| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| Other Sizes |
|
| 靶点 |
DNA intercalator
|
|---|---|
| 体外研究 (In Vitro) |
Nemorubicin 对 HT-29、A2780、DU145、EM-2、Jurkat 和 CEM 细胞系表现出抗肿瘤活性,IC70 分别为 578 nM、468 nM、193 nM、191 nM、68 nM 和 131 ± 9 nM [1].
Nemorubicin 是一种由 CYP3A 激活的抗癌前药,能够生成更有效的代谢物 PNU-159682[1][2]. Nemorubicin 通过核苷酸切除修复发挥作用(NER)系统。与缺乏 XPG 的 L1210/0 细胞相比,保留 NER 的 L1210/DDP 细胞表现出更高水平的新霉素 (0-0.3 μM) 活性。对 Nemorubicin 具有抗性的细胞对紫外线损伤更加敏感[3]。 Nemorubicin 的 IC50 为 0.2 nM,比缺乏 P450 的 9L 细胞(IC50,23.9 nM)低 120 倍,表明它是对 9L/3A/4 细胞具有细胞毒性。此外,nemoribucicin 的 IC50 为 1.4 nM,可显着抑制 Adeno-3A4 感染的 U251 细胞。当 P450 还原酶过度表达时,新柔比星的细胞毒性更强[4]。 |
| 体内研究 (In Vivo) |
Nemorubicin 在大鼠、小鼠和狗的肝微粒体中被人肝细胞色素 P450 (CYP) 3A4 转变为 PNU-159682[2]。当对患有 9L/3A4 肿瘤的小鼠静脉内 (IV) 或瘤内 (it) 给药时,新柔比星 (60 µg/kg) 显着延缓肿瘤的生长,但对 scid 中 9L 肿瘤的肿瘤生长延迟没有明显影响老鼠。在患有 9L/3A4 肿瘤的小鼠中,新霉素(40 µg/kg,腹腔注射)没有显示出抗肿瘤活性,也没有宿主毒性[4]。
|
| 酶活实验 |
相关性研究。[1]
Nemorubicin /MMDX (20 μmol/L)与10个人肝脏微粒体部分孵育;孵育方案与上面描述的相同。在这些实验中获得的PNU-159682形成率与在相同微粒体样品中评估的几种已知的CYP形式选择性催化活性相关(数据由BD Gentest提供,硝苯地平氧化和红霉素n -去甲基化除外)。采用线性回归分析确定决定系数(r2)和P值。 化学和免疫化学抑制研究。[1] 在不存在(即对照)和存在已知的CYP形式选择性化学抑制剂的情况下,用混合HLMs评价了20 μmol/L Nemorubicin /MMDX形成PNU-159682的情况。以下抑制剂在先前确定的适当浓度下对HLMs产生CYP形式选择性抑制:7,8-苯黄酮(1 μmol/L, cyp1a2选择性),磺胺苯唑(20 μmol/L, cyp2c9选择性),奎尼丁(5 μmol/L, cyp2d6选择性),二乙基二硫代氨基甲酸酯(25 μmol/L;CYP2A6/ e1选择性)、troleandomycin (100 μmol/L, cyp3a选择性)和酮康唑(1 μmol/L, cyp3a选择性)。在可逆抑制剂(7,8-苯黄酮、奎尼丁、磺胺苯唑和酮康唑)的实验中,抑制剂与底物共孵育;孵育方案与上述相同。在以机制为基础的抑制剂,即二乙基二硫代氨基甲酸酯和troleandomycin的实验中,抑制剂与肝微粒体和NADPH (0.5 mmol)在37°C下预孵育15分钟,然后加入底物和额外的0.5 mmol NADPH。然后按照上述方法进行反应。 免疫化学抑制研究是用含有抑制单克隆抗体的小鼠腹水进行的,这种单克隆抗体已被证明对不同的人类CYP酶具有特异性。混合HLMs (0.25 mg微粒体蛋白/mL;在0.3 mol/L Tris (pH 7.4)中,与一定量含有抗CYP单抗(20-140 μg)的小鼠腹水在37℃下预孵育5分钟;然后在0.2 mL的总量中加入Nemorubicin /MMDX(终浓度,20 μmol/L)和NADPH(终浓度,0.5 mmol/L)引发反应,进行如上所述。这些试验中使用的每种单抗的最高浓度(即7 μg腹水蛋白/总CYP的pmol)先前已被证明可以在HLMs中达到饱和,以进行适当的CYP形式特异性反应。在没有单克隆抗体的情况下进行对照孵育。 Nemorubicin MMDX与cdna表达的人细胞色素P450酶[1] 孵育 MMDX与含有cdna表达的CYP酶的微粒体孵育按照HLMs的方法进行,但所用酶的量为50 pmol/mL,孵育60分钟后终止;底物浓度为20 μmol/L。所有的孵育都是一式两份。采用荧光高效液相色谱法分析各样品上清液PNU-159682含量。 Nemorubicin (3'-脱氨基-3'-[2''(S)-甲氧基-4''-吗啉基]阿霉素;MMDX)是一种目前处于肝细胞癌II/III期临床试验的研究药物。MMDX的生物活化产物,3'-脱氨基-3'',4'-脱水-[2''(S)-甲氧基-3''(R)-氧-4''吗啉基]阿霉素(PNU-159682),最近在该药物与补充NADPH的大鼠肝微粒体的孵育中被鉴定出来。本研究旨在获取MMDX在人体内转化为PNU-159682的信息,并探讨PNU-159684的抗肿瘤活性。 实验设计:使用人肝微粒体(HLM)和表达个体人细胞色素P450(CYP)的基因工程细胞系的微粒体来研究MMDX的生物转化。我们还分别使用一组体外培养的人肿瘤细胞系和荷瘤小鼠检测了PNU-159682的细胞毒性和抗肿瘤活性。 结果:HLMs将MMDX转化为主要代谢产物,其在液相色谱中的保留时间和串联质谱中的离子裂解时间与合成的PNU-159682相同。在来自10名供体的HLMs库中,PNU-159682的形成率与三种不同的CYP3A介导的活性显著相关。Troleandomycin和酮康唑均为CYP3A抑制剂,可显著减少HLMs形成PNU-159682;该反应也被CYP3A4/5单克隆抗体浓度依赖性地抑制。在检测的10个cDNA表达的CYP中,只有CYP3A4形成PNU-159682。此外,PNU-159682在体外的细胞毒性明显高于MMDX和阿霉素,并且在所测试的两种体内肿瘤模型中有效,即播散性小鼠L1210白血病和MX-1人乳腺癌异种移植物。 结论:CYP3A4是人类肝脏中的主要CYP,它将MMDX转化为一种更具细胞毒性的代谢产物PNU-159682,在体内保持抗肿瘤活性。[1] 研究人员最近证明,Nemorubicin (MMDX)是一种正在研究的抗肿瘤药物,可被人肝细胞色素P450(CYP)3A4转化为活性代谢产物PNU-159682。本研究的目的是:(1)研究实验室动物(小鼠、大鼠和狗)肝微粒体对MMDX的代谢,以确定这些物种是否也产生PNU-159682,并确定其形成的CYP形式;(2) 比较MMDX与人肝微粒体(HLMs)的动物代谢,以确定哪种动物最接近人类;(3) 探讨PNU-159682形成的差异是否是先前报道的MMDX宿主毒性与物种和性别相关差异的原因。MMDX的动物代谢被证明与HLM观察到的代谢在性质上相似,因为在所有受试物种中,MMDX主要通过单一的CYP3A形式转化为PNU-159682。然而,在动力学参数方面,物种间和物种内存在明显的定量差异。小鼠和雄性大鼠的V(max)和内在代谢清除率(CL(int))值最接近人类,表明这些物种是研究MMDX生物转化的最合适的动物模型。在这里测试的物种、性别和品系的动物中,MMDX CL(int)与之前报告的MMDX LD(50)值之间存在密切的负相关关系,表明MMDX体内毒性的差异很可能是由于PNU-159682形成程度的性别和物种相关差异造成的。 |
| 细胞实验 |
在药物治疗前 24 小时,将 9L 和 CHO 细胞铺在 96 孔板的一式三份孔中,每孔 3000 个细胞。四天内,将不同浓度的 IFA 或新霉素应用于细胞。用结晶紫 (A595) 对细胞染色后,计算相对细胞存活率。 Prism 4 用于根据数据点的半对数图计算 IC50 值 [4]。
体外细胞毒性[1]
采用Skehan等人描述的磺胺嘧啶B法评估阿霉素、Nemorubicin /MMDX和PNU-159682对贴壁肿瘤细胞系(HT-29、A2780和DU 145)的细胞毒性作用;通过使用ZM细胞计数器计算治疗期结束时的存活细胞数,评估药物对非贴壁肿瘤细胞系(CEM、Jurkat和EM-2)生长的影响。在处理前24小时给呈指数增长的细胞播种,药物处理1小时后,取出培养基,在无药培养基中培养72小时;对照细胞不接触药物。在每个实验中,测定分6次进行。然后用线性插值法从半对数浓度-响应曲线计算IC70值。数据以至少三个独立实验的平均值±SE表示。 |
| 动物实验 |
Male ICR/Fox Chase SCID mice are used to grow 9L and 9L/3A4 cells as solid tumors. After being cultivated in DMEM medium to 75% confluence, the cells are trypsinized, rinsed in PBS, and adjusted to 2 × 107 cells/mL of DMEM without added fetal serum. Implantation of either 9L or 9L/3A4 tumor cells is done on four-week-old SCID mice (18–20 g) by injecting 4 × 106 cells/0.2 mL of cell suspension, s.c. on each hind flank. Beginning on the seventh day following tumor implantation, tumor sizes (length and width) are measured twice a week using Vernier calipers. Nemorubicin dissolved in PBS is injected intravenously (IV) or directly intratumorally (i.t.) (three injections spaced seven days apart, each at 60 µg Nemorubicin per kg body weight) when the average tumor size reaches 300 to 400 mm3. Using a 30-gauge needle and a syringe pump set to 1 µL/s, intratumoral injections are administered. Three injections are given for each tumor in an i.t. treatment, with a 50 µL injection volume per tumor per 25 g mouse. In other words, 120 µL of 15 µg/mL of Nemorubicin solution is given to a 30 g mouse, with 20 µL given per site × 3 sites per tumor × 2 tumors/mouse. The same volume of PBS is injected intraperitoneally into drug-free controls. Nemorubicin is injected intraperitoneally (i.p.) at 40 or 60 µg/kg body weight in certain experiments. For the duration of the study, body weight and tumor sizes are measured twice a week. The formula for calculating tumor volumes is V = π/6 (L × W)3/2. The formula for calculating percent tumor regression is 100 × (V1-V2)/V1, where V1 represents the tumor volume on the day of medication treatment and V2 represents the tumor volume on the day that the greatest reduction in tumor size is observed after medication treatment. The amount of time needed for tumors to double in volume following drug treatment is known as the tumor doubling time [4].
Disseminated L1210 Leukemia. [1] Eight-week-old inbred female CD2F1 (BALB/c × DBA/2) were used for evaluation of the therapeutic efficacy of PNU-159682 , in comparison with that of Nemorubicin /MMDX. Disseminated neoplasia was induced by i.v. injection of 105 L1210 cells; 1 day later, the animals were randomly assigned to an experimental group (n = 10) and received a single i.v. injection of MMDX, PNU-159682 , or saline (control group). Treatment efficacy was evaluated by comparing the median survival time in the treated and control groups, and expressed as increase in life span as follows: % increase in life span = (100 × median survival time of drug treated mice / median survival time of control mice) − 100. Statistical comparison between the groups was made using the nonparametric Mann-Whitney test. Subcutaneous MX-1 Human Mammary Adenocarcinoma Xenografts. [1] Four- to six-week-old female CD-1 athymic nude mice were used for evaluation of the activity of PNU-159682 against MX-1 human mammary carcinoma xenografts. On day 0, animals (n = 14) were grafted s.c. with MX-1 tumor fragments in the right flank. Eight days later, they were randomly assigned to the drug treatment group or control group (n = 7 mice per group), and treatment was started. PNU-159682 was given i.v. (4 μg/kg) according to a q7dx3 (every 7 days for three doses) schedule; control animals received saline injections. Tumor volume was estimated from measurements done with a caliper using the formula: tumor volume (mm3) = D × d2 / 2; where D and d are the longest and the shortest diameters, respectively. For ethical reasons, control animals were sacrificed on day 21 when the mean tumor volume in the group was ∼2,500 mm3; animals receiving drug treatment were monitored up to day 50, at which point they were sacrificed. |
| 药代性质 (ADME/PK) |
Purpose: Nemorubicin (3'-deamino-3'-[2''(S)-methoxy-4''-morpholinyl]doxorubicin; MMDX) is an investigational drug currently in phase II/III clinical testing in hepatocellular carcinoma. A bioactivation product of MMDX, 3'-deamino-3'',4'-anhydro-[2''(S)-methoxy-3''(R)-oxy-4''-morpholinyl]doxorubicin (PNU-159682), has been recently identified in an incubate of the drug with NADPH-supplemented rat liver microsomes. The aims of this study were to obtain information about MMDX biotransformation to PNU-159682 in humans, and to explore the antitumor activity of PNU-159682.
Experimental design: Human liver microsomes (HLM) and microsomes from genetically engineered cell lines expressing individual human cytochrome P450s (CYP) were used to study MMDX biotransformation. We also examined the cytotoxicity and antitumor activity of PNU-159682 using a panel of in vitro-cultured human tumor cell lines and tumor-bearing mice, respectively.
Results: HLMs converted MMDX to a major metabolite, whose retention time in liquid chromatography and ion fragmentation in tandem mass spectrometry were identical to those of synthetic PNU-159682. In a bank of HLMs from 10 donors, rates of PNU-159682 formation correlated significantly with three distinct CYP3A-mediated activities. Troleandomycin and ketoconazole, both inhibitors of CYP3A, markedly reduced PNU-159682 formation by HLMs; the reaction was also concentration-dependently inhibited by a monoclonal antibody to CYP3A4/5. Of the 10 cDNA-expressed CYPs examined, only CYP3A4 formed PNU-159682. In addition, PNU-159682 was remarkably more cytotoxic than MMDX and doxorubicin in vitro, and was effective in the two in vivo tumor models tested, i.e., disseminated murine L1210 leukemia and MX-1 human mammary carcinoma xenografts.
Conclusions: CYP3A4, the major CYP in human liver, converts MMDX to a more cytotoxic metabolite, PNU-159682, which retains antitumor activity in vivo. [5]
We recently demonstrated that nemorubicin (MMDX), an investigational antitumor drug, is converted to an active metabolite, PNU-159682, by human liver cytochrome P450 (CYP) 3A4. The objectives of this study were: (1) to investigate MMDX metabolism by liver microsomes from laboratory animals (mice, rats, and dogs of both sexes) to ascertain whether PNU-159682 is also produced in these species, and to identify the CYP form(s) responsible for its formation; (2) to compare the animal metabolism of MMDX with that by human liver microsomes (HLMs), in order to determine which animal species is closest to human beings; (3) to explore whether differences in PNU-159682 formation are responsible for previously reported species- and sex-related differences in MMDX host toxicity. The animal metabolism of MMDX proved to be qualitatively similar to that observed with HLMs since, in all tested species, MMDX was mainly converted to PNU-159682 by a single CYP3A form. However, there were marked quantitative inter- and intra-species differences in kinetic parameters. The mouse and the male rat exhibited V(max) and intrinsic metabolic clearance (CL(int)) values closest to those of human beings, suggesting that these species are the most suitable animal models to investigate MMDX biotransformation. A close inverse correlation was found between MMDX CL(int) and previously reported values of MMDX LD(50) for animals of the species, sex and strain tested here, indicating that differences in the in vivo toxicity of MMDX are most probably due to sex- and species-related differences in the extent of PNU-159682 formation. [6] |
| 参考文献 |
|
| 其他信息 |
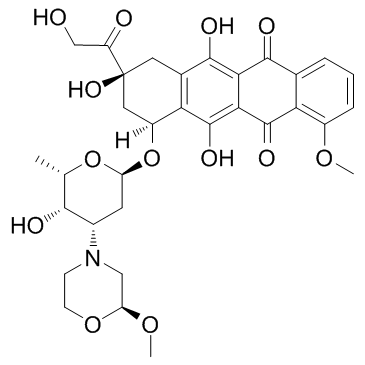
Nemorubicin is a member of morpholines, an anthracycline antibiotic, a primary alpha-hydroxy ketone and a tertiary alpha-hydroxy ketone. It is functionally related to a doxorubicin.
Nemorubicin is a morpholinyl analogue of the anthracycline doxorubicin with antineoplastic activity. Nemorubicin is metabolized via the P450 CYP3A enzyme to a highly cytotoxic derivative. Unlike most anthracyclines, nemorubicin is a topoisomerase I inhibitor and appears to exert its effect through the nucleotide excision repair (NER) system. In addition, this agent does not show cross-resistance with other anthracyclines. We recently demonstrated that nemorubicin (MMDX), an investigational antitumor drug, is converted to an active metabolite, PNU-159682, by human liver cytochrome P450 (CYP) 3A4. The objectives of this study were: (1) to investigate MMDX metabolism by liver microsomes from laboratory animals (mice, rats, and dogs of both sexes) to ascertain whether PNU-159682 is also produced in these species, and to identify the CYP form(s) responsible for its formation; (2) to compare the animal metabolism of MMDX with that by human liver microsomes (HLMs), in order to determine which animal species is closest to human beings; (3) to explore whether differences in PNU-159682 formation are responsible for previously reported species- and sex-related differences in MMDX host toxicity. The animal metabolism of MMDX proved to be qualitatively similar to that observed with HLMs since, in all tested species, MMDX was mainly converted to PNU-159682 by a single CYP3A form. However, there were marked quantitative inter- and intra-species differences in kinetic parameters. The mouse and the male rat exhibited V(max) and intrinsic metabolic clearance (CL(int)) values closest to those of human beings, suggesting that these species are the most suitable animal models to investigate MMDX biotransformation. A close inverse correlation was found between MMDX CL(int) and previously reported values of MMDX LD(50) for animals of the species, sex and strain tested here, indicating that differences in the in vivo toxicity of MMDX are most probably due to sex- and species-related differences in the extent of PNU-159682 formation. Source: Biochem Pharmacol. 2008 Sep 15;76(6):784-95. Antibody drug conjugates (ADCs) normally compose of a humanized antibody and small molecular drug via a chemical linker. After decades of preclinical and clinical studies, a series of ADCs have been widely used for treating specific tumor types in the clinic such as brentuximab vedotin (Adcetris®) for relapsed Hodgkin's lymphoma and systemic anaplastic large cell lymphoma, gemtuzumab ozogamicin (Mylotarg®) for acute myeloid leukemia, ado-trastuzumab emtansine (Kadcyla®) for HER2-positive metastatic breast cancer, inotuzumab ozogamicin (Besponsa®) and most recently polatuzumab vedotin-piiq (Polivy®) for B cell malignancies. More than eighty ADCs have been investigated in different clinical stages from approximately six hundred clinical trials to date. This review summarizes the key elements of ADCs and highlights recent advances of ADCs, as well as important lessons learned from clinical data, and future directions.[3] Background: Targeted EDV nanocells loaded with doxorubicin and microRNA16a have shown excellent safety profiles in Phase I trials in recurrent glioma and mesothelioma. This planned safety analysis of an ongoing first-in-human, open label Phase I/IIa study in patients with treatment-refractory metastatic pancreatic cancer, assesses safety, biologic and clinical activity of EGFR-targeted EDV nanocells carrying cytotoxic drug PNU-159682, designed to overcome drug resistance, combined with EDV nanocells carrying immunomodulatory adjuvant α-galactosyl ceramide, designed to stimulate anti-tumour immune response. Methods: 9 patients with advanced pancreatic cancer enrolled in the dose escalation phase to evaluate safety of the EDV combination. Doses gradually escalated from 2 x 109 EDVs/dose to a maximum of 7 x 109 EDVs/dose in Week 7, with subsequent dosing at the maximum dose achieved in Cycle 1. iRECIST criteria was used to assess tumour response after each cycle, and blood was collected each cycle for cytokine and PBMC analysis. Results: Combination EDVs were well tolerated with no DLTs, and no drug related SAEs. A minority of patients experienced G1 infusion reactions, which responded promptly to supportive treatment. PR or SD was achieved at 8 weeks in 8/9 patients (CBR 89%), with responses confirmed at 4 months in 4/5 evaluable patients (80%), with 2 durable responses seen beyond 6 months. Exploratory analyses have revealed elevation of IFN-α and IFN-γ in almost all evaluable patients (6/8). In addition, we observed elevated CD8+ T cells (2/8), iNKT, dendritic and NK cells (3/8), and a reduction in exhausted CD8+ T cells (3/8), suggesting activation of both innate and adaptive immune responses. Conclusions: EDVs carrying the cytotoxic drug and immune adjuvant are safe and well tolerated. Early signals point to durable responses, possibly related to the development of an innate and adaptive immune response along with cytotoxic effects on drug resistant tumour cells. The Phase IIa study plans to enrol an additional 35 patients to further evaluate safety and anti-tumour efficacy. Clinical trial information: ACTRN12619000385145.[4] |
| 分子式 |
C32H37NO13
|
|---|---|
| 分子量 |
643.63508
|
| 精确质量 |
643.226
|
| 元素分析 |
C, 59.71; H, 5.79; N, 2.18; O, 32.32
|
| CAS号 |
108852-90-0
|
| 相关CAS号 |
Nemorubicin;108852-90-0; 108943-08-4 (HCl)
|
| PubChem CID |
65907
|
| 外观&性状 |
Red to pink solid powder
|
| 密度 |
1.6±0.1 g/cm3
|
| 沸点 |
852.2±65.0 °C at 760 mmHg
|
| 闪点 |
469.2±34.3 °C
|
| 蒸汽压 |
0.0±0.3 mmHg at 25°C
|
| 折射率 |
1.681
|
| LogP |
4.7
|
| tPSA |
201.75
|
| 氢键供体(HBD)数目 |
5
|
| 氢键受体(HBA)数目 |
14
|
| 可旋转键数目(RBC) |
7
|
| 重原子数目 |
46
|
| 分子复杂度/Complexity |
1160
|
| 定义原子立体中心数目 |
7
|
| SMILES |
COC1=C2C(C(C3=C(O)C(C[C@](C(CO)=O)(O)C[C@]4([H])O[C@H]5C[C@H](N6CCO[C@H](OC)C6)[C@H](O)[C@H](C)O5)=C4C(O)=C3C2=O)=O)=CC=C1
|
| InChi Key |
CTMCWCONSULRHO-UHQPFXKFSA-N
|
| InChi Code |
InChI=1S/C32H37NO13/c1-14-27(36)17(33-7-8-44-22(12-33)43-3)9-21(45-14)46-19-11-32(41,20(35)13-34)10-16-24(19)31(40)26-25(29(16)38)28(37)15-5-4-6-18(42-2)23(15)30(26)39/h4-6,14,17,19,21-22,27,34,36,38,40-41H,7-13H2,1-3H3/t14-,17-,19-,21-,22-,27+,32-/m0/s1
|
| 化学名 |
(7S,9S)-6,9,11-trihydroxy-9-(2-hydroxyacetyl)-7-[(2R,4S,5S,6S)-5-hydroxy-4-[(2S)-2-methoxymorpholin-4-yl]-6-methyloxan-2-yl]oxy-4-methoxy-8,10-dihydro-7H-tetracene-5,12-dione
|
| 别名 |
Methoxymorpholinyldoxorubicin; PNU 152243; PNU-152243A; PNU152243A; PNU-152243A; PNU 152243A; Nemorubicin; Nemorubicin; 108852-90-0; Nemorubicin [INN]; Methoxymorpholino-doxorubicin; Methoxymorpholinyl doxorubicin; FCE-23762; Nemorubicin (GMP); 3'-DESAMINO-3'-(2-METHOXY-4-MORPHOLINYL)-DOXORUBICIN; methoxymorpholinyl-doxorubicin; 3′-deamino-3′-[2″(S)-methoxy-4″-morpholinyl]doxorubicin; MMDX
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO: ~65 mg/mL (~101 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 3.25 mg/mL (5.05 mM) (饱和度未知) in 10% DMSO + 40% PEG300 +5% Tween-80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 32.5 mg/mL澄清的DMSO储备液加入400 μL PEG300中,混匀;再将50 μL Tween-80+加入到上述溶液中,混匀;然后加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.5537 mL | 7.7683 mL | 15.5366 mL | |
| 5 mM | 0.3107 mL | 1.5537 mL | 3.1073 mL | |
| 10 mM | 0.1554 mL | 0.7768 mL | 1.5537 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
|
|