| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg | |||
| Other Sizes |
| 靶点 |
HDAC1 ( Ki = 7 nM ); HDAC3/SMRT ( Ki = 8.2 nM ); HDAC6 ( Ki = 17 nM ); HDAC2 ( Ki = 19 nM ); HDAC10 ( Ki = 24 nM ); HDAC8 ( Ki = 280 nM ); MBLAC2 ( Ki < 10 nM )
|
|---|---|
| 体外研究 (In Vitro) |
体外活性:PCI-24781 对多种肿瘤细胞系表现出有效的抗肿瘤活性,GI50 范围为 0.15 μM 至 3.09 μM。 PCI-24781 对 HUVEC 内皮细胞也具有抗增殖作用,GI50 为 0.43 μM。 PCI-24781 治疗会导致 HCT116 或 DLD-1 细胞中乙酰化组蛋白和乙酰化微管蛋白呈剂量依赖性积累,诱导 p21 表达,并导致 PARP 裂解和 γH2AX 积累。 PCI-24781 对 HDAC 酶的抑制会导致与 HR 特别相关的基因(包括 RAD51)的转录显着减少。与 HR 的抑制一致,PCI-24781 处理会导致转染的 CHO 细胞中 I-SceI 诱导的染色体断裂的同源定向修复能力下降。 PCI-24781 诱导软组织肉瘤 (STS) 细胞 S 期耗竭、G2 细胞周期停滞和细胞凋亡。 PCI-24781 在 STS 细胞中诱导 Rad51 转录抑制,这可能是通过增强 E2F1 与 Rad51 近端启动子的结合介导的。 PCI-24781 在霍奇金淋巴瘤和非霍奇金淋巴瘤细胞系中通过 NF-κB 机制诱导 caspase 和活性氧依赖性细胞凋亡。激酶测定:使用连续胰蛋白酶偶联测定来测量 HDAC 活性。对于抑制剂表征,使用 96 孔测定板在 100 μL 反应体积中进行测量。对于每种同工酶,反应缓冲液中的 HDAC 蛋白 [50 mM HEPES、100 mM KCl、0.001% Tween 20、5% DMSO (pH 7.4),补充浓度为 0% (HDAC1)、0.01% (HDAC2) 的牛血清白蛋白、3、8 和 10) 或 0.05% (HDAC6)] 与不同浓度的 PCI-24781 混合,并孵育 15 分钟。添加胰蛋白酶至终浓度为 50 nM,添加乙酰基-Gly-Ala-(N-乙酰基-Lys)-AMC 至终浓度为 25 μM(HDAC1、3 和 6)、50 μM(HDAC2 和10) 或 100 μM (HDAC8) 来启动反应。阴性对照反应在不存在 PCI-24781 的情况下进行,重复八次。在荧光板读数器中监测反应。 30 分钟的滞后时间后,使用 355 nm 的激发波长和 460 nm 的检测波长在 30 分钟的时间范围内测量荧光。荧光随时间的增加被用作反应速率的量度。抑制常数 Ki(app) 使用程序 BatchKi 获得。细胞测定:将细胞培养至少两次倍增,并在 PCI-24781 暴露结束时使用阿拉玛蓝荧光细胞增殖测定监测生长。 PCI-24781 在 96 孔板的一式三份孔中以 9 个浓度进行测定,使用范围为 0.0015 μM 至 10 μM 的半对数间隔。每孔中的最终 DMSO 浓度为 0.15%。使用四参数逻辑方程通过非线性回归估计抑制细胞生长 50% (GI50) 和 95% 置信区间所需的浓度。
|
| 体内研究 (In Vivo) |
PCI-24781 以 200 mg/kg 的剂量每天一次(qod)给药,可显着抑制小鼠体内 HCT116 和 DLD-1 异种移植物的生长,分别达 69% 和 59%。在 HCT116 中以 20 mg/kg、40 mg/kg、80 mg/kg 或 160 mg/kg 的剂量每天一次给予 PCI-24781,连续 4 天,然后每周 3 天不治疗(每周 4 次)模型分别抑制肿瘤生长 48%、57%、82.2% 或 80.0%。
Abexinostat (PCI24781; CRA024781)的抗肿瘤活性和乙酰化诱导作用 [1] 为了评估CRA-024781的体内抗肿瘤活性,使用不同剂量和时间表对携带人结肠肿瘤异种移植物的小鼠静脉注射该化合物。在之前的HCT116异种移植物剂量计划研究中,静脉注射CRA-024781确定了两种具有良好治疗指标的方案:(a)每隔一天一次(q.o.d)或(b)连续4天每天一次,然后每周3天不治疗(q.d×每周4次;剂量计划数据未显示)。当根据第一种方案在HCT116或DLD-1异种移植物中以200mg/kg i.v.qo.d.的剂量评估CRA-024781时,观察到对肿瘤生长的统计学显著抑制(图4A和B)。HCT116和DLD-1模型的肿瘤生长抑制率分别为69%(P<0.000001)和59%(P<0.01)。尽管在DLD-1研究中观察到相对于溶媒对照组体重减轻了13%,但在HCT116研究中没有观察到体重减轻,这表明实验之间存在一些耐受性差异,200mg/kg接近每日一次给药的最大耐受剂量(数据未显示)。然后使用第二种方案(q.d×每周4次)对CRA-024781进行多剂量评估。在HCT116模型中,20、40、80和160 mg/kg的肿瘤生长抑制率分别为48%(P<0.05)、57%(P<0.01)、82.2%(P<0.0001)和80.0%(P<0.00001)。到研究结束时,这些剂量均未导致动物相对于载体的体重减轻(数据未显示)。在DLD-1模型中,CRA-024781每周4次,每天一次,没有显著抑制肿瘤生长,尽管在最高剂量160 mg/kg时观察到轻微的抑制趋势,显示出43%的抑制率(P=0.09),没有相关的体重减轻(数据未显示)。为了确定研究中获得的CRA-024781的血浆浓度是否足以在体内抑制HDAC酶,对外周血细胞进行了离体检查。如图5所示,给药后2小时和6小时,每个治疗组的微管蛋白乙酰化都有可测量的增加。总之,CRA-024781对HCT116和DLD-1人结直肠肿瘤异种移植物均表现出统计学上显著的抗肿瘤活性,尽管总体而言,在HCT116异种移植物模型中抗肿瘤活性似乎更为明显。 将Abexinostat(PCI24781;CRA024781)与化疗联合使用可在体内产生优异的抗STS作用。接下来,我们评估了PCI-24781单独和联合化疗在体内的影响。在四项武装研究中使用了肌肉内生长的SKLMS1和皮下生长的HT1080或作为实验性肺转移瘤,比较了低剂量阿霉素、顺铂、PCI-24781或PCI-24781联合化疗对SCID小鼠中人类STS局部和转移生长的影响。肿瘤形成后开始治疗(100mm3)。同样,在实验性肺转移模型中,只有在通过生物发光鉴定出已建立的转移后才开始治疗[3] 线性混合模型用于评估治疗组随时间的肿瘤生长(以对数转换的肿瘤体积表示),线性回归模型用于评估各治疗组的肿瘤重量。