| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| Other Sizes |
| 靶点 |
Mitochondrial; neuroprotective
|
|---|---|
| 体外研究 (In Vitro) |
在不使用来自大脑、睫状体或胶质细胞的神经营养因子的情况下,原代胚胎大鼠脊髓 MN 在接种一小时后暴露于浓度范围为 0.1 至 10 µM 的 Olesoxime (TRO 19622) 中,可显着防止细胞损伤和死亡。这种保护在培养物中持续了三天。浓度为 10 µM 的 Olesoxime (TRO 19622) 通过神经营养因子混合物(包括大脑、睫状体和神经胶质细胞产生的因子)的作用维持 74±10% 的神经元存活。在此测试中,平均 EC50 为 3.2±0.2 µM。 Olesoxime (TRO 19622) 不仅可以保护 MN 细胞体,还可以促进神经突发育。在 1 µM 浓度下,olesoxime (TRO 19622) 仅略微提高细胞活力,但显着促进每个细胞的神经突发育达 54% [1]。人们发现了一类新型胆固醇肟,称为 Olesoxime (TRO 19622),因为它能够在缺乏神经营养因子的情况下提高纯运动神经元的存活率。 Olesoxime (TRO 19622) 选择性地靶向线粒体外膜中的蛋白质,重点关注线粒体并抑制氧化应激介导的通透性转变孔开放等过程[2]。
在细胞接种后1小时接触奥利索西(0.1-10 µM浓度范围),能显著保护原代培养的胚胎大鼠脊髓运动神经元(在缺乏脑源性、睫状神经营养因子和胶质细胞源性神经营养因子的条件下培养3天)免于死亡。当浓度为10 µM时,奥利索西维持了74±10%的神经元存活率(该比例与三种神经营养因子联合使用的效果相当)。本实验中测得的平均EC50值为3.2±0.2 µM。除保护神经元胞体外,奥利索西还促进神经突生长:在仅提高细胞存活率38%的1 µM浓度下,可使单个细胞的神经突总生长量增加54%。 化疗药物喜树碱能引起DNA链断裂并增加活性氧生成。皮质神经元与喜树碱共培养时,联合使用奥利索西可在16小时后产生剂量依赖性的细胞存活率提升,并降低活化的caspase-3和-7水平。这些效应与脑源性神经营养因子类似,但奥利索西的神经保护作用不依赖于ERK1/2或PI3K通路的激活。 微管靶向药物的体内给药常因周围神经病变发展而受限。体外实验显示,微管靶向药物会抑制大鼠和人类分化神经细胞的神经突生长,并引发末端结合蛋白(EB)1和EB2从微管解离至胞质。而同时暴露于奥利索西能维持EB蛋白分布和神经突生长。 通过啮齿类动物中枢神经系统细胞培养模型,在体外检测了奥利索西的髓鞘形成促进作用。奥利索西可剂量依赖性加速神经前体细胞向少突胶质前体细胞的分化,并在背根神经节神经元与少突胶质前体细胞的共培养体系中增强髓鞘形成[1]。 奥利索西(Olesoxime)是一种类胆固醇神经保护化合物,其作用靶点为线粒体电压依赖性阴离子通道(VDACs)。研究发现VDACs同样存在于质膜中,并在突触前成分中高度表达。本研究探讨了奥利索西与VDAC抑制剂对小鼠神经肌肉接头神经传递的影响。电生理分析显示:奥利索西能选择性抑制单次刺激和20Hz高频刺激诱发的神经递质释放,同时降低低频(0.5Hz)和20Hz刺激下FM1-43染料的流失速率(突触小泡胞吐作用指标)。提高细胞外Cl-浓度可增强奥利索西对胞吐的作用,且奥利索西能增加细胞内Cl-水平。奥利索西对诱发突触小泡胞吐及[Cl-]i的影响可被膜通透性与非通透性VDAC抑制剂阻断。免疫荧光标记证实突触膜上存在VDACs表达。鱼藤酮诱导线粒体功能障碍会干扰FM1-43的胞吐释放,而细胞通透性VDAC抑制剂(非奥利索西或非通透性VDAC抑制剂)可部分缓解鱼藤酮导致的FM1-43卸载异常和线粒体超氧化物生成。这表明奥利索西通过作用于质膜VDACs来限制神经传递——VDACs的激活可能通过增加神经末梢阴离子内流来抑制突触小泡胞吐[5]。 |
| 体内研究 (In Vivo) |
成年小鼠每天皮下注射 Olesoxime (TRO 19622)(3 或 30 mg/kg)超过两个月,耐受性良好,没有毒性或不良反应 [1]。当动物在损伤后口服治疗五天时,Olesoxime (TRO 19622) 以剂量依赖性方式增加运动神经元细胞体的存活率;在此剂量下,运动神经元存活率为 29 ±2% (n=18),与载体治疗的动物相比,存活率增加了 42% [3]。接受 3 mg/kg/d 或 30 mg/kg/d Olesoxime (TRO 19622) 预防性治疗的紫杉醇治疗大鼠分别具有 239±17.6 和 247±14.4 IENF/cm。对于两种剂量,下降幅度均显着小于用媒介物施用紫杉醇治疗的大鼠中观察到的 46%。
奥利索西(Olesoxime)是一种类胆固醇小分子化合物,最初在针对肌萎缩侧索硬化症及其他运动神经元退行性疾病的药物筛选中被发现。该药物不仅在体外和体内实验中表现出对运动神经元的神经保护与促再生作用,还在长春新碱和糖尿病引发的痛性周围神经病变大鼠模型中显示出镇痛效应。本研究采用紫杉醇诱导的痛性周围神经病变大鼠模型,旨在验证奥利索西能否逆转已形成的神经病理性疼痛,并探究其在紫杉醇暴露期间给药能否预防神经病理性疼痛综合征的发生及伴随的表皮感觉神经末梢分支退化。结果显示:奥利索西显著改善已形成的机械性异常性疼痛和机械性痛觉过敏,连续给药5天未出现耐受现象,且镇痛效果在末次给药后持续5-10天。在紫杉醇暴露期间联合给予奥利索西,可显著且持久地减轻机械性异常性疼痛/痛觉过敏的严重程度,并明显减少感觉神经末梢分支的退化。奥利索西通过靶向线粒体蛋白发挥作用,其效应支持紫杉醇诱发痛性周围神经病变的线粒体毒性假说。我们得出结论:奥利索西在临床上或可用于预防和治疗紫杉醇诱发的痛性周围神经病变。[4] 奥利索西在面神经轴切断术诱导的新生大鼠运动神经元退化模型中进行测试。神经切断术后7天,连续5天口服奥利索西(100 mg/kg)的大鼠比溶剂对照组表现出显著更高的运动神经元存活率。 为评估奥利索西能否促进周围神经再生,对坐骨神经压伤成年小鼠皮下注射奥利索西(0.3、3或30 mg/kg)。给药组在伤后2周开始出现剂量依赖性的神经再生加速,至第4周时所有剂量组与溶剂对照组均存在显著差异。第6周时,奥利索西治疗组小鼠神经肌肉功能恢复达假手术组的80%。组织学分析显示,溶剂对照组轴突横截面积总体小于对照组,而30 mg/kg奥利索西组轴突面积显著增大(7.6±0.1 vs 6.0±0.1 µm²;p<0.05)。第4周时,所有剂量组均显著减少"低髓鞘化"纤维数量。 在G93A高表达SOD1转基因ALS小鼠模型中,从出生后60天开始皮下注射Olesoxime/奥利索西(3或30 mg/kg)可改善运动功能、延迟疾病发作并使生存期延长10%。其中3 mg/kg剂量组体重下降起始时间延迟15天(p<0.01),两个剂量组网格测试功能衰退均延迟约11天(p<0.01)。 在链脲佐菌素(55 mg/kg)诱导的糖尿病性神经病变大鼠模型中,通过电生理检测和甩尾试验评估神经病变,采用热异常性疼痛及热/机械性痛觉过敏测试检测伤害感受。糖尿病诱导10天后开始口服Olesoxime/奥利索西(30和300 mg/kg/天)可显著缓解疼痛(p≤0.05),效果与3 mg/kg吗啡相当,同时显著降低复合肌肉动作电位潜伏期(运动神经传导指标)。单次口服奥利索西(10、30或100 mg/kg)可剂量依赖性逆转糖尿病性异常性疼痛,最高剂量组与溶剂对照组差异显著(p≤0.05)。连续给药5天后,所有剂量均显著改善触觉异常性疼痛,效果与加巴喷丁(50 mg/kg bid)相当。 在紫杉醇(第0、2、4、6天腹腔注射2 mg/kg)诱导的大鼠神经病理性疼痛模型中,预防性研究(-1至15天给药)和治疗性研究(第25天起连续5天给药)显示:口服Olesoxime/奥利索西(3或30 mg/kg/天)能显著缓解紫杉醇诱导的异常性疼痛/痛觉过敏至第40天(末次给药后25天),同时将表皮内神经纤维的损失率从紫杉醇组的46%降至22-25%。10或100 mg/kg/天剂量组在给药次日即显著改善痛觉过敏和异常性疼痛,虽然效果可逆,但末次给药后镇痛作用维持10天。 在长春新碱(第1、4、6天静脉注射200 µg/kg)诱导的大鼠神经病理性疼痛模型中,最高测试剂量(100 mg/kg口服)首次给药4小时后即显著减轻异常性疼痛(p<0.001)。连续给予10、30和100 mg/kg/天Olesoxime/奥利索西可显著缓解第11-14天的长春新碱诱导异常性疼痛[1]。 |
| 酶活实验 |
肌萎缩侧索硬化症(ALS)是一种致命的神经退行性疾病,其特征是皮层和脊髓运动神经元的逐渐死亡,目前尚无有效的治疗方法。使用能够在体外预防运动神经元细胞死亡的化合物的基于细胞的测定法,筛选了大约40000种低分子量化合物,以确定潜在的小分子治疗方法。我们报道了胆甾-4-烯-3-酮肟(TRO19622)作为治疗ALS的潜在候选药物的鉴定。在体外,TRO19622在缺乏营养支持的情况下以剂量依赖的方式促进运动神经元的存活[3]。
|
| 细胞实验 |
溶液与化学试剂 [5]
神经半膈肌标本固定于Sylgard包被的培养槽底部。肌肉组织以5 ml·min−1流速持续灌注生理溶液(129 mM NaCl、5 mM KCl、2 mM CaCl2、1 mM MgSO4、1 mM NaH2PO4、20 mM NaHCO3、11 mM葡萄糖及3 mM HEPES;pH=7.4),溶液经5% CO2/95% O2混合气体饱和。部分实验采用高Cl−浓度溶液(146 mM NaCl、5 mM KCl、2 mM CaCl2、1 mM MgCl2、13.5 mM胆碱氯化物及3 mM HEPES;pH=7.4)。 在20 Hz或5 Hz神经刺激前,使用0.4 μM 奥利索西预处理20分钟。Olesoxime/奥利索西溶解于DMSO,溶剂终浓度为0.001%。0.001-0.1%浓度的DMSO对小鼠膈肌神经肌肉传递无影响,故DMSO实验数据作为对照。VDAC抑制剂DIDS(50 μM,4,4'-二异硫氰酸二苯乙烯-2,2'-二磺酸;Tocris)和S-18(1 μM,S-18硫代磷酸随机寡核苷酸)在奥利索西给药前5分钟加入灌流液并维持至实验结束。鱼藤酮(10 μM,作用30分钟)用于诱导线粒体功能障碍。(−)维沙米可(2 μM)作为囊泡乙酰胆碱转运体抑制剂,用于阻断突触小泡乙酰胆碱再填充。 突触后电位记录 [5] 使用2.5 M KCl填充的标准玻璃微电极(尖端电阻5-10 MΩ)记录终板电位(EPPs)和微小终板电位(MEPPs)。信号检测采用Model 1600放大器和LA II数字I/O板,记录信号经0.03 Hz-10 kHz滤波后以50 kHz采样率数字化存储,供离线分析。通过定制程序处理数据,计算平均振幅、上升时间(峰值20%-80%时程)和衰减时间(峰值至50%时程)。MEPPs频率通过记录150-200个信号后统计得出,信噪比>7:1,检测阈值设为0.2 mV。神经刺激采用吸吮电极连接Model 2100隔离刺激器,施加0.1 ms矩形超强电脉冲(频率0.5 Hz或20 Hz)。为抑制肌肉收缩,记录前20分钟在灌流液中加入肌特异性Na+通道抑制剂μ-芋螺毒素-GIIIB(0.5 μM)。在0.5 Hz低频刺激下记录20分钟奥利索西处理的EPPs,随后对预处理肌肉的膈神经施加20 Hz高频刺激3分钟。 |
| 动物实验 |
In vivo, TRO19622 rescued motor neurons from axotomy-induced cell death in neonatal rats and promoted nerve regeneration following sciatic nerve crush in mice. In SOD1G93A transgenic mice, a model of familial ALS, TRO19622 treatment improved motor performance, delayed the onset of the clinical disease, and extended survival. TRO19622 bound directly to two components of the mitochondrial permeability transition pore: the voltage-dependent anion channel and the translocator protein 18 kDa (or peripheral benzodiazepine receptor), suggesting a potential mechanism for its neuroprotective activity. TRO19622 may have therapeutic potential for ALS and other motor neuron and neurodegenerative diseases[3].
