir. If prophylaxis is not used, careful monitoring and early institution of antiviral therapy is warranted. Fludarabine has also been associated with development of opportunistic infections including herpes virus and adenovirus infection of the liver. Likelihood score: E* (Unproven but suspected cause of clinically apparent liver injury). Protein Binding 19-29% Interactions Fludarabine may raise the concentration of blood uric acid as part of a tumor lysis syndrome; dosage adjustment of antigout agents /allopurinol, colchicine, probenecid, sulfinpyrazone/ may be necessary to control hyperuricemia and gout; allopurinol may be preferred to prevent or reverse fludarabine-induced hyperuricemia because of risk of uric acid nephropathy with uricosuric antigout agents. Leukopenic and/or thrombocytopenic effects of fludarabine may be increased with concurrent or recent therapy if these medications /blood dyscrasia causing medications/ cause the same effects; dosage adjustment of fludarabine, if necessary, should be based on blood counts. Additive bone marrow depression may occur; dosage reduction may be required when two or more bone marrow depressants, including radiation, are used concurrently or consecutively. Concurrent use with fludarabine is not recommended because of a possible increased risk of fatal pulmonary toxicity. /Pentostatin/ For more Interactions (Complete) data for FLUDARABINE (10 total), please visit the HSDB record page. |
||
| 参考文献 | |||
| 其他信息 |
Therapeutic Uses
Fludarabine is indicated for treatment of patients with B-cell chronic lymphocytic leukemia (CLL) who have not responded to or whose disease has progressed during treatment with at least one standard alkylating agent-containing regimen. /Included in US product labeling/ Fludarabine is indicated for treatment of non-Hodgkin's lymphomas. /NOT included in US product labeling/ Fludarabine phosphate is a purine analogue now commonly used in the treatment of low-grade lymphoid malignancies. A study update to assess long-term survival following fludarabine salvage treatment in previously treated patients with chronic lymphocytic lymphoma (CLL). ... From September 1992 to December 1995, 74 patients with advanced, relapsing B-cell CLL were enrolled in the study. Fludarabine was given for 5 consecutive days at the dose of 25 mg/sq m/day in a 30 min infusion. Treatment was repeated every 28 days for a max of 6 courses. ... Nineteen (26%) patients achieved a complete response (CR) & 20 (27%) patients had a partial response (PR), giving an overall response rate of 53%. The median overall survival was 68 months, & there was a strong negative correlation with the number of previous treatments. The median time to progression was 18 months for patients who achieved a CR & 12 months for those with a PR. ... The results obtained with fludarabine alone in this subset of CLL patients indicate the existence of a conspicuous disease-free survival period. This time window could be used to consolidate the initial response with either biological approaches or high-dose therapeutic strategies such as autologous bone marrow transplantation, with the aim of eventual eradication of the disease. Drug Warnings FLUDARA FOR INJECTION should be administered under the supervision of a qualified physician experienced in the use of antineoplastic therapy. FLUDARA FOR INJECTION can severely suppress bone marrow function. When used at high doses in dose-ranging studies in patients with acute leukemia, FLUDARA FOR INJECTION was associated with severe neurologic effects, including blindness, coma, and death. This severe central nervous system toxicity occurred in 36% of patients treated with doses approximately four times greater (96 mg/sq m/day for 5-7 days) than the recommended dose. Similar severe central nervous system toxicity, including coma, seizures, agitation and confusion, has been reported in patients treated at doses in the range of the dose recommended for chronic lymphocytic leukemia. Instances of life-threatening and sometimes fatal autoimmune phenomena such as hemolytic anemia, autoimmune thrombocytopenia/thrombocytopenic purpura (ITP), Evan's syndrome, and acquired hemophilia have been reported to occur after one or more cycles of treatment with FLUDARA FOR INJECTION. Patients undergoing treatment with FLUDARA FOR INJECTION should be evaluated and closely monitored for hemolysis. In a clinical investigation using FLUDARA FOR INJECTION in combination with pentostatin (deoxycoformycin) for the treatment of refractory chronic lymphocytic leukemia (CLL), there was an unacceptably high incidence of fatal pulmonary toxicity. Therefore, the use of FLUDARA FOR INJECTION in combination with pentostatin is not recommended. The bone marrow depressant effects of fludarabine may result in an increased incidence of microbial infection, delayed healing, & gingival bleeding. Dental work, whenever possible, should be completed prior to initiation of therapy or deferred until blood counts have returned to normal. Patients should be instructed in proper oral hygiene during treatment, including caution in use of regular toothbrushes, dental floss, & toothpicks. Fludarabine also sometimes causes stomatitis associated with considerable discomfort. For more Drug Warnings (Complete) data for FLUDARABINE (26 total), please visit the HSDB record page. Pharmacodynamics Fludarabine is a chemotherapy drug used in the treatment of chronic lymphocytic leukemia. It acts at DNA polymerase alpha, ribonucleotide reductase and DNA primase, results in the inhibition of DNA synthesis, and destroys the cancer cells. |
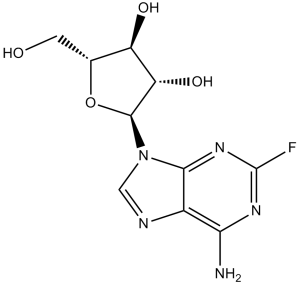
| 分子式 |
C10H12FN5O4
|
|
|---|---|---|
| 分子量 |
285.23
|
|
| 精确质量 |
285.087
|
|
| 元素分析 |
C, 42.11; H, 4.24; F, 6.66; N, 24.55; O, 22.44
|
|
| CAS号 |
21679-14-1
|
|
| 相关CAS号 |
|
|
| PubChem CID |
657237
|
|
| 外观&性状 |
White to yellow solid powder
|
|
| 密度 |
2.2±0.1 g/cm3
|
|
| 沸点 |
747.3±70.0 °C at 760 mmHg
|
|
| 熔点 |
265-268ºC
|
|
| 闪点 |
405.8±35.7 °C
|
|
| 蒸汽压 |
0.0±2.6 mmHg at 25°C
|
|
| 折射率 |
1.876
|
|
| LogP |
-0.4
|
|
| tPSA |
139.54
|
|
| 氢键供体(HBD)数目 |
4
|
|
| 氢键受体(HBA)数目 |
9
|
|
| 可旋转键数目(RBC) |
2
|
|
| 重原子数目 |
20
|
|
| 分子复杂度/Complexity |
367
|
|
| 定义原子立体中心数目 |
4
|
|
| SMILES |
FC1=NC(=C2C(=N1)N(C([H])=N2)[C@@]1([H])[C@]([H])([C@@]([H])([C@@]([H])(C([H])([H])O[H])O1)O[H])O[H])N([H])[H]
|
|
| InChi Key |
HBUBKKRHXORPQB-FJFJXFQQSA-N
|
|
| InChi Code |
InChI=1S/C10H12FN5O4/c11-10-14-7(12)4-8(15-10)16(2-13-4)9-6(19)5(18)3(1-17)20-9/h2-3,5-6,9,17-19H,1H2,(H2,12,14,15)/t3-,5-,6+,9-/m1/s1
|
|
| 化学名 |
(2R,3S,4S,5R)-2-(6-amino-2-fluoropurin-9-yl)-5-(hydroxymethyl)oxolane-3,4-diol
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (8.76 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (8.76 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (8.76 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: 30% propylene glycol, 5% Tween 80, 65% D5W: 30 mg/mL 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 3.5059 mL | 17.5297 mL | 35.0594 mL | |
| 5 mM | 0.7012 mL | 3.5059 mL | 7.0119 mL | |
| 10 mM | 0.3506 mL | 1.7530 mL | 3.5059 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Cord Blood Transplant in Children and Young Adults With Blood Cancers and Non-malignant Disorders
CTID: NCT04644016
Phase: Phase 2 Status: Recruiting
Date: 2024-12-02
 |
 |