单独使用低剂量阿霉素治疗对SKLMS1异种移植物的生长没有显著影响(图3A)Abexinostat(PCI24781;CRA024781)单独诱导显著的肿瘤生长抑制(PCI-24781治疗的小鼠与对照组未治疗的肿瘤的肿瘤体积与时间的斜率;P=0.001)。最重要的是,与对照组、单独使用阿霉素或单独使用PCI-24781治疗肿瘤组相比,联合PCI-24781和低剂量阿霉素具有显著的抑制作用(P<0.0001)。研究结束时,对照组的平均肿瘤重量为1.62 g±0.47,阿霉素为1.34 g±0.43,PCI-24781为1.11 g±0.26,联合用药为0.64 g±0.24(图3B)。与对照组相比,单独使用PCI-24781显著降低了肿瘤重量(P=0.026)。此外,与其他治疗相比,PCI-24781联合化疗显著减轻了肿瘤重量(对照组、阿霉素和PCI-24781分别为P<0.0001、=0.0023和=0.047)。[3] 不同治疗组肿瘤的H&E染色显示,在阿贝诺司他(PCI24781;CRA024781)和联合治疗组中,肿瘤明显坏死(图3C);对活肿瘤切片进行免疫组织化学评估,以了解不同疗法对STS细胞增殖(PCNA)和凋亡(TUNEL)的影响。PCNA和TUNEL阳性染色核的平均值显示,对照组为88±2和20±2.4,阿霉素为85±1.2和16±1.4,PCI-24781为71±2.3和19±1.1,联合治疗为57±4.6和61±18.4,表明联合治疗具有最强的抗增殖和凋亡诱导作用(P<0.05)。还对切片进行了CD31染色,以检查对肿瘤相关血管系统的不同治疗效果。CD31计数没有显著差异;然而,在联合治疗组中,可以观察到大而通畅的血管数量显著减少[3]。 同样,在HT1080异种移植物中测试了Abexinostat (PCI24781; CRA024781)、顺铂及其组合的效果(图4)。与顺铂或PCI-24781治疗组和对照组小鼠相比,没有发现随时间推移的显著肿瘤生长差异。然而,联合治疗观察到肿瘤生长明显减少(与其他治疗组相比,P<0.001;图4A)。研究结束时,对照组的平均肿瘤重量为1.23 g±0.15,顺铂组为1.01 g±0.39,PCI-24781组为1.09 g±0.54,联合用药组为0.36 g±0.22(图4B)。单独使用PCI-24781或顺铂治疗没有明显减轻肿瘤重量,而联合治疗则观察到明显的肿瘤重量减轻(分别与对照组、顺铂组和PCI-24781组相比,P=0.0003、=0.0038和=0.0011)。免疫组织化学结果与上述SKLMS1治疗的肿瘤相似,显示PCI-24781和联合组坏死增加(图4C)。联合治疗组增殖减少和凋亡增强最为明显(对照组的平均PCNA和TUNEL阳性染色核分别为83±7.1和18±0.3,顺铂组为62±2.8和17±2.5,PCI-24781组为50±2.8和21±5.9,联合治疗组为38±14.1和33±8.6;P<0.05)。各组间CD31阳性率没有显著差异,而联合组大血管减少[3]。 最后,评估了各种疗法对STS肺转移的影响。采用实验性纤维肉瘤肺转移模型Abexinostat(PCI24781;CRA024781)与阿霉素或顺铂联合使用进行了测试(图4D)。随后对小鼠进行生物发光;代表性的连续图像如图4D所示,显示联合治疗小鼠的生物发光减少。H&E染色显示,在对照和化疗治疗的肿瘤中,大的转移性沉积物取代了许多肺实质;在PCI-24781组中观察到较小的病变,在联合治疗小鼠中观察到微小的显微镜病变。肺转移重量是通过从研究结束时的实际肺重量中减去估计的平均正常小鼠肺重量来计算的。对照组的平均肺转移重量为0.55 g±0.14,顺铂为0.62 g±0.26,阿霉素为0.48 g±0.33,PCI-24781组为0.33 g±0.20,PCI-24781-顺铂为0.15 g±0.19,PCI-2488-阿霉素为0.13 g±0.14。在PCI-24781治疗的小鼠中观察到转移负荷减少的趋势,但没有达到统计学意义,而与对照组或顺铂治疗组相比,PCI-24781联合任何一种化疗都能显著减轻肺转移的重量(P<0.05)。综上所述,这些数据表明,尽管PCI-24781在体外表现出显著的抗STS作用,但在体内作为单一疗法仅具有微弱的疗效。然而,将PCI-24781与低剂量常规化疗联合使用可在体内显著抑制STS肿瘤和转移生长,这是对潜在临床应用的观察[3]。 |
| 酶活实验 |
连续运行的胰蛋白酶偶联测定用于测量 HDAC 活性。使用 96 孔测定板在 100 μL 反应体积中进行测量,以进行抑制剂表征。 HDAC 蛋白与每种同工酶不同浓度的 PCI-24781 结合,并孵育 15 分钟。反应缓冲液为 50 mM HEPES、100 mM KCl、0.001% Tween 20、5% DMSO (pH 7.4),补充浓度为 0% (HDAC1)、0.01% (HDAC2、3、8 和 10) 的牛血清白蛋白),或 0.05% (HDAC6)。通过添加终浓度为 25 μM(HDAC1、3 和 6)、50 μM(HDAC2 和 10)或 100 μM(HDAC8)的乙酰基-Gly-Ala-(N-乙酰基-Lys)-AMC 开始反应。 )。添加胰蛋白酶至终浓度为 50 nM。一式八份,阴性对照反应在没有 PCI-24781 的情况下进行。荧光板读取器用于跟踪反应。在 30 分钟的滞后时间后,使用 355 nm 的激发波长和 460 nm 的检测波长在 30 分钟内测量荧光。使用荧光随时间的增加来计算反应速率。程序BatchKi用于获得抑制常数Ki(app)。
HDAC活动[1] 使用之前详细描述的连续胰蛋白酶偶联测定法测量HDAC活性(11)。为了表征抑制剂,使用96孔测定板在100μL的反应体积内进行了测量。对于每种同工酶,将反应缓冲液中的HDAC蛋白[50 mmol/L HEPES、100 mmol/L KCl、0.001%吐温20、5%DMSO(pH 7.4),补充有浓度为0%(HDAC1)、0.01%(HDAC2、3、8和10)或0.05%(HDAC6)的牛血清白蛋白]与不同浓度的抑制剂混合,并孵育15分钟。加入胰蛋白酶至终浓度为50 nmol/L,加入乙酰基Gly-Ala-(N-乙酰基-Lys)-AMC至终浓度25μmol/L(HDAC1、3和6)、50μmol/L(HADC2和10)或100μmol/L(HDAC8)以引发反应。阴性对照反应在没有抑制剂的情况下进行,重复8次。在荧光板读数器中监测反应。在30分钟的延迟时间后,使用355nm的激发波长和460nm的检测波长在30分钟内测量荧光。荧光随时间的增加被用作反应速率的度量。使用BatchKi程序获得抑制常数Ki(app)。 |
| 细胞实验 |
对 10 种肿瘤细胞系和 HUVEC 进行至少两次倍增培养后,使用阿拉玛蓝荧光细胞增殖测定法评估生长,以确定化合物暴露的终点。使用 0.0015 至 10 μmol/L 范围内的半对数间隔,在 96 孔板的一式三份孔中以九种浓度对该化合物进行测定。每孔的 DMSO 最终浓度为 0.15%。使用四参数逻辑方程通过非线性回归估计抑制细胞生长 50% 和 95% 置信区间所需的浓度[1]。
细胞增殖试验[1] 将10个肿瘤细胞系和HUVEC培养至少两倍,并在化合物暴露结束时使用如前所述的Alamar蓝荧光细胞增殖测定法监测生长。使用0.0015至10μmol/L的半对数间隔,在96孔板的三个孔中以9种浓度对化合物进行了测定。每个孔中的DMSO最终浓度为0.15%。使用四参数逻辑斯谛方程通过非线性回归估计抑制细胞生长50%(GI50%)和95%置信区间所需的浓度。 组蛋白和微管蛋白乙酰化、p21Cip1/WAF1积累、聚ADP核糖聚合酶切割和磷酸化组蛋白变体H2AX[2] 通过蛋白质印迹法检测了用Abexinostat (PCI24781; CRA024781)处理的细胞中乙酰化组蛋白、乙酰化微管蛋白、p21Cip1/WAF1、聚ADP核糖聚合酶(PARP)切割和磷酸化组蛋白变体H2AX(γH2AX)蛋白。肿瘤细胞和亚融合的HUVEC在浓度范围为0.01至10μmol/L的Abexinostat (PCI24781; CRA024781)存在下培养18小时。然后收集细胞并在含有蛋白酶抑制剂和磷酸酶抑制剂的裂解缓冲液中裂解。将裂解物溶解在SDS-PAGE还原样品缓冲液中,煮沸,然后在Novex Tris-甘氨酸凝胶中电泳。将凝胶印迹到硝化纤维上,用抗乙酰赖氨酸抗体检测乙酰化组蛋白、抗乙酰化微管蛋白抗体、抗p21Cip1/WAF1抗体、抗PARP抗体或抗γH2AX抗体。洗涤印迹,用适当的辣根过氧化物酶偶联的二抗孵育,并对印迹进行增强化学发光处理。 Annexin V染色法检测细胞凋亡。[2] 为了确定Abexinostat(PCI24781;CRA024781)和PARP抑制剂PJ34(EMD Biosciences)在HCT116细胞中的潜在协同作用,通过分析单独或联合使用特定剂量的药物96小时后膜联蛋白V-FITC(Biosource)的结合来评估细胞毒性。调整剂量,以保持两种药物在两种联合治疗中的比例恒定。使用FACSCalibur仪器(Becton Dickinson)定量细胞凋亡。CalcuSyn程序(Biosoft)用于根据参考文献29中所述计算的CI生成中值效应图。CI大于1表示拮抗作用,CI为1表示相加作用,CI小于1表示协同作用。为了确定HCT116细胞在24小时时的凋亡百分比,用0.2、0.5和1.0μM PCI-24781处理细胞,24小时后评估膜联蛋白V结合。 免疫荧光。[2] HCT116细胞在室载玻片上生长,用0.2μM的Abexinostat (PCI24781; CRA024781)处理24小时。然后将细胞暴露于10 Gy的辐射下,并在辐射后孵育1或16小时。然后将细胞固定在含有2%多聚甲醛、0.2%Triton X-100的PBS缓冲液中并透化。将细胞封闭在2%BSA的PBS中,用抗RAD51多克隆抗体探测,然后用AlexaFluor594偶联的二抗探测。染色后,使用带有DAPI的Vecta屏蔽安装介质 安装盖玻片,并使用荧光显微镜进行可视化。 TaqMan基因表达检测。[2] HCT116细胞用Abexinostat(PCI24781;CRA024781)处理不同时间,并使用RNeasy试剂盒 提取总RNA。使用核糖绿RNA定量试剂盒(分子探针)定量总RNA。根据制造商的说明,通过使用TaqMan主混合物 和50ng总RNA作为模板,建立一式三份的一步RT-PCR测定。重新测定每个反应孔中的RNA量,并用于正常化。 蛋白质印迹分析。[2] 用Abexinostat(PCI24781;CRA024781)处理细胞指定时间并裂解,使用BCA蛋白检测试剂盒 定量总蛋白。每条泳道中都装载了等量的蛋白质。用于阻断胱天蛋白酶切割的泛胱天蛋白酶抑制剂Q-VD-OPh购自MP Biomedicals。每种处理的总蛋白(30μg)在4-15%梯度SDS-PAGE凝胶 上溶解。将蛋白质转移到PVDF膜上,并使用与AlexaFluor680和IFdye800 偶联的适当一抗和二抗进行检测。使用Odyssey扫描仪 进行成像。 同源重组修复试验。[2] 如参考文献39所述,在DRAA8中国仓鼠卵巢细胞中测量同源重组修复活性。简而言之,DRAA8/CHO细胞包含一个无功能的GFP序列和一个整合到hprt基因座的内部GFP(iGFP)序列。突变的GFP序列包含一个18 bp的I-SceI识别位点,通过表达I-SceI-内切酶引入DSBs。通过使用核转染(Amaxa)转染I-SceI表达载体(3.5μg),并使用FACS通过测量GFP信号来定量使用下游iGFP重复序列诱导的DSB基因转化Abexinostat(PCI24781;CRA024781)转染后6小时以适当浓度加入,根据7-氨基放线菌素D(7-AAD)信号对活细胞进行门控,36小时后分析门控活细胞群中的GFP表达。 克隆生存试验。[2] 为了确定Abexinostat(PCI24781;CRA024781)处理对CHO-K1和NHEJ缺陷型Ku80突变XRS5细胞系集落形成的影响,将适当板密度的细胞铺在10cm的培养皿中并允许其附着。将细胞暴露于0.5、1.0或2.0μM浓度的药物中24小时,然后将细胞置于不含药物的新鲜生长培养基中,孵育7-10天。菌落用100%异丙醇固定,用1%结晶紫染色。对于每种情况,进行三次测定。在HCT116、NCI-H460和A549肺肿瘤细胞系中,为了确定PCI-24781治疗与辐射协同作用的适当时间,用1μM PCI-247811预处理培养物不同长度的时间,范围从2到24小时。将细胞暴露于0、2、4或6 Gy辐射(Gammacell 40,Atomic Energy of Canada,有限公司),并在7-12天后评估克隆生存率。根据每个剂量的镀覆效率,计算集落形成能力的百分比。 细胞增殖的测量。[3] 根据制造商的说明,细胞生长测定使用CellTiter96水性非放射性细胞增殖测定试剂盒。在HDACi(Abexinostat(PCI24781;CRA024781)/SAHA)治疗和阿霉素或顺铂单独或与HDACi联合治疗后48小时分析生长率;评估了几种给药顺序:用PCI-24781预处理24小时,然后加化疗24小时,反之,用化疗预处理,然后加PCI-24781,以及同时用这两种化合物治疗24小时。在490 nm波长下测量吸光度;处理过的细胞吸光度值以未处理细胞吸光度的百分比表示。 克隆试验。[3] STS细胞在培养皿中用DMSO(对照)和不同浓度的HDACi(Abexinostat(PCI24781;CRA024781)/SAHA)处理24小时。每孔重新接种100个细胞,然后在正常培养基中生长10天,然后用6%戊二醛、0.5%结晶紫溶液染色30分钟。从每个孔中倒出染色溶液,用去离子水洗涤细胞。计数保留染色溶液的单个菌落。 细胞周期分析。[3] STS细胞单层用Abexinostat(PCI24781;CRA024781)/SAHA处理不同时间。如所述进行碘化丙啶/荧光激活细胞分选(FACS)分析。 |
| 动物实验 |
Female BALB/c nu/nu mice are given 3×106 tumor cells each, along with DLD-1 and HCT116 tumor cells, subcutaneously. When the tumor volume was on average -100 mm, treatment with Abexinostat (CRA 024781) began[1]. To measure the antitumor activity of Abexinostat (CRA 024781), mice with human colon tumor xenografts are given different doses and schedules of the drug intravenously [1].
Pharmacokinetic Analysis [1] Abexinostat (PCI24781; CRA024781) was formulated in 30% HP-cyclodextrin in water and a 10 mg/kg bolus dose was administered i.v. to female BALB/c nu/nu mice (16–22 g). Blood samples were collected over 24 hours. Plasma was prepared from each blood sample with lithium heparin and was assayed for Abexinostat (PCI24781; CRA024781) by liquid chromatography with tandem mass spectrometry. Mouse plasma samples were assayed for CRA-024781 by high-performance liquid chromatography with tandem mass spectrometric detection. Plasma samples were extracted by protein precipitation using acetonitrile (MeCN). A Hypersil C-18 column, 50 × 2.1 mm was used for sample separation. Samples were separated on reversed-phase high-performance liquid chromatography under linear gradient conditions using water/MeCN as mobile phases, at a flow rate at 0.5 mL/min. Samples were ionized under electrospray and quantified by multiple reactive monitoring, recording the transition from the molecular ion to the product ion: 398 → 200 m/z. Linearity (>0.25–1,000 ng/mL) was achieved with interday and intraday coefficient of variation (%) and deviation of the mean from theoretical (%) ±15%. The lower limit of quantitation was 0.25 ng/mL. Pharmacokinetic variables were estimated with compartmental methods using WinNonlin-Pro version 4.1 (Pharsight Corp., Mountain View, CA). Pharmacokinetic calculations were done using nominal doses and nominal collection times. In vivo Efficacy Studies [1] Female BALB/c nu/nu mice were acclimated for 3 to 5 days prior to tumor implantation. All mice were maintained in sterilized translucent polycarbonate microisolator cages under specific pathogen–free conditions. HCT116 and DLD-1 tumor cells were implanted s.c. in nude mice at 3 × 106 per mouse. Tumor-bearing mice were randomized based on tumor volume prior to the initiation of treatment. Treatment with Abexinostat (PCI24781; CRA024781) started when the average tumor volume was ∼100 mm3. Tumor volume was calculated as follows: volume = 0.5 × X2 × Y, where X, tumor width; and Y, tumor length. The vehicle used in all studies was 20% HP-β-cyclodextrin in water. Dosages were given i.v. either every other day (q.o.d.) or for 4 consecutive days followed by 3 days without treatment for each week of the study (q.d. × 4 per week) as indicated. Inhibition of tumor growth was calculated as follows: 100 × (1 − dT/dC), where dT was the change in average tumor volume since the first dose in the treatment group and dC was the change in average tumor volume since the first dose in the control group. Statistical analysis was done with one-way ANOVA on log-transformed data to meet the assumption of underlying normal distribution for the test to be valid, and P values were corrected for multiple comparisons to control by Dunnett's method. For single-group comparison, statistical analyses were done with t test on log-transformed data to meet the assumption of an underlying normal distribution for the test to be valid. In Vivo Studies. [2] BALB/c female nude mice were implanted s.c. with 3 × 106 HCT116 cells in a 1:1 ratio with Matrigel into the right-hand flank 24 h after administering 4.5 Gy (whole-body irradiation). Mice were entered into study ≈10 days after implantation or when tumor volumes reached a minimum of 75–100 mm3. Four treatment regimens were followed with three animals in each group, each receiving a dose of 200 mg/kg: (i) vehicle; (ii) animals received a single oral dose 4 h before the end of the study (1×); (iii) animals received one oral dose 28 h before the end of the study and a second dose 6 h later (2×); and (iv) animals were dosed as in the 2× group but also received a third dose the following morning, 24 h after the first dose was administered and 4 h before the end of the study (3×). Animals were humanely killed, tumors were extracted, and total protein was isolated and quantitated by using the BCA protein assay kit. Total protein (30 μg) was loaded for each tumor, and Western blotting was performed to determine RAD51, acetylated tubulin, and actin levels. In vivo therapeutic studies. [3] Trypan blue staining confirmed viable STS cells (SKLMS1 or HT1080 cells 1 × 106/0.1 mL HBSS/mouse) were injected into the flank (SKLMS1 i.m., HT1080 s.c.) of 6-wk-old female SCID mice (n = 40/experiment), growth was measured twice weekly; HT1080GL cells (stably expressing green fluorescent protein/Luciferase) were tail vein injected, resulting in experimental lung metastases that could be followed by bioluminescence. When average tumor volumes reached 100 mm3, the mice were assigned to four treatment groups (7-8 mice/group): (a) control (vehicles only); (b) doxorubicin/cisplatinum (1.2 mg/kg/biweekly and 2 mg/kg/biweekly, respectively, i.p.); (c) Abexinostat (PCI24781; CRA024781) (50 mg/kg/d ×5 d/wk, i.p.); and (d) Abexinostat (PCI24781; CRA024781) plus chemotherapy (PCI-24781 initiated 24 h before chemotherapy in all cases). PCI-24781 dose and treatment schedules were determined per company recommendations. A similar experimental design was used for lung metastasis treatment, initiated when bioluminescence showed established lung metastases; the study included six arms so that Abexinostat (PCI24781; CRA024781) combined with either chemotherapeutic agent could be evaluated. The mice were followed for tumor size and body weight and sacrificed when control group tumors reached 1.5 cm average largest dimension or when bioluminescence suggested control group had significant pulmonary tumor load. Tumors were resected, weighed, and frozen or fixed in formalin and paraffin-embedded for immunohistochemical studies. Similarly, lungs were resected, weighed, and fixed in formalin. |
| 药代性质 (ADME/PK) |
In vivo Pharmacokinetics [1]
Having established that Abexinostat (PCI24781; CRA024781) displayed HDAC inhibitory and antitumor properties in vitro, we assessed the pharmacokinetics of the compound to evaluate exposure in order to enable further testing in efficacy models. CRA-024781 was delivered i.v. to female mice and plasma concentrations were monitored over time (Fig. 3). Based on these data, the clearance was calculated to be 297 mL/min/kg, the volume of distribution in the central compartment was 3,750 mL/kg, the steady-state volume of distribution was 9,230 mL/kg, the predominant plasma half-life was 6.7 minutes (73% area under the curve), and the mean residence time was 31 minutes. These data suggest that CRA-024781 had sufficient in vivo exposure when given by the i.v. route of administration for use in the study of the biological effects of HDAC inhibition in vivo. CRA-024781 had an in vivo pharmacokinetic profile that suggested adequate drug exposure to allow HDAC inhibition in vivo. The 10 mg/kg i.v. dose achieved a plasma concentration above the measured cellular GI50% for HCT116 tumor cells for 15 minutes. However, it is difficult to predict a priori the in vivo drug exposure (area under the curve) that will be adequate for efficacy based on GI50% or on the appearance of mechanistic biomarkers (protein acetylation, etc.), because these values are based on continuous exposure of tumor cells to the drug in vitro, on the other hand, tumors grown in vivo are exposed to the drug on a certain schedule (e.g., q.d. × 4 for 16 days) at varying concentrations of compound based on the pharmacokinetics and degree of protein binding of the drug in plasma. Also, the drug concentration in plasma does not necessarily reflect the concentration distributed to the tumor. Indeed, the relatively high steady-state volume of distribution (9,230 mL/kg) suggests that CRA-024781 may readily distribute into tissues. Nevertheless, the doses required for maximal efficacy (≥80 mg/kg) are >10 mg/kg, perhaps because HDAC enzymes must be inhibited for a more prolonged period of time or to a greater extent following each dose in order to achieve antitumor efficacy. |
| 毒性/毒理 (Toxicokinetics/TK) |
In a previous experiment, an oral dose of 200 mg/kg did not cause toxicity as measured by body weight loss when dosed for 3 consecutive days. The dose of 200 mg/kg in mice was also chosen because it is similar to the plasma area under the concentration–time curve expected in an ongoing clinical trial after an oral dose of 2.0 mg/kg.[2]
|
| 参考文献 |
|
| 其他信息 |
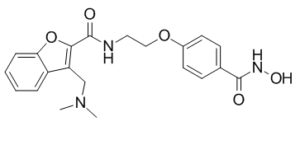
3-[(dimethylamino)methyl]-N-[2-[4-[(hydroxyamino)-oxomethyl]phenoxy]ethyl]-2-benzofurancarboxamide is a member of benzofurans.
Abexinostat has been used in trials studying the treatment of Sarcoma, Lymphoma, Leukemia, Lymphocytic, and Hodgkin Disease, among others. It is a novel, broad-spectrum hydroxamic acid-based inhibitor of histone deacetylase (HDAC) with potential antineoplastic activity. Abexinostat is an orally bioavailable hydroxamate-based pan-inhibitor of histone deacetylase (HDAC), with potential antineoplastic and radiosensitizing activities. Upon administration, abexinostat inhibits HDAC, resulting in an accumulation of highly acetylated histones, followed by the induction of chromatin remodeling; the selective transcription of tumor suppressor genes; and the tumor suppressor protein-mediated inhibition of tumor cell division and induction of tumor cell apoptosis. In addition, abexinostat decreases the expression of the DNA-repair protein RAD51, thereby reducing the RAD51 protein, preventing repair of DNA double-strand breaks and increasing sensitivity of tumor cells to DNA damaging agents. HDAC, upregulated in many tumor types, is an enzyme that is responsible for the deacetylation of chromatin histone proteins. Mechanism of Action Abexinostat is a novel histone deacetylase (HDAC) inhibitor. HDAC inhibitors target HDAC enzymes and inhibit the proliferation of cancer cells and induce cancer cell death, or apoptosis. Histone deacetylation is carried out by a family of related HDAC enzymes. Inhibition of these enzymes causes changes to chromatin structure and to gene expression patterns, which results in the inhibition of proliferation of cancer cells, and induction of apoptosis. CRA-024781 is a novel, broad spectrum hydroxamic acid-based inhibitor of histone deacetylase (HDAC) that shows antitumor activity in vitro and in vivo preclinically and is under evaluation in phase I clinical trials for cancer. CRA-024781 inhibited pure recombinant HDAC1 with a K(i) of 0.007 mumol/L, and also inhibited the other HDAC isozymes HDAC2, HDAC3/SMRT, HDAC6, HDAC8, and HDAC10 in the nanomolar range. Treatment of cultured tumor cell lines grown in vitro with CRA-024781 resulted in the accumulation of acetylated histone and acetylated tubulin, resulting in an inhibition of tumor cell growth and the induction of apoptosis. CRA-024781 parenterally administered to mice harboring HCT116 or DLD-1 colon tumor xenografts resulted in a statistically significant reduction in tumor growth at doses that were well tolerated as measured by body weight. Inhibition of tumor growth was accompanied by an increase in the acetylation of alpha-tubulin in peripheral blood mononuclear cells, and an alteration in the expression of many genes in the tumors, including several involved in apoptosis and cell growth. These results reveal CRA-024781 to be a novel HDAC inhibitor with potent antitumor activity.[1] Histone deacetylase (HDAC) inhibitors such as the phenyl hydroxamic acid PCI-24781 have emerged recently as a class of therapeutic agents for the treatment of cancer. Recent data showing synergy of HDAC inhibitors with ionizing radiation and other DNA-damaging agents have suggested that HDAC inhibitors may act, in part, by inhibiting DNA repair. Here we present evidence that HDAC enzymes are important for homologous recombinational repair of DNA double-strand breaks. Combination studies of PCI-24781 with the poly(ADP-ribose) polymerase inhibitor PJ34, an agent thought to produce lesions repaired by homologous recombination (HR), resulted in a synergistic effect on apoptosis. Immunofluorescence analysis demonstrated that HDAC inhibition caused a complete inhibition of subnuclear repair foci in response to ionizing radiation. Mechanistic investigations revealed that inhibition of HDAC enzymes by PCI-24781 led to a significant reduction in the transcription of genes specifically associated with HR, including RAD51. RAD51 protein levels were significantly decreased after 24 h of drug exposure both in vitro and in vivo. Consistent with inhibition of HR, treatment with PCI-24781 resulted in a decreased ability to perform homology directed repair of I-SceI-induced chromosome breaks in transfected CHO cells. In addition, an enhancement of cell killing was observed in Ku mutant cells lacking functional nonhomologous end joining compared with WT cells. Together these results demonstrate that HDAC enzymes are critically important to enable functional HR by controlling the expression of HR-related genes and promoting the proper assembly of HR-directed subnuclear foci. [2] Purpose: Histone deactylase inhibitors (HDACi) are a promising new class of anticancer therapeutics; however, little is known about HDACi activity in soft tissue sarcoma (STS), a heterogeneous cohort of mesenchymal origin malignancies. Consequently, we investigated the novel HDACi PCI-24781, alone/in combination with conventional chemotherapy, to determine its potential anti-STS-related effects and the underlying mechanisms involved. Experimental design: Immunoblotting was used to evaluate the effects of PCI-24781 on histone and nonhistone protein acetylation and expression of potential downstream targets. Cell culture-based assays were utilized to assess the effects of PCI-24781 on STS cell growth, cell cycle progression, apoptosis, and chemosensitivity. Quantitative reverse transcription-PCR, chromatin immunoprecipitation, and reporter assays helped elucidate molecular mechanisms resulting in PCI-24781-induced Rad51 repression. The effect of PCI-24781, alone or with chemotherapy, on tumor and metastatic growth was tested in vivo using human STS xenograft models. Results: PCI-24781 exhibited significant anti-STS proliferative activity in vitro, inducing S phase depletion, G(2)/M cell cycle arrest, and increasing apoptosis. Superior effects were seen when combined with chemotherapy. A PCI-24781-induced reduction in Rad51, a major mediator of DNA double-strand break homologous recombination repair, was shown and may be a mechanism underlying PCI-24781 chemosensitization. We showed that PCI-24781 transcriptionally represses Rad51 through an E2F binding-site on the Rad51 proximal promoter. Although single-agent PCI-24781 had modest effects on STS growth and metastasis, marked inhibition was observed when combined with chemotherapy. [3] |
| 分子式 |
C21H23N3O5
|
|
|---|---|---|
| 分子量 |
397.42
|
|
| 精确质量 |
397.163
|
|
| 元素分析 |
C, 63.46; H, 5.83; N, 10.57; O, 20.13
|
|
| CAS号 |
783355-60-2
|
|
| 相关CAS号 |
|
|
| PubChem CID |
11749858
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 密度 |
1.3±0.1 g/cm3
|
|
| 折射率 |
1.624
|
|
| LogP |
1.68
|
|
| tPSA |
107.53
|
|
| 氢键供体(HBD)数目 |
3
|
|
| 氢键受体(HBA)数目 |
6
|
|
| 可旋转键数目(RBC) |
8
|
|
| 重原子数目 |
29
|
|
| 分子复杂度/Complexity |
550
|
|
| 定义原子立体中心数目 |
0
|
|
| SMILES |
O=C(NCCOC1=CC=C(C=C1)C(NO)=O)C2=C(C3=CC=CC=C3O2)CN(C)C
|
|
| InChi Key |
MAUCONCHVWBMHK-UHFFFAOYSA-N
|
|
| InChi Code |
InChI=1S/C21H23N3O5/c1-24(2)13-17-16-5-3-4-6-18(16)29-19(17)21(26)22-11-12-28-15-9-7-14(8-10-15)20(25)23-27/h3-10,27H,11-13H2,1-2H3,(H,22,26)(H,23,25)
|
|
| 化学名 |
3-[(dimethylamino)methyl]-N-[2-[4-(hydroxycarbamoyl)phenoxy]ethyl]-1-benzofuran-2-carboxamide
|
|
| 别名 |
CRA024781; PCI24781; CRA 024781; ABEXINOSTAT; 783355-60-2; PCI-24781; PCI 24781; CRA-024781; CRA-02478; CRA 024781; Abexinostat [USAN]; PCI-24781; CRA024781; PCI 24781; CRA-024781
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 该产品在溶液状态不稳定,请现配现用。 |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 6 mg/mL (15.10 mM) in 20% HP-β-CD in Saline (这些助溶剂从左到右依次添加,逐一添加), 悬浮液;超声助溶。
*生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.5162 mL | 12.5811 mL | 25.1623 mL | |
| 5 mM | 0.5032 mL | 2.5162 mL | 5.0325 mL | |
| 10 mM | 0.2516 mL | 1.2581 mL | 2.5162 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT03939182 | Active Recruiting |
Drug: Abexinostat Drug: Ibrutinib |
Diffuse Large B-cell Lymphoma Mantle Cell Lymphoma |
Memorial Sloan Kettering Cancer Center |
May 29, 2019 | Phase 1 |
| NCT03600441 | Active Recruiting |
Drug: Abexinostat | Follicular Lymphoma | Xynomic Pharmaceuticals, Inc. | August 27, 2018 | Phase 2 |
| NCT03590054 | Active Recruiting |
Drug: Abexinostat Biological: Pembrolizumab |
Locally Advanced Melanoma Metastatic Melanoma |
Rahul Aggarwal | August 20, 2018 | Phase 1 |
| NCT03934567 | Recruiting | