| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5mg |
|
||
| 10mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| Other Sizes |
|
| 靶点 |
DNA synthesis; DNA alkylation
|
||
|---|---|---|---|
| 体外研究 (In Vitro) |
体外活性:奥沙利铂的主要作用机制是通过 DNA 加合物的形成介导的。奥沙利铂诱导原发性和继发性 DNA 损伤,导致细胞凋亡。 Oxaliplatin 对人黑色素瘤细胞系 C32 和 G361 有活性,IC50 分别为 0.98 mM 和 0.14 mM。奥沙利铂有效抑制膀胱癌细胞系 RT4 和 TCCSUP、卵巢癌细胞系 A2780、结肠癌细胞系 HT-29、胶质母细胞瘤细胞系 U-373MG 和 U-87MG、以及黑色素瘤细胞系 SK-MEL-2 和 HT-144 IC50 分别为 11 μM、15 μM、0.17 μM、0.97 μM、2.95 μM、17.6 μM、30.9 μM 和 7.85 μM。细胞测定:细胞毒性研究通过磺基罗丹明-B 微量培养比色测定进行。通常,细胞(RT4、TCCSUP、A2780、HT-29、U-373MG、U-87MG、SK-MEL-2 和 HT-144 细胞系)在第 0 天接种到 96 孔板中,并在第 1 天暴露于奥沙利铂1;磺胺罗丹明-B 测定在奥沙利铂暴露后 48 小时进行。除添加奥沙利铂时和最后测定期间外,板始终在 37°C、5% CO2 和 100% 相对湿度下孵育。用于测定的初始铺板细胞数量范围为 2-20 × 103 细胞/50 /nL/孔。用于铺板的细胞数量和药物暴露时间基于初步研究,使用以下标准:(a) 对照孔中的细胞在测定当天仍处于对数生长期; (b) 测定当天未经处理的对照的最大吸光度在 1.0 至 1.5 范围内; (c) 细胞在药物暴露期间经历>2倍倍增。每个浓度使用八个孔。使用与 IBM PC 兼容计算机连接的 Biotek Instruments 型号 EL309 微孔板读板机在 570 和/或 540 nm 处读取板。通过计算机程序DATALOG将数据传输并转换为LOTUS 1-2-3格式,并通过比较处理的药物与对照来计算存活分数。
|
||
| 体内研究 (In Vivo) |
每周向携带 HCCLM3 肝细胞肿瘤的裸鼠腹膜内注射 10 mg/kg 奥沙利铂,可显着减少肿瘤体积和凋亡指数。奥沙利铂(5mg/kg,第 1、5 和 9 天静脉注射)对 T 白血病淋巴瘤 L40 AKR 有活性,T/C 为 1.77。奥沙利铂对脑内移植的 L1210 白血病、MA 16-C 异种移植物、B16 黑色素瘤异种移植物、Lewis 肺异种移植物和 C26 结肠癌异种移植物也有效。奥沙利铂会诱导小鼠逆行神经元运输受损。
假治疗时,TTc转运导致胸椎上的荧光信号强度在注射后0至60分钟增加。从0到60分钟,荧光信号平均增加了722%+/-117%(平均值+/-SD)。奥沙利铂治疗的动物在基线时具有可比的转运(787%+/-140%),但在整个研究过程中转运迅速下降,连续一周降至363%+/-88%、269%+/-96%、191%+/-58%、121%+/-39%、75%+/-21%,并在7周时稳定在57%(+/-15%)左右。在大约3周时出现了统计学上显著的差异(p≤0.05,线性混合效应回归模型)。具有恒定截止阈值的定量免疫荧光组织学显示,与对照组相比,治疗动物在7周时脊髓中的TTc降低(5.2任意单位+/-0.52 vs 7.1 AU+/-1.38,p<0.0004,T检验)。NeuN染色显示,两组神经细胞质量没有显著差异(10.2+/-1.21 vs 10.5 AU+/-1.53,p>0.56,T检验)。 结论:我们首次证明,神经影像学体内分子成像可以显示奥沙利铂诱导的神经病变模型的影像学变化。逆行神经转运受损被认为是奥沙利铂诱导的神经病变病理生理学的重要组成部分。[6] |
||
| 细胞实验 |
磺基罗丹明-B 微量培养比色测定用于进行细胞毒性研究。磺基罗丹明-B 测试通常在细胞(RT4、TCCSUP、A2780、HT-29、U-373MG、U-87MG、SK-MEL-2 和 HT-144 细胞系)接种到 96-在第 0 天对孔板进行培养,并在第 1 天暴露于奥沙利铂。除了添加奥沙利铂时和最终测定期间外,板始终在 37°C、5% CO2 和 100% 相对湿度下孵育。该测定从 2–20 × 103 个细胞/50 nL/孔铺在载玻片上开始。检测当天,对照孔中的细胞必须仍处于对数生长期;未经处理的对照的最大吸光度必须介于 1.0 和 1.5 之间;并且在药物暴露期间,细胞必须经历两次以上的倍增。这些标准基于试点研究。一个浓度由八个孔组成。使用 IBM PC 兼容计算机作为接口,使用 Biotek Instruments 型号 EL309 酶标仪在 570-540 nm 处读取板。计算机程序 DATALOG 传输数据并将其转换为 LOTUS 1-2-3 格式。比较治疗药物和对照药物以确定存活分数。
|
||
| 动物实验 |
|
||
| 药代性质 (ADME/PK) |
Absorption
The reactive oxaliplatin derivatives are present as a fraction of the unbound platinum in plasma ultrafiltrate. After a single 2-hour intravenous infusion of oxaliplatin at a dose of 85 mg/m2, pharmacokinetic parameters expressed as ultrafiltrable platinum was Cmax of 0.814 mcg/mL. Interpatient and intrapatient variability in ultrafiltrable platinum exposure (AUC0-48hr) assessed over 3 cycles was 23% and 6%, respectively. Route of Elimination The major route of platinum elimination is renal excretion. At five days after a single 2-hour infusion of ELOXATIN, urinary elimination accounted for about 54% of the platinum eliminated, with fecal excretion accounting for only about 2%. Volume of Distribution After a single 2-hour intravenous infusion of oxaliplatin at a dose of 85 mg/m2, the volume of distribution is 440 L.At the end of a 2-hour infusion, approximately 15% of the administered platinum is present in the systemic circulation. The remaining 85% is rapidly distributed into tissues or eliminated in the urine. Clearance Platinum was cleared from plasma at a rate (10-17 L/h) that was similar to or exceeded the average human glomerular filtration rate (GFR; 7.5 L/h). The renal clearance of ultrafiltrable platinum is significantly correlated with GFR. Metabolism / Metabolites Oxaliplatin undergoes rapid and extensive nonenzymatic biotransformation. There is no evidence of cytochrome P450-mediated metabolism in vitro. Up to 17 platinum-containing derivatives have been observed in plasma ultrafiltrate samples from patients, including several cytotoxic species (monochloro DACH platinum, dichloro DACH platinum, and monoaquo and diaquo DACH platinum) and a number of noncytotoxic, conjugated species. Biological Half-Life The decline of ultrafilterable platinum levels following oxaliplatin administration is triphasic with two distribution phases: t1/2α; 0.43 hours and t1/2β; 16.8 hours. This is followed by a long terminal elimination phase that lasts 391 hours (t1/2γ). |
||
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
Mild and transient elevations in serum aminotransferase levels are found in an appreciable proportion of patients taking oxaliplatin, but their relationship to oxaliplatin is often unclear. Chemotherapy with oxaliplatin has been associated with histological changes in the liver marked by sinusoidal dilatation, congestion and centrolobular necrosis indicative of sinusoidal obstruction syndrome. These changes are usually mild-to-moderate in severity and not clinically significant during the acute phase, but they can progress to clinically apparent sinusoidal obstruction syndrome or, with chronic therapy, to nodular regenerative hyperplasia with splenomegaly, thrombocytopenia and esophageal varices. Nodular regenerative hyperplasia typically requires 6 to 18 months to develop and arises after repeated cycles of chemotherapy with oxaliplatin. Serum enzyme and bilirubin elevations are minimal, the major laboratory finding being a progressive and persistent thrombocytopenia reflecting the development of splenomegaly and portal hypertension. The first clinical evidence of nodular regenerative hyperplasia may be ascites, esophageal variceal hemorrhage or hepatic encephalopathy. Attempts at hepatic resection, severe gastrointestinal bleeding and septicemia may trigger hepatic decompensation and liver failure. Interestingly, nodular regenerative hyperplasia and portal hypertension tend to improve slowly once chemotherapy is stopped, but the long term consequences of the changes are not well defined. Likelihood score: A (well established cause of clinically apparent liver injury). Protein Binding In patients, plasma protein binding of platinum is irreversible and is greater than 90%. The main binding proteins are albumin and gamma-globulins. Platinum also binds irreversibly and accumulates (approximately 2-fold) in erythrocytes, where it appears to have no relevant activity. No platinum accumulation was observed in plasma ultrafiltrate following 85 mg/m2 every two weeks. |
||
| 参考文献 | |||
| 其他信息 |
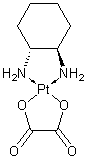
An organoplatinum complex in which the platinum atom is complexed with 1,2-diaminocyclohexane, and with an oxalate ligand which is displaced to yield active oxaliplatin derivatives. These derivatives form inter- and intra-strand DNA crosslinks that inhibit DNA replication and transcription. Oxaliplatin is an antineoplastic agent that is often administered with FLUOROURACIL and FOLINIC ACID in the treatment of metastatic COLORECTAL NEOPLASMS.
See also: Oxaliplatin (annotation moved to). Of the new generation platinum compounds that have been evaluated, those with the 1,2-diaminocyclohexane carrier ligand-including oxaliplatin--have been focused upon in recent years. Molecular biology studies and the National Cancer Institute in vitro cytotoxic screening showed that diaminocyclohexane platinums such as oxaliplatin belong to a distinct cytotoxic family, differing from cisplatin and carboplatin, with specific intracellular target(s), mechanism(s) of action and/or mechanism(s) of resistance. In phase I trials, the dose-limiting toxicity of oxaliplatin was characterized by transient acute dysesthesias and cumulative distal neurotoxicity, which was reversible within a few months after treatment discontinuation. Moreover, oxaliplatin did not display any, auditory, renal and hematologic dose-limiting toxicity at the recommended dose of 130 mg/m2 q three weeks or 85 mg/m2 q two weeks given as a two-hour i.v. infusion. Clinical phase II experiences on the antitumoral activity of oxaliplatin have been conducted in hundreds of patients with advanced colorectal cancers (ACRC). Single agent activity reported as objective response rate in ACRC patients is 10% and 20% overall in ACRC patients with 5-fluorouracil (5-FU) pretreated/refractory and previously untreated ACRC, respectively. Synergistic cytotoxic effects in preclinical studies with thymidylate synthase inhibitors, cisplatin/carboplatin and topoisomerase I inhibitors, and the absence of hematologic dose-limiting toxicity have made oxaliplatin an attractive compound for combinations. Phase II trials combining oxaliplatin with 5-FU and folinic acid ACRC patients previously treated/refractory to 5-FU showed overall response rates ranging from 21% to 58%, and survivals ranging from 12 to 17 months. In patients with previously untreated ACRC, combinations of oxaliplatin with 5-FU and folinic acid showed response rates ranging from 34% to 67% and median survivals ranging from 15 to 19 months. Two randomized trials totaling 620 previously untreated patients with ACRC, comparing 5-FU and folinic acid to the same regimen with oxaliplatin, have shown a 34% overall response rate in the oxaliplatin group versus 12% in the 5-FU/folinic acid group for the first trial; and 51.2% vs. 22.6% in the second one. These statistically significant differences were confirmed in time to progression advantage for the oxaliplatin arm (8.7 vs. 6.1 months, and 8.7 vs. 6.1 months, respectively). A small but consistent number of histological complete responses have been reported in patients with advanced colorectal cancer treated with the combination of oxaliplatin with 5-FU/folinic acid, and secondary metastasectomy is increasingly done by oncologists familiar with the combination. Based on preclinical and clinical reports showing additive or synergistic effects between oxaliplatin and several anticancer drugs including cisplatin, irinotecan, topotecan, and paclitaxel, clinical trials of combinations with other compounds have been performed or are still ongoing in tumor types in which oxaliplatin alone showed antitumoral activity such as ovarian, non-small-cell lung, breast cancer and non-Hodgkin lymphoma. Its single agent and combination therapy data in ovarian cancer confirm its non-cross resistance with cisplatin/carboplatin. While the role of oxaliplatin in medical oncology is yet to be fully defined, it appears to be an important new anticancer agent.[1] We have previously confirmed the in vitro activity of cisplatin and carboplatin against human melanoma cell lines. Both drugs are important components in the chemotherapy used in our service for advanced metastatic melanoma. In this communication we report the in vitro activity of oxaliplatin against human melanoma cell lines in comparison with cisplatin and carboplatin. Oxaliplatin was found to be active against C32 and G361 cell lines with IC50 values of 49.48 and 9.07 microM (1 h exposure), 9.47 and 1.30 microM (4 h exposure), and 0.98 and 0.14 microM (24 h exposure), respectively. The cytotoxic activity of oxaliplatin in this in vitro system appears to be significantly superior to that of carboplatin. Its activity becomes comparatively closer to that of cisplatin as exposure time increases. Indeed at a 24 h exposure oxaliplatin appears to be significantly more active than cisplatin against the G361 cell line (p=0.0343). Oxaliplatin merits evaluation in the clinic both as a single agent and in combination with other drugs active against melanoma.[2] The in vitro cytotoxicity, protein binding, partitioning of platinum from whole blood into erythrocytes, its exchange back into plasma, and the in vitro biotransformation in plasma were studied for the new nonnephrotoxic platinum analogue oxaliplatin. The cytotoxicity studies were carried out against a panel of human tumor cell lines derived from carcinomas of the ovary (A2780, A2780/cp), bladder (TCCSUP, RT4), colon (HT-29), melanoma (SKMEL-2, HTB144), and glioma (U373MG and U87MG). The relative potency of the five platinum complexes was oxaliplatin = tetraplatin > cisplatin > iproplatin > carboplatin. Oxaliplatin was active against HT-29 and only minimally cross-resistant with cisplatin against A2780/cp. Both bladder carcinoma cell lines, both melanoma cell lines, and one of the two glioblastoma cell lines were resistant to both oxaliplatin and tetraplatin. The cytotoxicity profiles of the drug pairs oxaliplatin-tetraplatin and cisplatin-carboplatin showed statistically significant correlation by the Spearman rank correlation test. Oxaliplatin was similar to cisplatin and tetraplatin in protein binding; 85-88% of all platinum from oxaliplatin (5, 10, or 20 micrograms/ml) was bound to plasma proteins within the first 5 h with an average half-life of 1.71 +/- 0.06 h. When oxaliplatin was incubated in whole blood (5, 10, and 20 micrograms/ml), the erythrocytes took up 37.1 +/- 2.1% of the total platinum in 2 h (maximum uptake) which was not exchangeable into plasma. Thus the erythrocyte-bound fraction does not serve as a reservoir of drug. In plasma, oxaliplatin was unchanged at 0.5 h, but at 1 h, 30% of the total platinum in plasma was in a peak which had identical retention to that of (trans-1,2-diaminocyclohexane)dichloroplatinum(II), the major biotransformation product of tetraplatin. At 2 h, (trans-1,2-diaminocyclohexane)dichloroplatinum(II) and three other platinum-containing peaks were detected but no unchanged oxaliplatin. All the platinum eluted in a single peak near the solvent front at 4 h. The marked similarity in cytotoxicity between oxaliplatin and tetraplatin may be due to the formation of (trans-1,2-diaminocyclohexane)dichloroplatinum(II) in tissue culture media.[3] Objective: The platinum-based chemotherapeutic agent oxaliplatin displays a wide range of antitumor activities. To date, no detailed data are available about the effects of oxaliplatin on hepatocellular carcinoma (HCC) cells. Herein, the anti-proliferation effects of oxaliplatin on HCCLM3 and Hep3B cells in vitro and in vivo are studied. Research methods: Cell viability was assessed by an MTT assay and apoptosis by flow cytometry and transmission electron microscopy. Apoptosis-related proteins in HCCLM3 cells were evaluated by microarray analysis, quantitative reverse transcriptase-PCR assay and western blotting. The effect of oxaliplatin was also studied in vivo using a xenograft model. Results: Oxaliplatin inhibited the growth of HCCLM3 and Hep3B cells. Using flow cytometry, transmission electron microscopy and the terminal deoxynucleotidyl transferase-mediated dUTP nick end labeling assay, we found that apoptosis was the main mechanism by which oxaliplatin inhibited tumor progression. Microarray analysis, quantitative reverse transcriptase-PCR and western blot analysis further demonstrated downregulation of the anti-apoptotic proteins Bcl-2 and Bcl-xL and upregulation of the pro-apoptotic protein Bax during oxaliplatin-induced apoptosis. Conclusions: The anti-proliferation effect of oxaliplatin in HCC cells is due to induction of apoptosis. Therefore, oxaliplatin may be an effective treatment for HCC and its use merits further in-depth investigation.[4] A new platinum complex, oxalatoplatin or l-OHP, which, at the same metal dose in experimental tests is as efficient as cisplatin, and is more so at a lower metal dose than carboplatin; which is as efficient in human tumors of the testis and ovary as these other analogs, and more so in melanoma and breast cancer; which is not nephrotoxic, cardiotoxic or mutagenic, and hardly hematotoxic and neurotoxic, is described and compared with the above-mentioned platinum complexes. Combined with 5Fu, it induces a high number of remissions in colorectal cancer, and has brought about cures in inoperable gastric cancers. Combined with carboplatin, it has resulted in a high proportion of cures in L1210-carrying mice, which no other two-by-two combination of these complexes has achieved.[5] Colon cancer is one of the most common malignancies in the world. Oxaliplatin, a third-generation platinum compound, is widely used in clinical chemotherapy of colon cancer. Although the mechanisms of the antitumor effect of Oxaliplatin have been investigated in recent years, the proteomic changes that are associated with the cellular response to this compound are poorly understood. In this study, we performed a comparative proteomic analysis to survey the global changes in protein expression levels after Oxaliplatin treatment in three colon cancer cell lines: HT29, SW620, and LoVo. Two-dimensional gel electrophoresis coupled with MALDI-TOF/TOF mass spectrometry revealed 57, 48, and 53 differentially expressed proteins in the three cell lines (HT29, SW620 and LoVo, respectively) after Oxaliplatin treatment. Of these proteins, 21 overlapped among all three cell lines. These overlapping proteins participate in many cellular processes, such as apoptosis, signal transduction, transcription and translation, cell structural organization, and metabolism. Additionally, the expression levels of ezrin (EZRI), heat-shock protein beta-1 (HSPB1), translationally controlled tumor protein (TCTP), and cell division control protein 2 homolog (CDC2) were confirmed by immunoblotting. This is the first direct proteomic analysis of Oxaliplatin-treated colon cancer cells. Several interesting proteins that we found warrant further investigation owing to their potential significant functions in the antitumor effect of Oxaliplatin.[8] |
| 分子式 |
C8H14N2O4PT
|
|
|---|---|---|
| 分子量 |
397.29
|
|
| 精确质量 |
397.06
|
|
| 元素分析 |
C, 24.19; H, 3.55; N, 7.05; O, 16.11; Pt, 49.10
|
|
| CAS号 |
61825-94-3
|
|
| 相关CAS号 |
|
|
| PubChem CID |
9887053
|
|
| 外观&性状 |
White solid powder
|
|
| 沸点 |
193.6ºC at 760 mmHg
|
|
| LogP |
0.614
|
|
| tPSA |
104.64
|
|
| 氢键供体(HBD)数目 |
4
|
|
| 氢键受体(HBA)数目 |
6
|
|
| 可旋转键数目(RBC) |
0
|
|
| 重原子数目 |
15
|
|
| 分子复杂度/Complexity |
191
|
|
| 定义原子立体中心数目 |
2
|
|
| SMILES |
[Pt+2].[O-]C(C(=O)[O-])=O.N([H])([H])[C@]1([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])[C@@]1([H])N([H])[H]
|
|
| InChi Key |
DRMCATBEKSVAPL-BNTLRKBRSA-N
|
|
| InChi Code |
InChI=1S/C6H12N2.C2H2O4.Pt/c7-5-3-1-2-4-6(5)8;3-1(4)2(5)6;/h5-8H,1-4H2;(H,3,4)(H,5,6);/q-2;;+2/t5-,6-;;/m1../s1
|
|
| 化学名 |
[(1R,2R)-2-azanidylcyclohexyl]azanide;oxalic acid;platinum(2+)
|
|
| 别名 |
L-OHP; diaminocyclohexane oxalatoplatinum; oxalatoplatin; oxalatoplatinum; DTXSID0036760; Oxalato(trans-l-1,2-cyclohexanediamine)platinum(II); cis-oxalato-trans-l-1,2-diaminocyclohexaneplatinum(II); US brand name: Eloxatin Foreign brand names: Dacotin; Dacplat; Eloxatine; Abbreviations: 1OHP; LOHP; Code names: JM83; RP54780; SR96669.
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 本产品在运输和储存过程中需避光。 |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
Note: Oxaliplatin一般不用DMSO溶解,因为铂类药物在DMSO中易失活!另外, Oxaliplatin在溶液中不稳定,请现配现用!
配方 1 中的溶解度: 1.92 mg/mL (4.83 mM) in PBS (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶。 (<60°C). 配方 2 中的溶解度: 3.33 mg/mL (8.38 mM) in 5% w/v Glucose Solution (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶. 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.5171 mL | 12.5853 mL | 25.1705 mL | |
| 5 mM | 0.5034 mL | 2.5171 mL | 5.0341 mL | |
| 10 mM | 0.2517 mL | 1.2585 mL | 2.5171 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Study of Pembrolizumab (MK-3475) Versus Chemotherapy in Chinese Participants With Stage IV Colorectal Cancer (MK-3475-C66)
CTID: NCT05239741
Phase: Phase 3 Status: Recruiting
Date: 2024-12-02
|
|---|