For in vivo studies, Olesoxime/TRO19622 was administrated either by oral gavage as a suspension in hydroxypropylmethylcellulose or vegetable oil or by subcutaneous [3]. Olesoxime was prepared fresh daily in corn oil. Olesoxime or the vehicle was administered via oral gavage in a volume of 5.0 ml/kg. The Olesoxime doses used here (3-100 mg/kg) were chosen based on prior reports of neuroprotective and analgesic activity.[4] Treatment paradigm [4] To determine whether Olesoxime has an analgesic effect on established paclitaxel-evoked pain, we examined withdrawal responses in animals after daily oral dosing with olesoxime during the period of approximate peak pain severity. Baseline responses in the behavioral tests were done on D23 and D24 after the first administration of paclitaxel (the approximate beginning of the plateau phase of maximal pain severity), and three experimental groups were formed such that each had approximately equal mechano-allodynia and mechano-hyperalgesia. The groups (each n = 12) were then randomly assigned to receive Olesoxime (10 mg/kg or 100 mg/kg) or vehicle on 5 consecutive days, beginning on D27. Behavior was tested 4 h after each of the daily administrations. Behavior was also assessed during a washout period beginning 1 day after the last administration of olesoxime/vehicle (washout day 1; WD1), and on WD3, WD5, WD10, WD14, and WD18. Behavioral assays were done by an observer who was blind as to group assignment. Preventive paradigm [4] To determine whether Olesoxime could prevent the development of paclitaxel-evoked painful peripheral neuropathy, three experimental groups were compared (each n = 12). The groups were administered vehicle or Olesoxime at 3 mg/kg or 30 mg/kg daily for 17 consecutive days, starting the day prior to the first injection of paclitaxel (D-1) until 9 days after the last injection of paclitaxel (D15). Dosing was continued after the last paclitaxel injection because there is a delay of several days before the onset of statistically significant pain hypersensitivity [8] and the time of onset of the pain-producing pathology is thus uncertain. On those days when both drugs were to be administered, Olesoxime was given at 0900 h and paclitaxel at 1300 h. Behavioral assays were repeated every 3-5 days beginning on D16 until D40 by an observer who was blind as to group assignment. Effects of prophylactic treatment on paclitaxel-evoked intraepidermal nerve fiber degeneration [4] The paclitaxel model used here has been shown to be associated with a significant loss of intraepidermal nerve fibers (IENFs), i.e., the sensory terminal receptor arbors of the afferents that innervate the epidermis [11, 22]. To determine whether olesoxime prevents this degeneration, the prophylactic dosing protocol described above was repeated in three groups of rats (Olesoxime at 3 mg/kg or 30 mg/kg, or vehicle; each n = 12). Behavioral tests were done on D29 and D30 to confirm the presence of the expected paclitaxel-evoked pain hypersensitivity in the vehicle-treated group and the expected analgesic effects in the 3 mg/kg and 30 mg/kg groups. On D31, eight rats were randomly selected from each group and sacrificed for the immunocytochemical assessment of IENFs. An additional four naïve rats (i.e., neither paclitaxel nor olesoxime treatment) of the same age and weight were sacrificed as normal controls. Effects on paclitaxel-evoked spontaneous discharge [4] Paclitaxel-evoked painful peripheral neuropathy is associated with an abnormal incidence of spontaneously discharging A-fibers and C-fibers. To determine whether the acute analgesic effects of Olesoxime were associated with suppression of this discharge, we surveyed the incidence of spontaneously discharging fibers in rats that had been treated with vehicle or 100 mg/kg olesoxime (each n = 6) on two consecutive days (the treatment paradigm study described above found significant anti-allodynic and anti-hyperalgesic effects after this treatment). All rats had confirmed paclitaxel-evoked pain (assessed on D23-D24) and subsequently received Olesoxime or vehicle treatment during the plateau phase of peak pain severity (D27-D44). Electrophysiological experiments began on the second day of treatment, 4 h after drug/vehicle administration. The paclitaxel-treated rats were compared to a group of four naïve rats (neither paclitaxel nor olesoxime exposure). The experimenter was blind as to the rat's group assignment. Surgical preparation for fiber recordings required about 1 h and data were collected over the next 2-3 h when plasma concentrations of Olesoxime are maximal after oral administration. Recording methods were identical to those described previously. Briefly, the number of individually-identifiable fibers in each microfilament was determined and the incidence of individually-identifiable fibers with spontaneous discharge was noted, as was their discharge frequency. The conduction velocity was determined for all individually-identifiable fibers. We did not differentiate between A-fibers with conduction velocities in the A□ and A□ ranges because it is impossible to differentiate functional classes of A-fibers on this basis. We purposely avoided characterizing the fibers’ responses to receptive field stimulation. To do so would require repeated application of noxious stimuli that might sensitize nociceptors. Sensitized nociceptors have an ongoing discharge that would be impossible to distinguish from paclitaxel-evoked spontaneous discharge. Olesoxime plasma levels [4] Blood was drawn from the tail vein in animals enrolled in the behavioral studies or via cardiac puncture in the animals sacrificed for the anatomical and electrophysiological studies, collected in lithium-heparin tubes, centrifuged at 3000 rpm for 10 min and the plasma frozen on Dry Ice. Quantification was performed via high-performance liquid chromatography with MS/MS detection. The detection limit of the assay was 0.01 μM. |
| 药代性质 (ADME/PK) |
Metabolism and pharmacokinetics [1]
Olesoxime has been administered to rats and mice by oral gavage as a suspension in hydroxypropylmethylcellulose or vegetable oil, and by subcutaneous injection as a mixture of Cremophor EL/dimethyl sulfoxide/ethanol/ phosphate-buffered saline (5:5:10:80, respectively). To determine bioavailability, adult mice received daily subcutaneous injections of olesoxime for 1 or 6 weeks at doses of 0.3, 3 and 30 mg/kg. Levels of olesoxime in plasma and brain were measured by high performance liquid chromatography with tandem mass spectroscopy detection. Plasma and brain olesoxime levels were dose-dependent, reached steady-state by 1 week and remained stable over the 6-week treatment period. Levels of olesoxime were approximately 1.25 and 0.5 µM in plasma and brain, respectively, at the 3-mg/kg/day dose. Pharmacokinetic studies in rats demonstrated that olesoxime had an elimination t1/2 value of approximately 24 h, leading to accumulation with steady-state levels in plasma achieved after three daily oral administrations. In the diabetic and vincristine-treated rats, repeated oral administration of a 10-mg/kg/day dose of olesoxime resulted in steady-state plasma concentrations of between 2 and 4.5 µM. Single-dose oral olesoxime at 100 mg/kg resulted in plasma concentrations between 14.2 and 37.5 µM in both models. In paclitaxel-treated rats, plasma levels after the first 10-mg/kg dose of olesoxime were 0.82 µM increasing to 1.39 µM after the fifth daily dose. For a 100-mg/kg dose, day 1 and day 5 plasma levels were 6.75 and 8.91 µM, respectively. A phase I, randomized, double-blind, placebo-controlled, dose-escalation clinical trial assessed the pharmacokinetics of four doses of olesoxime (50, 150, 250 and 500 mg po, qd) administered for 11 consecutive days to healthy Caucasian volunteers (n = 48). The absorption and elimination of olesoxime were slow at all doses: the Tmax value was approximately 10 h and concentrations of olesoxime were measurable for up to 19 days after dosing. The mean t1/2 was comparable between doses at approximately 120 h. Dose increased in a ratio of 3, 5 and 10 (from 50 to 150, 250 and 500 mg, respectively), but day 1 Cmax increased in a ratio of 2.2, 4.4 and 10.2, and AUC0-τ increased in a ratio of 2.1, 4.6 and 10.8. At steady-state, which was reached on day 11 in all groups, Cmax increased with dose in a ratio of 2.1, 7.2 and 12.2, and AUC0-τ increased with a ratio of 2.0, 6.5 and 11.6. Mean accumulation ratios of Cmax and Ctrough observed between days 1 and 11 were approximately 4. Plasma pharmacokinetic profiles were similar between volunteers and across all doses: the coefficients of variation of Cmax and AUC0-τ were between 21 and 47% on day 11. The pharmacokinetics of olesoxime (dosed just before a meal), co-administered with riluzole for 1 month, were assessed in a phase Ib clinical trial in patients (n = 36) with ALS. Median male and female Ctrough values were 512 and 742 ng/ml at a 125-mg dose of olesoxime, 979 and 1685 ng/ml at a 250-mg dose, and 2965 and 3310 ng/ml at a 500-mg dose; these values did not indicate a gender effect at any dose. The maximum Ctrough value was 5780 ng/ml and was observed on day 15 in the 500-mg dose group. Day 15 and day 30 olesoxime Ctrough values were similar, suggesting that steady-state was reached by day 15. Greater Ctrough plasma concentrations were observed in patients with ALS than in healthy volunteers, which may have been caused by co-administration with food or riluzole. The pharmacokinetics of olesoxime were also assessed in a phase Ib trial in pediatric (n = 5) and adult (n = 3) patients with SMA. After a single dose of olesoxime (125 mg po), the Cmax and AUC values were comparable in children and adults after adjusting the dose to mg/kg; Tmax, t1/2 and total clearance were identical. Results after once-daily dosing were similar. Brain penetration of olesoxime was studied in mice and rats by a variety of methods. The relative level of olesoxime brain penetration compared to known brain-penetrating compounds was evaluated using the in situ rat brain perfusion technique initially developed by Q. Smith. A total of six rats, 5 to 6 weeks old, were perfused with 3H-Olesoxime labelled in the C4 position. The permeation coefficient of the blood brain barrier (Kin) was found to be 5.9 ± 3.0 µl/g/s in a scale ranging from 0.01 to 60. When compared to reference compounds, olesoxime penetration falls between colchicine, a permeability-dependent compound, and flumazenil, a flux-dependent compound. An extraction and analytical method was also developed to detect and quantify olesoxime in both plasma and brain tissue. The amount of olesoxime in brains of mice used in various pharmacokinetic and efficacy studies allowed to compare brain levels to the AUC measured from plasma samples collected in the same study. Chronic administration performed in the nerve crush study in mice demonstrates accumulation in brain tissue over time while plasma concentrations remain constant (Table 4). Using these different approaches it can be concluded that olesoxime enters the brain and that tissue levels corresponding to efficacy can be correlated with plasma concentrations. [2] |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity [1]
Daily administration of olesoxime (3 or 30 mg/kg sc) to adult mice for more than 2 months was well tolerated without toxicity or adverse effects. Toxicity was not observed in animals exposed to doses 40-fold greater than the expected therapeutic dose for 4 weeks. At the time of publication, no further toxicity data were available. Early CNS safety of olesoxime was assessed on the generation/propagation of action potentials in cultured cortical neurons. About 10 days after plating, spontaneous action potentials of cortical neurons were recorded on Multi-Electrode Arrays. The firing rate (Hz/s) was measured in control conditions (standard saline solution) for 10 minutes, and then olesoxime was perfused for an additional 10 minute period. When exposed to 10 µM olesoxime, cortical neurons did not show any modification of their firing rate. In comparison, complete firing inhibition was observed immediately after tetrodotoxin (100 nM TTX) perfusion (Figure 8A). Similarly acute exposure of rat E14 motoneurons to 10 µM olesoxime (3 min) did not modify the action potential profiles evoked by a 20 Hz stimulation (data not shown). [2] Side effects and contraindications [1] In the phase I clinical trial of olesoxime (50, 150, 250 and 500 mg po, qd for 11 days) in healthy volunteers, no serious adverse events were reported. There were 69 treatment-emergent adverse events (TEAEs) reported, of which 18 were considered possibly related, 22 were considered unlikely to be related and 27 were judged unrelated to olesoxime. Of the possibly related TEAEs, two occurred after the 50-mg dose, two occurred after the 250-mg dose, seven occurred after the 500-mg dose and seven occurred after placebo. Most TEAEs were mild (48 events) or moderate (21 events) in intensity. The most frequently reported TEAEs were diarrhea (9 episodes), headache (7 episodes), constipation (4 episodes), pharyngitis (4 episodes) and back pain (4 episodes). TEAEs were not dose-related. There were no relevant changes in vital signs, ECG parameters, laboratory tests or physical examinations. In the phase Ib clinical trial of olesoxime (125, 250 or 500 mg po, qd) plus riluzole (50 mg po, bid) in patients with ALS, all doses were well tolerated. There were 69 TEAEs reported, of which 2 were considered probably related, 13 possibly related, 21 unlikely to be related and 33 unrelated to olesoxime; the 2 considered probably related both occurred in the placebo group. Of the possibly related TEAEs, one occurred in the control group, six in the 125-mg group, three in the 250-mg group and three in the 500-mg group. The TEAEs were mild (n = 55), moderate (n = 13) or severe (n = 2) in intensity. The most frequently reported TEAEs were asthenia (12 episodes, 9 after olesoxime), diarrhea (6 episodes, 4 after olesoxime), muscle spasms (4 episodes, 3 after olesoxime) and constipation (3 episodes, 1 after olesoxime). The frequency, severity and duration of TEAEs were not dose-related. No relevant changes in vital signs, ECG parameters, laboratory tests or physical examinations were observed in any dose group. No safety issues were reported during the phase Ib clinical trial of olesoxime (125 mg po) in pediatric and adult patients with SMA, or during the 1-month follow-up period. |
| 参考文献 |
|
| 其他信息 |
Olesoxime is a cholesterol-like small molecule that has demonstrated a remarkable neuroprotective profile in a battery of both in vitro and in vivo preclinical models. For example, it has demonstrated the ability to prevent neurodegeneration, enhance nerve function and accelerate neuroregeneration following nerve trauma.
Drug Indication Investigated for use/treatment in neurologic disorders. Treatment of spinal muscular atrophy Mechanism of Action Olesoxime interacts with a physiologically relevant target: the mitochondrial permeability transition pore (mPTP). Mitochondria are central mediators of cell death and are implicated in most if not all neurodegenerative diseases regardless of the initiating factor: genetic mutations, excitotoxicity, reactive oxygen species, ischemia, chemical toxicity, etc. Mitochondria play diverse roles in all cells. In neurons, especially near synaptic sites, mitochondria are essential calcium-buffering organelles in areas where membrane excitability leads to large influx of calcium through calcium channels. Mitochondria also produce the ATP necessary for microtubule-based axoplasmic transport and maintaining the activity of ion and nutrient transporters. If a neuron fails to establish or maintain its functional role, mitochondria are responsible for eliminating it by releasing apoptotic factors. Olesoxime, by interacting with protein components of the mPTP, prevents the release of these apoptotic factors and therefore protects the neuron. This mechanism of action may lead to a general neuroprotective activity with utility in other therapeutic indications. Effective therapies are needed for amyotrophic lateral sclerosis (ALS), a debilitating and fatal motor neuron disease. Cell and animal models of ALS are beginning to reveal possible principles governing the biology of motor neuron-selective vulnerability that implicate mitochondria and the mitochondrial permeability pore (mPTP). Proteins associated with the mPTP are known to be enriched in motor neurons and the genetic deletion of a major regulator of the mPTP has robust effects in ALS transgenic mice, delaying disease onset and extending survival. Thus, the mPTP is a rational, mechanism-based target for the development of drugs designed to treat ALS. Trophos SA has discovered Olesoxime (TRO-19622), a small-molecule with a cholesterol-like structure, which has remarkable neuroprotective properties for motor neurons in cell culture and in rodents. Olesoxime appears to act on mitochondria, possibly at the mPTP. Phase I clinical trials of olesoxime have been completed successfully. Olesoxime is well tolerated and achieves levels predicted to be clinically effective when administered orally. It has been granted orphan drug status for the treatment of ALS in the US and for the treatment of spinal muscular atrophy in the EU. Phase II/III clinical trials are in progress in Europe.[1] The development of Olesoxime as a potential treatment for ALS is a major step forward for the field of MN disease. The rationale for the use of olesoxime in ALS is reasonably strong and mechanism-based. The theory behind targeting mitochondria and, specifically, the mPTP is based firmly on cell and animal model basic research. The specific targets of olesoxime have been suggested to be the TSPO and VDAC: TSPO is believed to be a modulator of the mPTP and VDAC is believed to be a dispensable component of the mPTP. Another study using a different TSPO ligand (Ro5–4864) demonstrated protection against neonatal MN cell death induced by axotomy, but no positive effects were noted in G93Ahigh-mSOD1 mice, suggesting that olesoxime binding to VDAC is perhaps the more therapeutically relevant interaction for neuroprotection against pathologic mPTP opening in adult MNs. The properties of olesoxime are propitious for a neurotherapeutic compound: it can be administered as an oral capsule, it passes the blood-brain barrier and it is well tolerated. However, more data are needed on the actions and safety of this compound on injured or damaged biological systems. More basic biological studies need to be undertaken to define the mechanisms of action of Olesoxime at subcellular and molecular levels. First, the identification of olesoxime as a drug acting on mitochondria needs to be established firmly. There are three isoforms of VDAC and some are at the plasma membrane and endoplasmic reticulum as well as on the OMM. If olesoxime does target mitochondria and does modulate the mPTP, then its actions on mitochondrial calcium retention need to be clarified. Alternatively, olesoxime could indirectly act on the mPTP by modulating mithochondrial ROS products. Furthermore, the types of cells that olesoxime protects need to be identified. For example, in vivo olesoxime could be exerting protective actions directly on MNs or it could be acting on microglia, astrocytes, Schwann cells or skeletal muscle cells to indirectly protect MNs. Patients with ALS desperately need an effective treatment for their disease. The exploration of olesoxime as a new small-molecule therapy offers hope. [1] Olesoxime (TRO19622) is a novel mitochondrial-targeted neuroprotective compound undergoing a pivotal clinical efficacy study in Amyotrophic Lateral Sclerosis (ALS) and also in development for Spinal Muscular Atrophy (SMA). It belongs to a new family of cholesterol-oximes identified for its survival-promoting activity on purified motor neurons deprived of neurotrophic factors. Olesoxime targets proteins of the outer mitochondrial membrane, concentrates at the mitochondria and prevents permeability transition pore opening mediated by, among other things, oxidative stress. Olesoxime has been shown to exert a potent neuroprotective effect in various in vitro and in vivo models. In particular olesoxime provided significant protection in experimental animal models of motor neuron disorders and more particularly ALS. Olesoxime is orally active, crosses the blood brain barrier, and is well tolerated. Collectively, its pharmacological properties designate olesoxime as a promising drug candidate for motor neuron diseases. [2] Amyotrophic lateral sclerosis (ALS) is a fatal neurodegenerative disorder characterized by progressive death of cortical and spinal motor neurons, for which there is no effective treatment. Using a cell-based assay for compounds capable of preventing motor neuron cell death in vitro, a collection of approximately 40,000 low-molecular-weight compounds was screened to identify potential small-molecule therapeutics. We report the identification of cholest-4-en-3-one, oxime (TRO19622) as a potential drug candidate for the treatment of ALS. In vitro, TRO19622 promoted motor neuron survival in the absence of trophic support in a dose-dependent manner. In vivo, TRO19622 rescued motor neurons from axotomy-induced cell death in neonatal rats and promoted nerve regeneration following sciatic nerve crush in mice. In SOD1(G93A) transgenic mice, a model of familial ALS, TRO19622 treatment improved motor performance, delayed the onset of the clinical disease, and extended survival. TRO19622 bound directly to two components of the mitochondrial permeability transition pore: the voltage-dependent anion channel and the translocator protein 18 kDa (or peripheral benzodiazepine receptor), suggesting a potential mechanism for its neuroprotective activity. TRO19622 may have therapeutic potential for ALS and other motor neuron and neurodegenerative diseases.[3] |
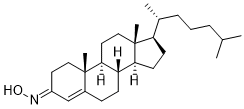
| 分子式 |
C27H45NO
|
|---|---|
| 分子量 |
399.6523
|
| 精确质量 |
399.35
|
| 元素分析 |
C, 81.14; H, 11.35; N, 3.50; O, 4.00
|
| CAS号 |
22033-87-0
|
| PubChem CID |
76971721
|
| 外观&性状 |
Typically exists as white to off-white solids at room temperature
|
| 密度 |
1.1
|
| 沸点 |
510ºC at 760mmHg
|
| 熔点 |
145-148ºC
|
| 闪点 |
341ºC
|
| 蒸汽压 |
1.56E-12mmHg at 25°C
|
| 折射率 |
1.583
|
| LogP |
7.858
|
| tPSA |
32.59
|
| 氢键供体(HBD)数目 |
1
|
| 氢键受体(HBA)数目 |
2
|
| 可旋转键数目(RBC) |
5
|
| 重原子数目 |
29
|
| 分子复杂度/Complexity |
663
|
| 定义原子立体中心数目 |
7
|
| SMILES |
C[C@@]12C(CC[C@]3([H])[C@]2([H])CC[C@@]4(C)[C@@]3([H])CC[C@@]4([C@]([H])(C)CCCC(C)C)[H])=CC(CC1)=NO
|
| InChi Key |
QNTASHOAVRSLMD-SIWSWZRQSA-N
|
| InChi Code |
InChI=1S/C27H45NO/c1-18(2)7-6-8-19(3)23-11-12-24-22-10-9-20-17-21(28-29)13-15-26(20,4)25(22)14-16-27(23,24)5/h17-19,22-25,29H,6-16H2,1-5H3/b28-21+/t19-,22+,23-,24+,25+,26+,27-/m1/s1
|
| 化学名 |
(8S,9S,10R,13R,14S,17R,E/Z)-10,13-dimethyl-17-((R)-6-methylheptan-2-yl)-1,2,6,7,8,9,10,11,12,13,14,15,16,17-tetradecahydro-3H-cyclopenta[a]phenanthren-3-one oxime
|
| 别名 |
E/Z-olesoxime; NSC 21311; NSC-21311; NSC21311; TRO-19622; TRO19622; TRO19622; RG6083; RG 6083; RG-6083;Olesoxime; Olesoxime, Z-; 22033-87-0; UNII-I2QN18P645; I2QN18P645; 66514-00-9; TRO 19622; (NE/Z)-N-[(8S,9S,10R,13R,14S,17R)-10,13-dimethyl-17-[(2R)-6-methylheptan-2-yl]-1,2,6,7,8,9,11,12,14,15,16,17-dodecahydrocyclopenta[a]phenanthren-3-ylidene]hydroxylamine;
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ~50 mg/mL (~125.11 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (6.26 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (6.26 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (6.26 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.5022 mL | 12.5109 mL | 25.0219 mL | |
| 5 mM | 0.5004 mL | 2.5022 mL | 5.0044 mL | |
| 10 mM | 0.2502 mL | 1.2511 mL | 2.5022 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
A double-blind, randomized, multi-center study with 500 mg QD of TRO19622 versus placebo in patients with painful peripheral diabetic neuropathy
CTID: null
Phase: Phase 2 Status: Completed
Date: