| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| 10g |
|
||
| Other Sizes |
|
| 体外研究 (In Vitro) |
奥卡西平显着抑制胶质母细胞瘤细胞的生长,在治疗剂量下可达到 IC50。在 U87 和 T98 细胞系中进行奥卡西平筛选,IC50 值分别为 12.35 和 9.45 μg/mL[2]。
|
|---|---|
| 体内研究 (In Vivo) |
奥卡西平已被证明可以保护小鼠和大鼠免受休克引起的全身强直阵挛性癫痫发作,口服 ED50 值范围为 13.5 至 20.5 mg/kg。连续四个星期每天给予奥卡西平的老鼠没有表现出对这种抗惊厥作用的耐受迹象。
|
| 细胞实验 |
细胞活力测定 [2]
细胞类型:人胶质瘤细胞系 U-87 MG 和 T98G 测试浓度:2.5、5、10、20 和40 μg/mL 孵育时间:72小时 实验结果:对T98G细胞系的生长抑制 每个浓度为17.7 ±4.1% (2.5 μg/mL)、21.1±3.6% (5 μg/mL)、53.6±14.2% (10 μg/mL)、82.2±2.3% (20 μg/mL) 和 85.0± 2.3% (40 μg/mL) /毫升)。各浓度对U-87 MG细胞系的生长抑制作用分别为-1.7±5.1%(0.008 μg/mL)、5.3±2.4%(0.08 μg/mL)、3.5±7.4%(0.8 μg/mL)、0.3± 9.2%(16微克/毫升)和-4.2±9.6%(40微克/毫升)。 |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Oxcarbazepine is completely absorbed following oral administration. A single 600mg dose of oxcarbazepine resulted in an MHD Cmax of 34 μmol/L and a median Tmax of 4.5 hours. When administered twice daily, steady-state levels of MHD are attained within 2-3 days. The rate and extent of absorption of oxcarbazepine is not affected by food intake. Following oral administration, more than 95% of the administered dose of oxcarbazepine is found in the urine. Of this, approximately 49% is MHD glucuronide metabolites, 27% is unchanged MHD, 3% is inactive DHD metabolites, 13% is conjugated oxcarbazepine, and less than 1% is unchanged parent drug. Fecal elimination accounts for only 4% of the administered dose. The apparent volume of distribution of oxcarbazepine is 49 L. The apparent volumes of distribution of (S)- and (R)-MHD were found to be 23.6 L and 31.7 L, respectively. Plasma clearance of oxcarbazepine has been estimated to be approximately 84.9 L/h, whereas plasma clearance of its active metabolite, MHD, was estimated to be 2.0 L/h. Rapid metabolic clearance appears to be the main pathway for oxcarbazepine, while clearance of its metabolites occurs mainly via renal excretion. Oxcarbazepine is completely absorbed. Food does not alter the rate and extent of absorption of oxcarbazepine. Both oxcarbazepine and its active 10-monohydroxy metabolite (MHD) are distributed into milk in humans. Elimination: Renal: greater than 95%, with more than 99% of the dose excreted in the form of metabolites. Fecal: less than 4%. Oxcarbazepine is an antiepileptic drug with a chemical structure similar to carbamazepine, but with different metabolism. Oxcarbazepine is rapidly reduced to 10,11-dihydro-10-hydroxy-carbazepine (monohydroxy derivative, MHD), the clinically relevant metabolite of oxcarbazepine. MHD has (S)-(+)- and the (R)-(-)-enantiomer, but the pharmacokinetics of the racemate are usually reported. The bioavailability of the oral formulation of oxcarbazepine is high (>95%). It is rapidly absorbed after oral administration, reaching peak concentrations within about 1-3 hours after a single dose, whereas the peak of MHD occurs within 4-12 hours. At steady state, the peak of MHD occurs about 2-4 hours after drug intake. The plasma protein binding of MHD is about 40%. Cerebrospinal fluid concentrations of MHD are in the same range as unbound plasma concentrations of MHD. Oxcarbazepine can be transferred significantly through the placenta in humans. Oxcarbazepine and MHD exhibit linear pharmaco-kinetics and no autoinduction occurs. ... For more Absorption, Distribution and Excretion (Complete) data for OXCARBAZEPINE (9 total), please visit the HSDB record page. Metabolism / Metabolites Oxcarbazepine is rapidly and extensively metabolized to its primary metabolite, MHD, which is responsible for the bulk of its anti-epileptic activity and exists in much higher concentrations in the plasma than the parent drug. MHD is formed via reduction by several members of the aldo-keto reductase family of cytosolic liver enzymes and exists as a racemate in plasma in an approximate ratio of 80% (S)-MHD to 20% (R)-MHD. MHD is further metabolized to glucuronide conjugate metabolites for excretion, and small amounts are oxidized to 10-,11-dihydro-10,11-dihydroxycarbamazepine (DHD) which is pharmacologically inactive. Only 10% of an administered dose of oxcarbazepine will remain as either the parent drug or glucuronide conjugates of the parent drug. Oxcarbazepine is rapidly reduced by cytosolic enzymes in the liver to its 10-monohydroxy metabolite, MHD, which is primarily responsible for the pharmacological effect of Trileptal. MHD is metabolized further by conjugation with glucuronic acid. Minor amounts (4% of the dose) are oxidized to the pharmacologically inactive 10,11-dihydroxy metabolite (DHD). Oxcarbazepine is cleared from the body mostly in the form of metabolites which are predominantly excreted by the kidneys. More than 95% of the dose appears in the urine, with less than 1% as unchanged oxcarbazepine. Fecal excretion accounts for less than 4% of the administered dose. Approximately 80% of the dose is excreted in the urine either as glucuronides of MHD (49%) or as unchanged MHD (27%); the inactive DHD accounts for approximately 3% and conjugates of MHD and oxcarbazepine account for 13% of the dose. The disposition of the new anti-epileptic agent oxcarbazepine (10,11-dihydro-10-oxo-5H-dibenz[b,f]azepine-5-carboxamide) has been studied in two healthy volunteers following an oral 400 mg dose of (14)C-labelled drug. The dose was excreted almost completely in the urine (94.6 and 97.1%) within six days. Fecal excretion amounted to 4.3 and 1.9% of the dose in the two subjects. In the 0-6 days urine samples the biotransformation products have been isolated and identified. 10,11-Dihydro-10-hydroxycarbamazepine (GP 47,779) and its two diastereoisomeric O-glucuronides were found as main metabolites. Taken together, they accounted for 79% of urinary (14)C. Unchanged oxcarbazepine, and its sulfate and glucuronide conjugates were isolated in smaller amounts only (13%). Other minor metabolites were the trans- and cis-isomers of 10,11-dihydro-10,11-dihydroxy-carbamazepine (approximately 4%), and a phenolic derivative of GP 47,779 (less than 1%). The biotransformation of oxcarbazepine proceeds mainly by reduction to GP 47,779, and subsequent conjugation with glucuronic acid. Reduction is stereospecific, favoring the S-configuration of GP 47,779. Direct conjugation of oxcarbazepine, in the enol form, is a minor pathway. Oxidative reactions are unimportant. ... The interaction potential of oxcarbazepine is relatively low. However, enzyme-inducing antiepileptic drugs such as phenytoin, phenobarbital or carbamazepine can reduce slightly the concentrations of 10,11-dihydro-10-hydroxy-carbazepine (monohydroxy derivative, MHD). Verapamil may moderately decrease MHD concentrations, but this effect is probably without clinical relevance. The influence of oxcarbazepine on other antiepileptic drugs is not clinically relevant in most cases. However, oxcarbazepine appears to increase concentrations of phenytoin and to decrease trough concentrations of lamotrigine and topiramate. Oxcarbazepine lowers concentrations of ethinylestradiol and levonorgestrel, and women treated with oxcarbazepine should consider additional contraceptive measures. Due to the absent or lower enzyme-inducing effect of oxcarbazepine, switching from carbamazepine to oxcarbazepine can result in increased serum concentrations of comedication, sometimes associated with adverse effects. ... Oxcarbazepine is completely absorbed and extensively metabolized to its pharmacologically active 10-monohydroxy metabolite (MHD) by cytosolic enzymes. MHD is metabolized further by conjugation with glucuronic acid. Route of Elimination: Oxcarbazepine is cleared from the body mostly in the form of metabolites which are predominantly excreted by the kidneys. Fecal excretion accounts for less than 4% of the administered dose. Half Life: The half-life of the parent is about 2 hours, while the half-life of MHD is about 9 hours, so that MHD is responsible for most anti-epileptic activity. Biological Half-Life The plasma half-life of oxcarbazepine is approximately 2 hours and the plasma half-life of MHD is approximately 9 hours. Oxcarbazepine: 2 hours. 10-Monohydroxy metabolite: 9 hours. Note: In patients with renal function impairment with a creatinine clearance < 30 mL/minute, the half life of 10 monohydroxy metabolite is prolonged to 10 hours ... ... Elimination half-lives in healthy volunteers are 1-5 hours for oxcarbazepine and 7-20 hours for 10,11-dihydro-10-hydroxy-carbazepine (monohydroxy derivative, MHD). Longer and shorter elimination half-lives have been reported in elderly volunteers and children, respectively. ... |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
The exact mechanism by which oxcarbazepine exerts its anticonvulsant effect is unknown. It is known that the pharmacological activity of oxcarbazepine occurs primarily through its 10-monohydroxy metabolite (MHD). In vitro studies indicate an MHD-induced blockade of voltage-sensitive sodium channels, resulting in stabilization of hyperexcited neuronal membranes, inhibition of repetitive neuronal discharges, and diminution of propagation of synaptic impulses. Interactions Oxcarbazepine may induce metabolism of some calcium-channel blocking agents (e.g., felodipine, verapamil), possibly via induction of CYP3A4 and CYP3A5 isoenzymes, resulting in decreased AUC of the calcium-channel blocking agents. Oxcarbazepine may induce metabolism of oral estrogen-progestin contraceptives, possibly via induction of CYP3A4 and CYP3A5, resulting in decreased area under the plasma concentration-time curve (AUC) and consequent decreased efficacy of the contraceptives. Oxcarbazepine may inhibit metabolism of other anticonvulsants (e.g., phenobarbital, phenytoin), possibly via inhibition of the cytochrome P-450 (CYP) isoenzyme 2C19, resulting in increased plasma concentrations of these drugs. Oxcarbazepine dosages exceeding 1200 mg daily may increase plasma phenytoin concentrations by 40% and, therefore, when such dosages of oxcarbazepine are used concomitantly with phenytoin, dosage reduction of phenytoin may be required. Potent inducers of CYP isoenzymes (e.g., carbamazepine, phenytoin, phenobarbital) may decrease plasma concentrations of oxcarbazepine and its active 10-monohydroxy metabolite (MHD). Oxcarbazepine and its 10-monohydroxy metabolite may increase the concentration of phenobarbital by about 14%; at oxcarbazepine doses above 1200 mg a day; phenytoin concentrations may be increased by about 40%. For more Interactions (Complete) data for OXCARBAZEPINE (6 total), please visit the HSDB record page. |
| 参考文献 |
|
| 其他信息 |
Therapeutic Uses
Oxcarbazepine is indicated for monotherapeutic or adjunctive therapeutic use in the treatment of partial seizures in adults and children ages 4 to 16 with epilepsy. /Included in US product labeling/ /EXPL THER:/ ... Oxcarbazepine /was compared/ with acamprosate in relapse prevention in recently withdrawn alcohol-dependent patients. /They/ investigated the efficacy and safety of oxcarbazepin (vs acamprosate) by conducting a 24-week randomized, parallel-group, open-label, clinical trial on 30 acutely detoxified alcoholic patients. Survival analyses (Kaplan-Meier) were performed to look for evidence of a longer "survival" of patients receiving oxcarbazepine. ... After withdrawal, time to severe relapse and time to first consumption of any ethanol by oxcarbazepin patients were not longer than for acamprosate patients. Abstinent patients in both study groups showed a significantly lower obsessive compulsive drinking scale-German version (OCDS-G) than relapsed patients. No undesired effects occurred when oxcarbazepin patients consumed alcohol. ... It is noteworthy that oxcarbazepine is well tolerated, even when alcohol is on board. ... /EXPL THER:/ ... Data related to 150 patients harboring supratentorial brain gliomas with the aim to assess the efficacy of oxcarbazepine in preventing the occurrence or the recurrence of early postoperative seizures and its tolerability when it is rapidly titrated /was analyzed/. Only four patients (2.7%) experienced seizures within the first week after surgery. Patients did not report disturbances during the titration phase. Regarding adverse events in the first week, six patients (4%) showed minor skin rash. Persistent symptomatic hyponatremia never occurred. ... Oxcarbazepine can be a good alternative to traditional antiepileptic agents in the prevention of perioperative seizures being efficacy, ease of use (rapid titration in 3 days, not requiring close plasma concentration monitoring) and good tolerability (no major side effects during titration and during the first postoperative week) the key factors. Moreover, oxcarbazepine can be a valid choice when long-term therapy is required because of the low interaction with other drugs and the low hematological side effects. Drug Warnings Multiorgan hypersensitivity reactions occurring days to weeks or months (range 4-60 days) after initiation of oxcarbazepine therapy have been reported in adults and pediatric patients. Although these reactions have been reported rarely, many of these patients required hospitalization, and some reactions were considered life-threatening. Manifestations may include (but are not limited to) fever, rash, lymphadenopathy, hepatitis, abnormal liver function test results, eosinophilia, thrombocytopenia, neutropenia, pruritus, nephritis, oliguria, hepatorenal syndrome, arthralgia, and asthenia. While severe hyponatremia is reported to be more frequent in adults treated with oxcarbazepine than with carbamazepine, there is not sufficient data about the incidence of hyponatremia in childhood during treatment with oxcarbazepine. ... Changes in serum electrolyte balance in 75 children with epilepsy before and during treatment with oxcarbazepine and after replacing carbamazepine therapy with oxcarbazepine therapy /were evaluate/. All patients had normal sodium serum levels at the onset of oxcarbazepine. During treatment with oxcarbazepine ... hyponatremia (Na +< 135 mmol/L) without clinical symptoms /were found/ in 26.6 % of the children (n = 20), /and/ sodium levels below 125 mmol/L were observed in 2 children (2.6 %). Clinically relevant hyponatremia occurred in one girl only (1.3 %). In a subgroup of 27 children, in whom carbamazepine was directly replaced with oxcarbazepine, hyponatremia without symptoms was found in one child under carbamazepine (3.7 %) and in six children under oxcarbazepine (22.2 %). Dosage of oxcarbazepine, serum levels of the active metabolite of oxcarbazepine, antiepileptic comedication or patients' age and gender were of no predictive value for the development of hyponatremia. ... Adverse effects occurring in 5% or more of patients and more frequently than placebo include dizziness, somnolence, diplopia, fatigue, nausea, vomiting, ataxia, abnormal vision, abdominal pain, tremor, dyspepsia, abnormal gait. Serious dermatologic reactions, including Stevens-Johnson syndrome and toxic epidermal necrolysis, have been reported in adults and children receiving oxcarbazepine; reactions have been life-threatening, have required hospitalization, and rarely have been fatal. The incidence of Stevens-Johnson syndrome and toxic epidermal necrolysis reported in patients receiving oxcarbazepine exceeds the rate in the general population by threefold to tenfold. The median time to onset of these reactions was 19 days. Recurrence of serious dermatologic reactions following rechallenge with oxcarbazepine has occurred. For more Drug Warnings (Complete) data for OXCARBAZEPINE (11 total), please visit the HSDB record page. Pharmacodynamics Oxcarbazepine is an anticonvulsant drug that reduces the incidence of seizures in epilepsy by inhibiting abnormal electrical activity in the brain. There have been rare reports of oxcarbazepine resulting in the development of hematologic abnormalities, including agranulocytosis and aplastic anemia. Patients should be undergo frequent laboratory testing and should be monitored closely for signs and symptoms of blood dyscrasias. Oxcarbazepine has also been associated with the development of dermatologic reactions which can progress from a simple rash to potentially fatal reactions such as toxic epidermal necrolysis (TEN) or Stevens-Johnson Syndrome (SJS). Patients with the HLA-A 3101 and/or HLA-B 1502 alleles may be at higher risk of this reaction. Oxcarbazepine should be discontinued at the first sign of a drug-induced skin reaction. |
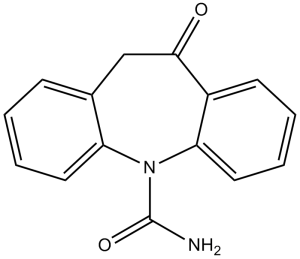
| 分子式 |
C15H12N2O2
|
|
|---|---|---|
| 分子量 |
252.27
|
|
| 精确质量 |
252.089
|
|
| CAS号 |
28721-07-5
|
|
| 相关CAS号 |
Oxcarbazepine-d4;1020719-71-4;Oxcarbazepine-d4-1;1134188-71-8
|
|
| PubChem CID |
34312
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 密度 |
1.3±0.1 g/cm3
|
|
| 沸点 |
457.2±55.0 °C at 760 mmHg
|
|
| 熔点 |
215-216°C
|
|
| 闪点 |
230.3±31.5 °C
|
|
| 蒸汽压 |
0.0±1.1 mmHg at 25°C
|
|
| 折射率 |
1.662
|
|
| LogP |
1.44
|
|
| tPSA |
63.4
|
|
| 氢键供体(HBD)数目 |
1
|
|
| 氢键受体(HBA)数目 |
2
|
|
| 可旋转键数目(RBC) |
0
|
|
| 重原子数目 |
19
|
|
| 分子复杂度/Complexity |
382
|
|
| 定义原子立体中心数目 |
0
|
|
| InChi Key |
QZAQRPLWHYVQMM-UHFFFAOYSA-N
|
|
| InChi Code |
InChI=1S/C15H12N2O2/c16-15(18)12-9-10-5-1-3-7-13(10)17(19)14-8-4-2-6-11(12)14/h1-6,8-9H,7H2,(H2,16,18)
|
|
| 化学名 |
5-oxo-6H-benzo[b][1]benzazepine-11-carboxamide
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 1.67 mg/mL (6.62 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 16.7 mg/mL澄清的DMSO储备液加入到400 μL PEG300中,混匀;再向上述溶液中加入50 μL Tween-80,混匀;然后加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 1.67 mg/mL (6.62 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 16.7 mg/mL 澄清 DMSO 储备液加入到 900 μL 玉米油中并混合均匀。 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 3.9640 mL | 19.8200 mL | 39.6401 mL | |
| 5 mM | 0.7928 mL | 3.9640 mL | 7.9280 mL | |
| 10 mM | 0.3964 mL | 1.9820 mL | 3.9640 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Longitudinal Comparative Effectiveness of Bipolar Disorder Therapies
CTID: NCT02893371
Phase: Status: Terminated
Date: 2024-03-12