| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| Other Sizes |
|
| 靶点 |
JAK1/Janus-associated kinase 1
|
||
|---|---|---|---|
| 体外研究 (In Vitro) |
体外活性:Itacitinib(也称为 INCB39110)是一种有效的、选择性的、口服生物可利用的 JAK1(Janus 相关激酶 1)抑制剂,对 JAK1 的选择性是 JAK2 的 >20 倍,是 JAK3 和 TYK2 的 >100 倍(IC50)对于 JAK1、2、3 和 TYK2,分别为 2、63、>2000 和 795 nM)。它具有潜在的抗肿瘤活性,目前正处于治疗骨髓纤维化、类风湿性关节炎和斑块状银屑病的二期临床试验中。 Janus 激酶 (JAK) 是由四种酶组成的家族; JAK1、JAK2、JAK3 和酪氨酸激酶 2 (TYK2) 在细胞因子信号转导中至关重要,并且与癌症和炎症性疾病密切相关。激酶测定:Itacitinib 对 JAK1 的选择性是 JAK2 的 >20 倍,是 JAK3 和 TYK2 的 >100 倍(JAK1、2、3 和 TYK2 的 IC50 分别为 2、63、>2000 和 795 nM)。
Itacitinib (INCB039110) 是一种有效的选择性 JAK1 抑制剂,对 JAK1 的选择性是 JAK2 的 20 倍以上,是 JAK3 和 TYK2 的 100 倍以上。骨髓纤维化研究采用 itacitinib [1]。
伊塔替尼减少巨噬细胞产生IL-6[3] 最近的证据表明,宿主巨噬细胞是CAR-T细胞治疗后IL-6的主要生产者。因此,我们质疑伊塔替尼是否会阻止宿主巨噬细胞产生IL-6。首先,用粒细胞集落刺激因子在体外扩增小鼠骨髓来源的巨噬细胞,并在第6天将伊塔替尼加入培养物中。在第7天将LPS加入培养物中以激活巨噬细胞。阿替尼的预防性治疗以剂量依赖的方式减少了IL-6的产生,表明阿替尼在减少炎性细胞因子产生方面的活性并非仅限于T细胞(图2A)。我们还观察到其他几种细胞因子(即IL-10、IL-12p70、KC/GRO,补充图S2)的减少趋势并不显著 伊塔替尼减少CAR T细胞因子的产生[3] 尽管宿主免疫系统产生细胞因子是CRS的主要原因,但CAR-T细胞产生炎性细胞因子也是主要原因。在证明伊塔替尼能够减少宿主免疫系统产生炎性细胞因子后,我们接下来想研究伊塔替尼是否能减少CAR T细胞产生炎性因子。在与临床试验中达到的人体剂量相当的托珠单抗或伊塔替尼浓度下扩增人CD19-CAR T细胞。扩增3天后,CAR T细胞与表达CD19的NAMALWA靶细胞共培养,6小时后收集上清液以定量细胞因子。伊塔替尼,而不是托珠单抗,能够显著降低许多炎性细胞因子(即IL-2、IFN-γ、IL-6和IL-8)的水平(图3)。作为内部对照(背景),我们还测量了非转导T细胞产生的细胞因子(图3)。 临床相关浓度的伊塔替尼不影响PBMC增殖[3] 由于T细胞起着重要的抗肿瘤作用,因此研究了伊塔替尼对T细胞的影响,以确定治疗是否可能导致广泛的免疫抑制,从而可能干扰正常的T细胞增殖和功能。T细胞是从健康成年人的新鲜分离的人外周血单个核细胞中获得的。在用抗CD3/抗CD28包被的珠子激活后,T细胞在浓度增加的伊塔替尼存在下扩增,并通过流式细胞术测量增殖。与二甲基亚砜(DMSO)对照组相比,与IC50相关的伊塔替尼浓度(50-100nM)对抗CD3/抗CD28诱导的人T细胞扩增没有显著影响(图4A),表明伊塔替尼治疗对T细胞增殖能力没有负面影响。作为内部控制,与JAK/STAT信号活性的破坏一致,更高浓度的伊塔替尼(1000 nM)阻断了T细胞增殖(图4A)。 伊塔替尼不影响CAR-T细胞增殖[3] 为了研究阿替尼对CAR T细胞扩增和细胞溶解活性的特异性影响,在阿替尼浓度从100 nM增加到500 nM的情况下,用抗CD3/抗CD28包被的珠子扩增GD2-CAR T细胞。再次,与DMSO对照组相比,100-250nM的伊塔替尼对CD3/CD28诱导的GD2-CAR T细胞扩增没有显著影响,而500nM足以阻断CAR T细胞增殖(图4B)。重要的是,在低浓度(100和250 nM)伊塔替尼存在下扩增的GD2-CAR T细胞能够有效裂解表达GD2的肿瘤细胞(图4C)。作为阴性(背景)对照,我们还测量了非转导(非特异性)T细胞的靶细胞裂解。正如预期的那样,GD2-CAR T细胞在高剂量伊塔替尼(500 nM)存在下扩增,无法诱导靶细胞裂解超过背景水平(图4C)。综上所述,这些数据表明,IC50相关剂量的伊塔替尼不会干扰CAR-T细胞增殖或体外抗肿瘤活性。 接下来,我们询问伊塔替尼是否对CAR-T细胞抗原特异性增殖有影响。EGFR-CAR T细胞用抗CD3/CD28珠扩增2周,然后在伊塔替尼或DMSO对照存在下用EGFR珠重新刺激。同样,与IC50相关的伊塔替尼剂量(100或250 nM)不影响CAR-T细胞抗原特异性增殖(图4D)。 伊塔替尼在体外不影响CD19-CAR T细胞溶解活性[3] 为了研究阿替尼对靶向CD19抗原的人CAR T细胞的影响,我们用阿替尼或抗IL-6受体(托珠单抗)处理CD19-CAR T细胞3天,然后测量它们对表达CD19的靶细胞的细胞溶解活性。尽管模拟人类药理活性的托珠单抗浓度显著降低了CAR T细胞的细胞溶解活性,但与对照CAR T细胞相比,100 nM的伊塔替尼没有显示出显著效果(图6A)。用更高剂量的伊塔替尼(300 nM,约为细胞IC50的五倍)扩增的CAR T细胞对抗肿瘤活性显示出适度但具有统计学意义的抑制作用(图6A)。作为内部对照,还测试了未转染的PBMCs的抗肿瘤活性。未转导的T细胞不能特异性裂解靶细胞,并且不受超过背景水平的伊塔替尼或托珠单抗治疗的影响(图6B)。 |
||
| 体内研究 (In Vivo) |
Itacitinib 能够以临床相关剂量抑制小鼠人胰腺异种移植模型中的肿瘤生长,无论是作为单一疗法还是与吉西他滨等细胞毒性药物联合使用。
伊塔替尼/Itacitinib降低急性恶性炎症小鼠模型中的细胞因子水平[3] 由于CRS是与CAR T细胞治疗相关的最常见的副作用,我们研究了伊塔替尼是否能够降低与导致CRS的急性过度活化相关的细胞因子水平。因此,我们进行了实验,用ConA挑战天真动物,ConA是一种强效的T细胞有丝分裂原,能够诱导广泛的炎症细胞因子释放和增殖。与经历CRS的个体相似,接受ConA治疗的动物血清中多种炎性细胞因子水平升高,并出现行为变化,如发烧、不适、低血压、缺氧、毛细血管渗漏、多器官毒性和潜在死亡。为了研究伊塔替尼在该模型中的作用,相应的动物被预防性地给予60或120mg/kg的伊塔替尼来达到与临床试验中观察到的JAK1抑制覆盖率相当的效果。与赋形剂给药动物相比,伊塔替尼能够以剂量依赖的方式显著降低CRS中许多细胞因子(即IL-6、IL-12和IFN-γ)的血清水平(图1A)。正如预期的那样,伊塔替尼对独立于JAK1途径的细胞因子(即IL-5,图1A)没有显著影响。然而,并非所有JAK介导的细胞因子都显著降低(即IL-4,图1A)。此外,在ConA攻击后30分钟给动物服用伊塔替尼的治疗模式中,伊塔替尼也能够剂量依赖性地减少CRS相关的细胞因子(图1B)。 为了证实伊塔替尼/Itacitinib减少恶性炎症的能力,用抗CD3攻击幼稚动物以诱导非特异性T细胞活化和细胞因子反应。同样,相应的动物被预防性或治疗性地给予120mg/kg的伊塔替尼。与载体治疗的小鼠相比,伊塔替尼能够显著降低CRS中许多细胞因子的血清水平,但对独立于JAK1途径的细胞因子没有影响(补充图S1A)[3]。 在确定伊塔替尼能够在体外减少IL-6的产生后,我们接下来将我们的研究扩展到体内环境,以评估伊塔替尼对小鼠活化巨噬细胞的影响。在接受腹腔注射LPS之前,用伊塔替尼或赋形剂对小鼠进行预防性治疗3天,以达到稳定状态。注射后两小时,从腹腔灌洗液中测量细胞因子。如图2B所示,模拟临床试验中JAK1抑制覆盖率的伊塔替尼剂量显著降低了体内活化巨噬细胞的IL-6产生。因此,来自体外和体内系统的数据表明,在实验诱导的CRS模型中,伊塔替尼能够下调炎症性IL-6的主要细胞来源[3]。 伊塔替尼在体内不会损害T细胞抗肿瘤活性[3] 为了进一步测试伊塔替尼对抗原特异性T细胞增殖和体内抗肿瘤活性的影响,我们从OT-1小鼠中分离出脾细胞,OT-1小鼠是针对肽OVA257-264(SIINFEKL)特异性TCR Vα2Vβ5的转基因小鼠(36)。在浓度逐渐增加的伊塔替尼存在下,用SIINFEKL肽扩增OT-1 T细胞,并通过流式细胞术测量其扩增情况。正如预期的那样,与IC50相关的伊塔替尼浓度对扩增速率的影响很小(补充图S3A)。与最大游离浓度相关的伊塔替尼浓度(分别为189和244 nM,在没有或存在强效CYP3A4抑制剂的情况下)诱导了T细胞增殖的适度减少(补充图S3A)。为了评估伊塔替尼对OT-1 CD8体内抗肿瘤疗效的影响,我们进行了将OVA特异性CD8细胞过继转移到先前移植了OVA表达肿瘤细胞系(EG7)的C57BL/6小鼠体内的实验。肿瘤攻击后五天,相应的动物口服赋形剂或60或120mg/kg的伊塔替尼,每日两次,持续两周。肿瘤接种八天后,动物接受了OVA特异性OT-1幼稚CD8细胞的过继转移。与对照组相比,过继转移OT-1 CD8能够显著减少肿瘤生长(图4)。重要的是,与JAK1覆盖目标剂量相当的伊塔替尼剂量不会影响OT-1细胞的抗肿瘤疗效(图5)。 伊塔替尼不影响体内CD19-CAR T细胞的抗肿瘤活性[3] 为了测试伊塔替尼的体内作用,我们研究了口服Itacitinib对CD19-CAR T细胞抗肿瘤作用的影响。用表达CD19+nalm6荧光素酶的人淋巴瘤细胞攻击免疫缺陷小鼠(NSG)。一旦肿瘤被植入(第4天),小鼠接受了3×106个人CD19-CAR T细胞的过继转移。在该模型中,CAR T细胞能够控制肿瘤生长,通过荧光素表达进行测量(图7)。重要的是,动物每日口服依他替尼剂量(120mg/kg)不影响过继转移的CAR T细胞的抗肿瘤活性,因此表明,在靶向剂量下,依他替尼对CAR T细胞抗肿瘤活性没有显著影响。 最后,为了确认伊塔替尼在更具攻击性的模型上不会影响CAR T细胞活性,用5×106 CD19+NAMALWA荧光素酶表达的人淋巴瘤细胞攻击免疫缺陷小鼠(NSG)。一旦肿瘤被植入(第7天),小鼠接受了人CD19-CAR T细胞的过继转移。与接受对照细胞的动物相比,接受CAR T细胞过继转移的动物具有显著的肿瘤生长延迟,这可以通过荧光素表达(补充图S4B)和存活率扩大(P=0.0014)(补充图S46)来衡量。即使在这种侵袭性肿瘤模型中,动物每天口服依他替尼也不会影响过继转移的CAR T细胞的抗肿瘤活性(P=0.1860),从而证实了预防性服用依他替尼来预防CRS的安全性[3]。 联合使用Janus激酶1(JAK1)和JAK2抑制治疗可有效减轻脾肿大和与骨髓纤维化相关的症状负担,但与剂量依赖性贫血和血小板减少症有关。在这项开放标签II期研究中,我们评估了三种剂量水平的强效选择性口服JAK1抑制剂Itacitinib/INCB039110在中度或高危骨髓纤维化患者中的疗效和安全性,血小板计数≥50×109/L。在10、45和32名参加100mg每日两次、200mg每日两次和600mg每日一次队列的患者中,分别有50.0%、64.4%和68.8%完成了第24周。在第12周(主要终点)和第24周,200mg每日两次队列中35.7%和28.6%的患者以及600mg每日一次队列中32.3%和35.5%的患者的总症状评分分别降低了≥50%。相比之下,100 mg每日两次队列中的两名患者(20%)在第12周和第24周的总症状评分降低了≥50%。对于200mg每日两次和600mg每日一次的队列,第12周脾脏体积减少的中位数分别为14.2%和17.4%。此外,在开始治疗前12周内需要输注红细胞的21/39(53.8%)患者在研究第1-24周内输注的红细胞数量减少了≥50%。只有一名患者因3级血小板减少症而停药。非血液学不良事件大多为1级或2级;最常见的是疲劳。INCB039110治疗导致临床上有意义的症状缓解,脾脏体积适度减少,骨髓抑制有限[1]。 |
||
| 酶活实验 |
Janus kinase (JAK)抑制剂(也称为Jakinibs)是一类靶向各种JAK亚型(JAK1、JAK2、JAK3和/或Tyk2)的小药物。它们发挥抗炎特性,部分与促炎M1巨噬细胞激活状态的调节有关。然而,JAK抑制剂对巨噬细胞更广泛激活状态的确切影响仍有待确定,特别是在涉及促炎M1巨噬细胞和促纤维化M2巨噬细胞同时激活的疾病背景下。在自身免疫性肺纤维化如硬皮病相关间质性肺疾病(ILD)中尤其如此,其中M1和M2巨噬细胞起关键的致病作用。在本研究中,我们直接比较了三种JAK抑制剂的抗炎和抗纤维化作用(ruxolitinib (JAK2/1抑制剂);tofacitinib (JAK3/2抑制剂)和itacitinib (JAK1抑制剂)对五种不同激活状态的人单核细胞源性巨噬细胞(MDM)的影响。这三种JAK抑制剂对巨噬细胞具有抗炎作用,这可以通过IFNγ和LPS或单独IFNγ激活的M1巨噬细胞中关键极化标志物(CD86、MHCII、TLR4)的表达下调和关键促炎细胞因子(CXCL10、IL-6和TNFα)的分泌有限来证明。我们还强调,这些JAK抑制剂可以限制由IL-4和IL-13诱导的巨噬细胞的M2a活化,特别是通过下调M2a相关表面标记物CD206和CCL18的分泌来证明。此外,这些JAK抑制剂降低了IL-10和地塞米松(M2c +指数)或单独IL-10 (M2c MDM)诱导的交替活化巨噬细胞中CXCL13、MARCO和SOCS3等标志物的表达。在所有极化态下,Jakinibs对JAK2的抑制作用在1 μM和0.1 μM范围内均达到最高。[2]
激酶生化分析[4] 使用具有重组表位标记激酶结构域(JAK1,837–1142;JAK2,828–1132;JAK3,718–1124;TYK2,873–1187)和肽底物(生物素EQEDEPEGDYFLEX)的均相时间分辨荧光测定法进行酶测定。在测定缓冲液中,在有或没有测试化合物(11点稀释)、JAK酶、500 nM肽、三磷酸腺苷(ATP;1 mM)和2.0%二甲亚砜的情况下进行每种酶反应。50%抑制浓度(IC50)计算为抑制50%荧光信号所需的化合物浓度。使用每种激酶的ATP Km浓度,在标准筛选条件下测试100 nMItacitinib/INCB039110,评估了针对60种非JAK家族激酶的额外活性。与对照值相比,显著抑制被定义为大于或等于30%(重复测定的平均值)。 |
||
| 细胞实验 |
极化标记物的验证和考虑的JAK抑制剂在两种与人血浆水平相关的浓度下各自的毒性[2]
与未受M0刺激的MDM相比,CXCL10、IL-6、IL1Ra和TNFα在IFNγ诱导的M1i MDM和(IFNγ + LPS)诱导的M1Li MDM中均显著过表达(图1A-B)。CCL18、PDGFbb、PPARγ和tenascin C (TenaC)在(IL-4/IL-13)诱导的M2a MDM中与未刺激的M0 MDM相比显著过表达(图1C-D)。在IL-10诱导的M2c MDM和(IL-10/地塞米松)诱导的M2c + Dex中,CXCL13、IL-10、MARCO和SOCS3均上调(图1E)。 T细胞增殖试验[3] 使用Ficoll-Hypaque分离法从人全血样本中制备外周血单核细胞(PBMCs),然后通过离心淘析从PBMCs中获得T细胞。T细胞在RPMI 1640培养基中维持,该培养基补充了10%胎牛血清、1%HEPES、2 mM L-谷氨酰胺、0.05 mM 2-巯基乙醇和100μg/mL链霉素,以及100单位/mL青霉素(完全RPMI或CM)。T细胞用Dynabeads(针对CD3/CD28的固定激动剂抗体)以3:1的比例激活,以0.5×106个细胞/mL的密度重新悬浮在24孔板中,并用不同浓度(50至1000 nM)的Itacitinib/伊塔替尼处理。将平板在37°C的5%CO2气氛中孵育10天,每隔一天通过珠基方法测定增殖情况。每隔一天用新鲜的CM补充培养物。 细胞毒性试验[3] 将表达萤光素酶的SY5Y神经母细胞瘤细胞(GD-2+)以50000个细胞/孔的速度铺在96孔板中。24小时后,将150000个CAR-T细胞加入相应的孔中,最终体积为200μL。平行接种单独的靶细胞,以量化最大萤光素酶表达(相对发光单位;RLUmax)。17小时后,向共培养物中加入100μL荧光素底物。使用EnVision平板阅读器在孵育10分钟后测量发光。细胞裂解百分比通过以下计算获得:[1−(RLU实验)/(RLUmax)]×100。实验一式三份。 单核细胞趋化蛋白(MCP)-1测定[4] 人外周血单个核细胞在37°C、5%CO2下用伊塔替尼预孵育10分钟,并在RPMI培养基中以1.5×106个细胞/ml的速度培养。通过添加30 ng/ml的人重组IL-6刺激孔,并在37°C、5%CO2下孵育48小时。收集上清液,并通过商业ELISA分析人MCP-1的水平。使用GraphPad Prism 5.0软件通过曲线拟合进行ItacitinibIC50测定。 细胞增殖试验[4] 然后从PBMCs中获得人T细胞,并将其保存在含有10%胎牛血清的RPMI中。对于IL-2刺激的细胞增殖分析,首先用10μg/ml的植物血凝素处理细胞3天,以刺激IL-2受体的表达。随后洗涤细胞,以每孔6000个细胞的速度重新悬浮在RPMI培养基中,并在100 U/ml人IL-2的存在下用伊塔替尼处理。将平板在37°C的5%CO2中孵育3天,通过添加CellTiter Glo®试剂并检测发光来确定增殖情况。ItacitinibIC50测定使用GraphPad Prism 5.0软件进行。 IL-17/IL-22细胞因子分析[4] 人外周血单个核细胞在添加10%胎牛血清的RPMI中维持,T细胞用1μg/ml抗CD3和5μg/ml抗CD28抗体激活。2天后,用IL-23(100ng/ml)、IL-2(10ng/ml)和伊塔替尼洗涤细胞并重新培养。细胞在37°C下再孵育4天。ELISA法测定上清液中IL-17和IL-22的浓度。 人磷酸化STAT3(pSTAT3)全血测定[4] 将健康人类志愿者 的血液收集到肝素化管中。血液在37°C下与不同浓度的伊塔替尼一起孵育10分钟。随后,在37°C下用100ng/ml的IL-6刺激细胞15分钟。使用低渗条件裂解红细胞,并通过离心去除上清液。将白细胞制成颗粒并裂解,以制备总细胞提取物。使用商业化的磷酸-STAT3特异性ELISA分析提取物中的pSTAT3。 新出现的证据表明肿瘤相关炎症在胰腺导管腺癌的发生和进展中的重要性。具体来说,炎症相关的IL-6/JAK/STAT3信号通路的组成性激活在胰腺肿瘤中已被报道,并被认为是晚期疾病患者总生存率的不良预后因素。本研究的目的是评估IL-6/JAK/STAT3信号抑制对体外胰腺细胞生长和体内肿瘤生长的影响。INCB039110是一种JAK1选择性抑制剂,目前处于多个2期临床试验中,用于阻断细胞中IL-6/JAK/STAT3信号通路。我们发现,虽然INCB039110抑制IL-6/JAK/STAT3信号通路对传统2D单层细胞培养条件下生长的胰腺细胞系的增殖没有影响,但该抑制剂在3d球形培养系统中对胰腺肿瘤细胞系Hs700T和BxPC-3表现出生长抑制活性。重要的是,在这些细胞中添加刺激JAK/STAT3信号通路的细胞因子可显著促进球状体的生长,而INCB039110可完全逆转这一过程。此外,在联合研究中,JAK1抑制增强了吉西他滨对Hs700T和BxPC-3球体的细胞毒性。另一种新型Jak1选择性抑制剂INCB052793也证实了这一结果,该抑制剂目前正处于晚期恶性肿瘤患者的1期临床试验中。[2] |
||
| 动物实验 |
|
||
| 药代性质 (ADME/PK) |
Pharmacokinetics of itacitinib in mice following multiple oral dosing [4]
The pharmacokinetics of itacitinib in female BALB/c mice was determined following twice daily oral doses at 20, 40, and 80 mg/kg for 12 days (Fig. 4). The mean peak plasma concentration (Cmax) and area under the curve values increased with the dose although not proportionally. Pharmacokinetics studies [4] The oral absorption of itacitinib was determined in commercially purchased female BALB/c mice (BALB/cAnNCrl strain# 028, Charles River Laboratories). Itacitinib was formulated in 0.5% methylcellulose and administered by oral gavage at 20, 40, or 80 mg/kg twice daily for 12 days. Retro-orbital blood samples were collected at 1, 2, 8, and 16 h post-dose on the last day. All blood samples were collected using EDTA as the anticoagulant and centrifuged to obtain plasma samples. Plasma concentrations of itacitinib were determined by liquid chromatography coupled to tandem mass spectrometry using a positive interface on a Sciex API-4000 mass spectrometer and multiple reaction monitoring. The plasma concentration-time data was used to determine the pharmacokinetic parameters by standard non compartmental methods using WinNonlin® version 5.0.1. This article presents the population pharmacokinetic (PopPK) analysis and exposure-response analyses for the primary efficacy end point-acute graft-versus-host disease (aGVHD) day 28 response-and select safety measures (incidence of thrombocytopenia, hypertriglyceridemia, and cytomegalovirus infection) from a phase 3 randomized, double-blind study comparing itacitinib plus corticosteroids versus placebo plus corticosteroids for the treatment of aGVHD. The PopPK data set contained sparse data from patients with aGVHD and select enriched data from healthy volunteers. The structural model was a 2-compartment model with first-order elimination and dose-dependent nonlinear absorption with dual first-order absorption pathways with lag times. Strong cytochrome P450 (CYP) 3A inhibitor coadministration, moderate renal impairment, and participant population (healthy volunteers vs patients with aGVHD) were covariates on apparent clearance. Participant population was also a covariate on apparent intercompartmental clearance and lag time of the secondary absorption compartment. Apparent clearance decreased 42% with coadministration of strong CYP3A inhibitors. Simulations supported the following dose reductions with concomitant use of a strong CYP3A inhibitor: 300 mg once daily to 200 mg once daily, 400 mg once daily to 300 mg once daily, and 600 mg once daily to 400 mg once daily. No dose adjustment is recommended for any other covariate based on the magnitude of impact when they were retained in the model. The exposure-response relationship was characterized between itacitinib exposure and probability of aGVHD day 28 response using a linear logistic regression model. Both itacitinib exposure and aGVHD risk status were significant predictors of response. There was no relationship between itacitinib exposure and thrombocytopenia, hypertriglyceridemia, or cytomegalovirus infection. https://pubmed.ncbi.nlm.nih.gov/36601737/ |
||
| 毒性/毒理 (Toxicokinetics/TK) |
Safety and tolerability [1]
The median (range) exposure to INCB039110 was 102 (23–519) days in the 100 mg twice-daily cohort, 268 (22–535) days in the 200 mg twice-daily cohort, and 197 (58–343) days in the 600 mg once-daily cohort. The most common non-hematologic adverse events regardless of causality are shown in Table 2; most were grade 1 or 2. Grade ≥3 non-hematologic adverse events that occurred in more than one patient were: pneumonia, dyspnea, and hypertension (3 patients each), and congestive heart failure, rectal hemorrhage, asthenia, pyrexia, urinary tract infection, hyperkalemia, increased alkaline phosphatase, and acute renal failure (2 patients each). These 25 events occurred in 18 unique patients. Although infections were common (44.8%), including upper respiratory tract infections in 19.5% of patients (Online Supplementary Table S1), most were mild or moderate, and only four cases (1 each of bronchitis, folliculitis, Herpes simplex, and urinary tract infection) were considered treatment-related by the investigator. All of these four cases were grade 2 and not considered serious, and all resolved without changes to study treatment. Two patients (both in the 600 mg once-daily cohort) died during the study: a 62-year old patient died of pneumonia after approximately 5 months on therapy, and a 61-year old patient died of unspecified causes potentially related to disease progression after slightly less than 4 months on therapy. Both deaths were considered by the investigator to be unrelated to treatment. |
||
| 参考文献 |
|
||
| 其他信息 |
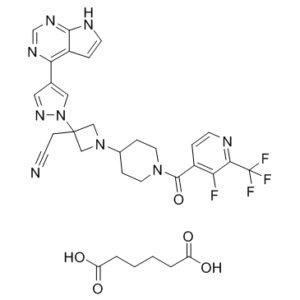
Itacitinib Adipate is the adipate salt form of itacitinib, an orally bioavailable inhibitor of Janus-associated kinase 1 (JAK1) with potential antineoplastic and immunomodulating activities. Upon oral administration, itacitinib selectively inhibits JAK-1, thereby inhibiting the phosphorylation of signal transducer and activator of transcription (STAT) proteins and the production of proinflammatory factors induced by other cytokines, including interleukin-23 (IL-23) and interleukin-6 (IL-6). The JAK-STAT pathway plays a key role in the signaling of many cytokines and growth factors and is involved in cellular proliferation, growth, hematopoiesis, and the immune response; JAK kinases may be upregulated in inflammatory diseases, myeloproliferative disorders, and various malignancies.
Itacitinib has been used in trials studying the treatment of Melanoma, Carcinoma, Metastatic Cancer, Endometrial Cancer, and B-cell Malignancies, among others. Itacitinib is an orally bioavailable inhibitor of Janus-associated kinase 1 (JAK1) with potential antineoplastic and immunomodulating activities. Upon oral administration, itacitinib selectively inhibits JAK-1, thereby inhibiting the phosphorylation of signal transducer and activator of transcription (STAT) proteins and the production of proinflammatory factors induced by other cytokines, including interleukin-23 (IL-23) and interleukin-6 (IL-6). The JAK-STAT pathway plays a key role in the signaling of many cytokines and growth factors and is involved in cellular proliferation, growth, hematopoiesis, and the immune response; JAK kinases may be upregulated in inflammatory diseases, myeloproliferative disorders, and various malignancies. Drug Indication Treatment of acute graft versus host disease. Janus kinase (JAK) inhibitors (also termed Jakinibs) constitute a family of small drugs that target various isoforms of JAKs (JAK1, JAK2, JAK3 and/or tyrosine kinase 2 (Tyk2)). They exert anti-inflammatory properties linked, in part, to the modulation of the activation state of pro-inflammatory M1 macrophages. The exact impact of JAK inhibitors on a wider spectrum of activation states of macrophages is however still to be determined, especially in the context of disorders involving concomitant activation of pro-inflammatory M1 macrophages and profibrotic M2 macrophages. This is especially the case in autoimmune pulmonary fibrosis like scleroderma-associated interstitial lung disease (ILD), in which M1 and M2 macrophages play a key pathogenic role. In this study, we directly compared the anti-inflammatory and anti-fibrotic effects of three JAK inhibitors (ruxolitinib (JAK2/1 inhibitor); tofacitinib (JAK3/2 inhibitor) and itacitinib (JAK1 inhibitor)) on five different activation states of primary human monocyte-derived macrophages (MDM). These three JAK inhibitors exert anti-inflammatory properties towards macrophages, as demonstrated by the down-expression of key polarization markers (CD86, MHCII, TLR4) and the limited secretion of key pro-inflammatory cytokines (CXCL10, IL-6 and TNFα) in M1 macrophages activated by IFNγ and LPS or by IFNγ alone. We also highlighted that these JAK inhibitors can limit M2a activation of macrophages induced by IL-4 and IL-13, as notably demonstrated by the down-regulation of the M2a associated surface marker CD206 and of the secretion of CCL18. Moreover, these JAK inhibitors reduced the expression of markers such as CXCL13, MARCO and SOCS3 in alternatively activated macrophages induced by IL-10 and dexamethasone (M2c+dex) or IL-10 alone (M2c MDM). For all polarization states, Jakinibs with inhibitory properties over JAK2 had the highest effects, at both 1 μM or 0.1 μM. Based on these in vitro results, we also explored the effects of JAK2/1 inhibition by ruxolitinib in vivo, on mouse macrophages in a model of HOCl-induced ILD, that mimics scleroderma-associated ILD. In this model, we showed that ruxolitinib significantly prevented the upregulation of pro-inflammatory M1 markers (TNFα, CXCL10, NOS2) and pro-fibrotic M2 markers (Arg1 and Chi3L3). These results were associated with an improvement of skin and pulmonary involvement. Overall, our results suggest that the combined anti-inflammatory and anti-fibrotic properties of JAK2/1 inhibitors could be relevant to target lung macrophages in autoimmune and inflammatory pulmonary disorders that have no efficient disease modifying drugs to date. [2] Purpose: T-cells engineered to express a chimeric antigen receptor (CAR T-cells) are a promising cancer immunotherapy. Such targeted therapies have shown long-term relapse-free survival in patients with B-cell leukemia and lymphoma. However, cytokine release syndrome (CRS) represents a serious, potentially life-threatening side effect often associated with CAR T-cell therapy. CRS manifests as a rapid (hyper)immune reaction driven by excessive inflammatory cytokine release, including interferon-γ and interleukin-6. Experimental Design: Many cytokines implicated in CRS are known to signal through the Janus kinase–signal transducers and activators of transcription (JAK-STAT) pathway. Here we study the effect of blocking JAK pathway signaling on CAR T-cell proliferation, anti-tumor activity and cytokine levels in in vitro and in vivo models. Results: We report that itacitinib, a potent, selective JAK1 inhibitor, was able to significantly and dose-dependently reduce levels of multiple cytokines implicated in CRS in several in vitro and in vivo models. Importantly, we also report that at clinically relevant doses that mimic human JAK1 pharmacologic inhibition, itacitinib did not significantly inhibit proliferation or antitumor killing capacity of three different human CAR T-cell constructs (GD2, EGFR, and CD19). Finally, in an in vivo model, antitumor activity of CD19-CAR T-cells adoptively transferred into CD19+ tumor bearing immuno-deficient animals was unabated by oral itacitinib treatment. Conclusion: Together, these data suggest that itacitinib has potential as a prophylactic agent for the prevention of CAR T-cell–induced CRS, and a phase II clinical trial of itacitinib for prevention of CRS induced by CAR T-cell therapy has been initiated (NCT04071366).[3] Pharmacological modulation of the Janus kinase (JAK) family has achieved clinically meaningful therapeutic outcomes for the treatment of inflammatory and hematopoietic diseases. Several JAK1 selective compounds are being investigated clinically to determine their anti-inflammatory potential. We used recombinant enzymes and primary human lymphocytes to assess the JAK1 specificity of itacitinib (INCB039110) and study inhibition of signal transducers and activators of transcription (STAT) signaling. Rodent models of arthritis and inflammatory bowel disease were subsequently explored to elucidate the efficacy of orally administered itacitinib on inflammatory pathogenesis. Itacitinib is a potent and selective JAK1 inhibitor when profiled against the other JAK family members. Upon oral administration in rodents, itacitinib achieved dose-dependent pharmacokinetic exposures that highly correlated with STAT3 pharmacodynamic pathway inhibition. Itacitinib ameliorated symptoms and pathology of established experimentally-induced arthritis in a dose-dependent manner. Furthermore, itacitinib effectively delayed disease onset, reduced symptom severity, and accelerated recovery in three distinct mouse models of inflammatory bowel disease. Low dose itacitinib administered via cannula directly into the colon was highly efficacious in TNBS-induced colitis but with minimal systemic drug exposure, suggesting localized JAK1 inhibition is sufficient for disease amelioration. Itacitinib treatment in an acute graft-versus-host disease (GvHD) model rapidly reduced inflammatory markers within lymphocytes and target tissue, resulting in a marked improvement in disease symptoms. This is the first manuscript describing itacitinib as a potent and selective JAK1 inhibitor with anti-inflammatory activity across multiple preclinical disease models. These data support the scientific rationale for ongoing clinical trials studying itacitinib in select GvHD patient populations.[4] |
| 分子式 |
C₃₂H₃₃F₄N₉O₅
|
|
|---|---|---|
| 分子量 |
699.66
|
|
| 精确质量 |
699.254
|
|
| 元素分析 |
C, 54.93; H, 4.75; F, 10.86; N, 18.02; O, 11.43
|
|
| CAS号 |
1334302-63-4
|
|
| 相关CAS号 |
Itacitinib;1334298-90-6
|
|
| PubChem CID |
67390313
|
|
| 外观&性状 |
White to light yellow solid powder
|
|
| tPSA |
194
|
|
| 氢键供体(HBD)数目 |
3
|
|
| 氢键受体(HBA)数目 |
15
|
|
| 可旋转键数目(RBC) |
10
|
|
| 重原子数目 |
50
|
|
| 分子复杂度/Complexity |
1090
|
|
| 定义原子立体中心数目 |
0
|
|
| InChi Key |
CEGWJIQFBNFMHQ-UHFFFAOYSA-N
|
|
| InChi Code |
InChI=1S/C26H23F4N9O.C6H10O4/c27-20-18(1-7-32-22(20)26(28,29)30)24(40)37-9-3-17(4-10-37)38-13-25(14-38,5-6-31)39-12-16(11-36-39)21-19-2-8-33-23(19)35-15-34-21;7-5(8)3-1-2-4-6(9)10/h1-2,7-8,11-12,15,17H,3-5,9-10,13-14H2,(H,33,34,35);1-4H2,(H,7,8)(H,9,10)
|
|
| 化学名 |
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中(例如氮气保护),避免吸湿/受潮。 |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (3.57 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (3.57 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (3.57 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.4293 mL | 7.1463 mL | 14.2927 mL | |
| 5 mM | 0.2859 mL | 1.4293 mL | 2.8585 mL | |
| 10 mM | 0.1429 mL | 0.7146 mL | 1.4293 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT04239989 | Recruiting | Drug: Itacitinib Drug: Itacitinib Adipate |
Bronchiolitis Obliterans | M.D. Anderson Cancer Center | April 8, 2021 | Phase 1 |
| NCT04070781 | Terminated | Drug: Itacitinib Drug: Tocilizumab | Steroid Refractory GVHD Graft Vs Host Disease |
Columbia University | January 20, 2020 | Phase 1 |
| NCT04339101 | Active, not recruiting Has Results |
Drug: Fludarabine Drug: Itacitinib Adipate |
Acute Leukemia Hematologic and Lymphocytic Disorder |
City of Hope Medical Center | November 11, 2020 | Phase 2 |
| NCT04200365 | Terminated | Drug: Itacitinib | Chronic Graft-versus-host-disease | SCRI Development Innovations, LLC | June 5, 2020 | Phase 2 |
Treatment effects on total symptom score (TSS).Haematologica.2017 Feb;102(2):327-335 |
Treatment effects on spleen volume.Haematologica.2017 Feb;102(2):327-335. |
Mean hemoglobin level and platelet count over time by dose cohort.Haematologica.2017 Feb;102(2):327-335. |