| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| Other Sizes |
|
| 靶点 |
PPARγ; PPARα; UCP1; SOD; iNOS; Caspase 3/8/9;ERK2
|
|---|---|
| 体外研究 (In Vitro) |
本研究探讨了海洋类胡萝卜素Fucoxanthin/岩藻毒素对结核分枝杆菌(Mtb)临床分离株的抗结核特性。选择参与Mtb细胞壁生物合成的两种重要酶,UDP吡喃半乳糖变位酶(UGM)和芳胺-N-乙酰基转移酶(TBNAT)作为药物靶点,以揭示岩藻毒素抗结核作用的机制。所得结果表明,与标准药物异烟肼(INH)相比,岩藻毒素对所有测试的结核分枝杆菌菌株均显示出明显的抑菌作用,最低抑菌浓度(MIC)范围为2.8至4.1µM,基于细胞毒性评估,选择性指数良好(范围为6.1至8.9)。岩藻毒素和标准尿苷-5'-二磷酸对UGM的强效抑制作用分别为98.2%和99.2%。岩藻毒素能有效灭活TBNAT(半数最大抑制浓度(IC50)=4.8µM;99.1%的抑制率)与INH相比(IC50=5.9µM;97.4%的抑制)。此外,还实现了分子对接方法,以认可和合理化生物学发现,并设想结构-活性关系。由于过去十年的临床证据证实了细菌感染与自身免疫性疾病之间的相关性,在这项研究中,我们根据之前的临床观察和动物研究讨论了结核分枝杆菌感染与自身抗体疾病之间的联系。总之,我们提出,岩藻毒素通过抑菌作用作用于多个靶点以及抑制UGM和TBNAT,对治疗结核病具有巨大的治疗价值。这些结果可能导致避免或降低遗传易感宿主对与结核分枝杆菌感染相关的自身免疫性疾病的易感性。[1]
Fucoxanthin/岩藻毒素IC50分别为1445和1641µM(Hela和SiHa细胞)。芯片结果显示,与未处理的SiHa细胞相比,岩藻毒素处理的SiHa细胞中有2255个DEGs,包括943个上调基因和1312个下调基因。疾病和功能分析表明,这些DEG主要与癌症和组织损伤和异常有关,在线综合通路分析表明,DEG主要富集p53信号传导。HIST1H3D在岩藻毒素的作用下显著下调。抑制HIST1H3D mRNA显著降低了细胞增殖和集落形成,显著增加了凋亡的HeLa和SiHa细胞的百分比,细胞被阻滞在G0/G1细胞周期期。 结论:HIST1H3D可能是宫颈癌发生过程中的癌基因,也是治疗宫颈癌症的一个潜在的岩藻红靶点。[2] Fucoxanthin是一种从褐藻中提取的天然类胡萝卜素,它抑制了人类神经母细胞瘤细胞系GOTO细胞的生长。在药物治疗后第3天,10微克/毫升的岩藻黄素将GOTO细胞的生长率降低到对照组的38%。流式细胞术分析显示,岩藻毒素导致细胞周期阻滞在G0-G1期。在10微克/毫升的浓度下处理4小时后,岩藻毒素就证明N-myc基因的表达降低,这可能对类胡萝卜素的抗增殖作用机制很重要[3]。 |
| 体内研究 (In Vivo) |
本研究旨在探讨岩藻黄素/Fucoxanthin对内毒素诱导的大鼠葡萄膜炎(EIU)的疗效。研究了岩藻毒素对内毒素诱导的白细胞和蛋白质浸润、大鼠房水中一氧化氮(NO)、前列腺素(PG)-E2和肿瘤坏死因子(TNF)-α浓度的影响,以及对小鼠巨噬细胞系(RAW 264.7细胞)中环氧化酶(COX)-2和诱导型一氧化氮合酶(iNOS)蛋白表达的影响。通过足垫注射脂多糖(LPS)在雄性Lewis大鼠中诱导EIU。注射LPS后,立即静脉注射0.1、1或10mg(-1)的岩藻毒素。24小时后从双眼收集房水,并测量渗入房水的细胞数量和房水蛋白质浓度。通过酶联免疫吸附试验测定PGE2、NO和TNF-α的水平。RAW 264.7细胞用不同浓度的岩藻毒素预处理24小时,随后用LPS孵育24小时。通过Western印迹法分析COX-2和iNOS蛋白的表达。测定PGE2、NO和TNF-α的产生水平。Fucoxanthin以剂量依赖的方式抑制EIU的发展。用岩藻毒素治疗导致房水中PGE2、NO和TNF-α浓度降低。与LPS组相比,岩藻毒素处理的RAW264.7细胞中COX和iNOS蛋白的表达显著降低。它还显著降低了细胞培养基中PGE2、NO和TNF-α的产生浓度。目前的结果表明,岩藻毒素通过阻断iNOS和COX-2蛋白的表达来抑制EIU的炎症,其对眼睛的抗炎作用与类似剂量的泼尼松龙的作用相当。[8]
肾脏镉水平变化[9] 为了评估镉暴露对肾功能的影响,我们首先检测了未服用CdCl2的对照组肾脏中的基本镉水平。对照组的结果仅为5.28±0.45 ng/mL(修订后的表2)。CdCl2治疗,但没有岩藻黄素作为阴性对照组(NCG),显著增加了肾脏镉水平(P<0.05)。与NCG和10(F1)mg/kg bw/天岩藻毒素治疗组相比,以参复康片作为阳性对照的治疗大大降低了肾镉水平(P<0.05)。相比之下,25(F2)和50(F3)mg/kg bw/天的岩藻毒素处理阻断了镉诱导的镉水平升高(与NCG相比,P<0.05),而F2和F3组的肾镉水平明显低于PCG(P<0.05)。这些结果表明,以25或50 mg/kg bw/天的剂量补充岩藻毒素可促进肾脏镉代谢,对镉积累的改善效果优于参复康片。 肾损伤标志物水平的变化[9] 为了探索这些生理变化的分子机制,我们研究了肾损伤相关的生物标志物(修订后的表3)。结果显示,CdCl2处理组(NCG)的血浆BUN、KIM-1和NGAL水平显著高于未处理CdCl2的对照组(P<0.05)。与NCG相比,参复康片(PCG)、25(F2)和50(F3)mg/kg bw/天的岩藻黄素显著降低了BUN水平(P<0.05)。F2组、F3组和PCG组的BUN水平与对照组相比没有显著差异(P>0.05)。与NCG相比,参复康片和岩藻毒素治疗显著降低了KIM-1水平(P<0.05)。F2组的KIM-1水平与对照组没有显著差异(P>0.05),表明补充25mg/kg bw/天的岩藻毒素可以将KIM-1水平降至正常值。与NCG组相比,参复康片和岩藻毒素治疗显著降低了NGAL水平(P<0.05)。PCG组NGAL水平与对照组无显著差异(P>0.05),表明补充参复康片可以将NGAL水平降至正常值。 岩藻黄素对CdCl2处理过的胶束中抗氧化剂的影响[9] 为了评估岩藻黄素在抗氧化应激中的作用,我们检测了脂质过氧化途径中的一些关键酶水平。与对照组相比,NCG小鼠肾脏POD、SOD、CAT和APX的活性显著降低(P<0.05)。和NCG小鼠相比,岩藻黄素和参复康片治疗显著改善了氧化还原状态。与对照组相比,用中等(F2)和高(F3)浓度的岩藻毒素给药的小鼠POD、SOD、CAT和APX活性显著提高。PCG和NCG的肾CAT和APX活性没有显著差异(P>0.05)。在F2和F3组中,肾脏CAT活性显著高于NCG(P<0.05),与对照组相比没有显著差异(P>0.05)。F2和F3组的肾APX活性显著高于NCG(P<0.05),但在F3组,与对照组相比没有显著差异(P>0.05),表明25和50 mg/kg bw/天的岩藻毒素治疗在增加CAT和APX活性方面比参复康片效果更好(图6)。 |
| 酶活实验 |
UGM活性[4]
UGM活动已按照之前的规定完成岩藻黄素和标准UGM抑制剂尿苷-5'-二磷酸在DMSO中制备(所有进行的反应均使用2%(v/v)的DMSO)。简而言之,在缓冲液(100 mM 3-(N-吗啉代)丙磺酸(MOPS))中制备的UGM(25µg/mL);pH=8.0)与Na2S2O3(20 mM)在冰上预孵育1分钟。此外,将溶液混合物与测试抑制剂(20 mmol)孵育,然后在25°C下加入底物UDP-Galf(60µM)。随后,通过加入冰冷的HCl在不同时间停止反应,并直接在液氮中快速冷冻。UGM在2%(v/v)DMSO存在下的活性被视为对照。采用高效液相色谱(HPLC)系统监测UGM活性,根据详细程序跟踪所有仪器设置和操作要求。通过比较底物和产物峰的积分来测量转化程度。 TBNAT活性[4] 对基于微孔板光度计的测定方法进行了轻微的改进,以确定TBNAT催化的反应。通过用5,5′-二硫代双(2-硝基苯甲酸)(DTNB)检测乙酰辅酶A(AcCoA)的水解速率来检测TBNAT活性,并在405nm处记录吸光度。总之,制备了测试分子(岩藻黄素和标准INH)并将其溶解在DMSO中,所有反应都在DMSO(2%;v/v)的存在下进行。TBNAT(170 ng;在20 mM Tris-HCl(pH=8)中制备,与二硫苏糖醇(1 mM)和5%甘油混合)在25°C下与测试化合物(5µL,终浓度范围为10至20µM)一起孵育15分钟。此外,将15µL底物肼屈嗪(30µM)和12µL乙酰辅酶a(30µM)与获得的混合溶液混合。随后,在25°C下10分钟后,使用25µL DTNB(在pH=7.3的盐酸胍(6.4 M)和Tris-HCl(100 mM)中处理)停止反应,并将酶活性作为终点读数分析。TBNAT催化的反应(无抑制)被指定为对照。抑制百分比被确定为酶活性(表示为与测试分子形成辅酶A的速率)与没有抑制的对照活性的比率。通过非线性拟合抑制剂的抑制百分比和对数浓度与反应得到的抑制曲线用于评估IC50值。 |
| 细胞实验 |
最低抑菌浓度(MIC)评估[4]
如CLSI指南中所述,通过微量稀释法评估了岩藻黄质和INH的最小抑制浓度。阴性对照被指定为二甲亚砜(DMSO)和肉汤。在这里,使用1%的DMSO溶解和稀释测试化合物,并进一步与肉汤混合(25µL DMSO溶液在5mL肉汤中)。使用1%的DMSO对Mtb的生长没有影响。孔中受试物质的最终浓度范围为2.8至6.2µM。孵育24小时后,记录结果并表示为微摩尔尺度的最小抑菌浓度(MIC),该浓度阻碍了蓝色到粉红色的颜色变化。 细胞毒性分析[4] 细胞系和培养要求[4] 正常人胎儿肺成纤维细胞在37°C下,在添加了10%胎牛血清、2 mM L-谷氨酰胺溶液和1%非必需氨基酸溶液的最低必需鹰培养基MEM中,在5%CO2的加湿状态下培养。随后,在37°C下用胰蛋白酶/EDTA处理后收集细胞进行传代培养。 细胞毒性评估[4] 使用CellTiter-96测定法评估了岩藻黄素和INH的潜在细胞毒性。该测定基于活细胞中四唑染料MTS还原为甲氮,然后按照迄今为止报道的程序进行比色测定。用测试化合物处理的MRC-5细胞作为研究组,而未处理的MRC-3细胞作为对照组。在490nm处检测测试样品的吸光度,并使用孵育浓度与相对于未处理对照的吸光度百分比绘制每种化合物的抑制曲线。通过抑制曲线的非线性回归分析确定半最大抑制浓度(IC50)。PRISM软件辅助统计分析。 |
| 动物实验 |
Animals groups and EIU [8]
Eight-week-old male Lewis rats were used. The rats weighed about 250 g. EIU was induced by injection into one footpad of 200 μg of LPS from Salmonella typhimurium that had been diluted in 0.2 ml of saline. The rats were injected intravenously with 0.1, 1 or 10 mg kg−1 Fucoxanthin or 10 mg kg−1 prednisolone in a 0.1% dimethyl sulfoxide solution (Sigma, St. Louis, MO) mixed with 0.1 ml phosphate-buffered saline (PBS). Fucoxanthin was isolated from brown algae using a previously published method (Britton, 1995). Fucoxanthin was administered three times; simultaneously and 30 min before and after the LPS injection. For the LPS group, 0.1% dimethyl sulfoxide of PBS was administered intravenously using the same schedule for the fucoxanthin-administered group. In the control group, neither LPS nor fucoxanthin was injected into the rats. Experimental Design [9] Total animals (N = 120) were randomly divided into two groups of equal average body weight. The mice of the control group (N = 20) were given pure water only, whereas the animals of the cadmium exposure group (N = 100) were given CdCl2 orally at a dose of 30 milligram (mg)/kilogram (kg) body weight (bw)/day for 30 days. In this study, Fucoxanthin was administered at 10, 25 and 50 mg/kg bw/day. To evaluate ameliorative effects of fucoxanthin on the kidney, the cadmium exposure group was divided into the following five subgroups: without fucoxanthin treatment as a negative control group (NCG, N = 20); positive control group (PCG, N = 20) was mice received Shenfukang tablets orally at a dose of 50 mg/kg bw/day for 14 days; low (F1), medium (F2), and high (F3) fucoxanthin concentration treated mice (N = 20 mice at each group) were received fucoxanthin orally at a dose of 10, 25, and 50 mg/kg bw/day for 14 days, respectively. Animal Sacrifice and Sample Collection [9] After the 14-day Fucoxanthin treatment, mice were sacrificed. Kidney tissues and peripheral blood samples were collected directly. In each group, kidney samples of 14 mice were subsequently kept at −80°C in ultra cold storage freezer for analyses of cadmium concentration, antioxidant activity and relative gene expression; 3 mice were kept at 4°C in 10% neutral-buffered formalin for microscopic observation; and 3 mice were kept at 4°C in 2.5% neutral-buffered glutaraldehyde for electron microscope observation. As for the blood samples, they were added to the test tubes with anticoagulant, centrifuged for 5 minutes at a speed of 1372 g, and the upper plasma was collected for analysis of kidney damage. |
| 参考文献 |
|
| 其他信息 |
Fucoxanthin is an epoxycarotenol that is found in brown seaweed and which exhibits anti-cancer, anti-diabetic, anti-oxidative and neuroprotective properties. It has a role as an algal metabolite, a CFTR potentiator, a food antioxidant, a neuroprotective agent, a hypoglycemic agent, an apoptosis inhibitor, a hepatoprotective agent, a marine metabolite and a plant metabolite. It is an epoxycarotenol, an acetate ester, a secondary alcohol, a tertiary alcohol and a member of allenes.
Fucoxanthin is under investigation in clinical trial NCT03613740 (Effect of Fucoxanthin on the Components of the Metabolic Syndrome, Insulin Sensitivity and Insulin Secretion). Fucoxanthin isis a marine carotenoid mainly found in brown algae, giving them a brown or olive-green color. Fucoxanthin is investigated for its anti-inflammatory, antinociceptive and anti-cancer effects. In vivo studies have demonstrated that oral administration of fucoxanthin inhibited carcinogenesis in an animal model of duodenal, skin, colon and liver cancer. Fucoxanthin causes antitumor and anticarcinogenic effects by inducing G1 cell-cycle arrest and apoptosis by modulating expression of various cellular molecules and cellular signal transduction pathways, but the exact mechanism of anti-cancer action of fucoxanthin is not fully elucidated. Fucoxanthin regulates lipids metabolism, the effect most likely mediated by AMK-activated protein kinase. A clinical trial of fucoxanthin against non-alcoholic fatty liver disease is ongoing. Fucoxanthin has been reported in Jania, Corbicula sandai, and other organisms with data available. Objective: To investigate the role of fucoxanthin, reported to have significant anticancer effects, and histone Cluster 1 H3 Family Member D (HIST1H3D; implicated in tumorigenesis) in cervical cancer. Methods: The half maximal inhibitory concentration (IC50) of fucoxanthin against HeLa and SiHa cervical cancer cells was determined. Differentially expressed genes (DEGs) in SiHa cells treated with IC50 fucoxanthin were screened by high-throughput techniques and subjected to signal enrichment. Following identification of HIST1H3D as a candidate gene, HIST1H3D-knockdown models were created via transfection with a short hairpin HIST1H3D payload. Impacts on cell proliferation, cell-cycle distribution, colony formation, and apoptosis were studied. Results: The fucoxanthin IC50 was 1 445 and 1 641 µM (Hela and SiHa cells, respectively). Chip results revealed 2 255 DEGs, including 943 upregulated and 1 312 downregulated genes, in fucoxanthin-treated versus untreated SiHa cells. Disease and function analysis indicated that these DEGs are primarily associated with cancer and organismal injuries and abnormalities, and online integrated pathway analysis showed that the DEGs were mainly enriched in p53 signalling. HIST1H3D was significantly downregulated in response to fucoxanthin. Inhibition of HIST1H3D mRNA significantly reduced cell proliferation and colony formation, significantly augmented the percentage of apoptotic HeLa and SiHa cells, and cells were arrested in G0/G1 cell cycle phase.[5] Fucoxanthin, a natural carotenoid prepared from brown algae, inhibited the growth of GOTO cells, a human neuroblastoma cell line. Fucoxanthin at 10 micrograms/ml reduced the growth rate of GOTO cells to 38% of the control at day 3 after drug treatment. Flowcytometric analysis revealed that fucoxanthin caused the arrest in the G0-G1 phase of cell cycle. Expression of N-myc gene was proved to be decreased by fucoxanthin as early as 4 h after treatment at 10 micrograms/ml and that may be important for the mechanism of anti-proliferative action of the carotenoid. [6] Adult T-cell leukemia (ATL) is a fatal malignancy of T lymphocytes caused by human T-cell leukemia virus type 1 (HTLV-1) infection and remains incurable. Carotenoids are a family of natural pigments and have several biological functions. Among carotenoids, fucoxanthin is known to have antitumorigenic activity, but the precise mechanism of action is not elucidated. We evaluated the anti-ATL effects of fucoxanthin and its metabolite, fucoxanthinol. Both carotenoids inhibited cell viability of HTLV-1-infected T-cell lines and ATL cells, and fucoxanthinol was approximately twice more potent than fucoxanthin. In contrast, other carotenoids, beta-carotene and astaxanthin, had mild inhibitory effects on HTLV-1-infected T-cell lines. Importantly, uninfected cell lines and normal peripheral blood mononuclear cells were resistant to fucoxanthin and fucoxanthinol. Both carotenoids induced cell cycle arrest during G(1) phase by reducing the expression of cyclin D1, cyclin D2, CDK4 and CDK6, and inducing the expression of GADD45alpha, and induced apoptosis by reducing the expression of Bcl-2, XIAP, cIAP2 and survivin. The induced apoptosis was associated with activation of caspase-3, -8 and -9. Fucoxanthin and fucoxanthinol also suppressed IkappaBalpha phosphorylation and JunD expression, resulting in inactivation of nuclear factor-kappaB and activator protein-1. Mice with severe combined immunodeficiency harboring tumors induced by inoculation of HTLV-1-infected T cells responded to treatment with fucoxanthinol with suppression of tumor growth, showed extensive tissue distribution of fucoxanthinol, and the presence of therapeutically effective serum concentrations of fucoxanthinol. Our preclinical data suggest that fucoxanthin and fucoxanthinol could be potentially useful therapeutic agents for patients with ATL.[7] Kidney damages caused by cadmium are considered to be one of the most dangerous consequences for the human body. This study aimed to investigate the protective effects of fucoxanthin supplementation on mice models subjected to cadmium-induced kidney damage. The mice treated with cadmium chloride (CdCl2) were observed to have significantly reduced the cross-section area of glomeruli. Cadmium exposure has also caused the damage of the structural integrity of mitochondria and increased blood urea nitrogen (BUN), kidney injury molecule 1 (KIM1), and neutrophil gelatinase associated lipocalin (NGAL) levels. Peroxidase (POD), superoxide dismutase (SOD), catalase (CAT), and ascorbate peroxidase (APX) levels in cadmium-exposed mice were markedly declined. Caspase3, caspase8, and caspase9 gene expressions in association with apoptosis were dramatically elevated in renal tissues. The CdCl2 treated mice were orally administered with 50 mg/kg Shenfukang, 10 mg/kg, 25 mg/kg, and 50 mg/kg fucoxanthin for 14 days. The results revealed that high doses of fucoxanthin administration significantly decreased BUN, KIM1, NGAL levels, increasing POD, SOD, CAT, and ascorbate APX levels. Fucoxanthin administration also promoted recovery of the renal functions, micro-structural organization, and ultra-structural organization in the renal cells. In summary, the ameliorative effects of fucoxanthin supplementation against cadmium-induced kidney damage were mediated via inhibiting oxidative stress and apoptosis, promoting the recovery of structural integrity of mitochondria. [9] |
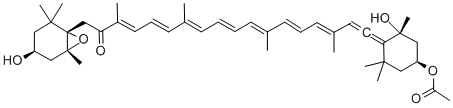
| 分子式 |
C42H58O6
|
|---|---|
| 分子量 |
658.92
|
| 精确质量 |
676.433
|
| 元素分析 |
C, 76.56; H, 8.87; O, 14.57
|
| CAS号 |
3351-86-8
|
| PubChem CID |
5281239
|
| 外观&性状 |
Pink to red solid powder
|
| 密度 |
1.1±0.1 g/cm3
|
| 沸点 |
786.5±60.0 °C at 760 mmHg
|
| 熔点 |
166-168ºC
|
| 闪点 |
228.5±26.4 °C
|
| 蒸汽压 |
0.0±6.2 mmHg at 25°C
|
| 折射率 |
1.563
|
| LogP |
7.7
|
| tPSA |
96.36
|
| 氢键供体(HBD)数目 |
2
|
| 氢键受体(HBA)数目 |
6
|
| 可旋转键数目(RBC) |
12
|
| 重原子数目 |
48
|
| 分子复杂度/Complexity |
1530
|
| 定义原子立体中心数目 |
5
|
| SMILES |
O=C(/C(C)=C/C=C/C(C)=C/C=C/C=C(C)/C=C/C=C(C)/C([H])=[C@@]=C([C@@]1(O)C)C(C)(C[C@H](OC(C)=O)C1)C)C[C@]2(C3(C)C)[C@@](C)(C[C@@H](O)C3)O2
|
| InChi Key |
InChI=1S/C42H58O6/c1-29(18-14-19-31(3)22-23-37-38(6,7)26-35(47-33(5)43)27-40(37,10)46)16-12-13-17-30(2)20-15-21-32(4)36(45)28-42-39(8,9)24-34(44)25-41(42,11)48-42/h12-22,34-35,44,46H,24-28H2,1-11H3/b13-12+,18-14+,20-15+,29-16+,30-17+,31-19+,32-21+/t23?,34-,35-,40+,41+,42-/m0/s1
|
| InChi Code |
InChI=1S/C42H58O6/c1-29(18-14-19-31(3)22-23-37-38(6,7)26-35(47-33(5)43)27-40(37,10)46)16-12-13-17-30(2)20-15-21-32(4)36(45)28-42-39(8,9)24-34(44)25-41(42,11)48-42/h12-22,34-35,44,46H,24-28H2,1-11H3/b13-12+,18-14+,20-15+,29-16+,30-17+,31-19+,32-21+/t23?,34-,35-,40+,41+,42-/m0/s1
|
| 化学名 |
C/C(=C\C=C\C=C(/C)\C=C\C=C(/C)\C(=O)C[C@]12[C@](O1)(C[C@H](CC2(C)C)O)C)/C=C/C=C(\C)/C=C=C3[C@](C[C@H](CC3(C)C)OC(=O)C)(C)O
|
| 别名 |
α-Carotene; 3351-86-8; all-trans-Fucoxanthin; CCRIS 4055; Sebatrol; 06O0TC0VSM; BRN 0073179; CHEBI:5186; Fucoxanthin
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ~12.5 mg/mL (~18.97 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 1.25 mg/mL (1.90 mM) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 悬浮液;超声助溶。
例如,若需制备1 mL的工作液,可将100 μL 12.5mg/mL澄清的DMSO储备液加入到900μL 20%SBE-β-CD生理盐水中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.5176 mL | 7.5882 mL | 15.1763 mL | |
| 5 mM | 0.3035 mL | 1.5176 mL | 3.0353 mL | |
| 10 mM | 0.1518 mL | 0.7588 mL | 1.5176 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT03613740 | Active Recruiting |
Drug: Fucoxanthin Drug: Placebo |
Metabolic Syndrome | University of Guadalajara | September 30, 2019 | Phase 2 |
| NCT02875392 | Completed | Other: placebo pills Other: 275mg Oligo Fucoidan + 275mg HS Fucoxanthin |
Non-alcoholic Fatty Liver Disease | Taipei Medical University WanFang Hospital |
November 2016 | Not Applicable |
| NCT04832412 | Completed | Dietary Supplement: BrainPhyt Dietary Supplement: 100 % Maltodextrin |
Fucoxanthin Cognitive Impairment Neuroprotection |
Microphyt | April 1, 2021 | Not Applicable |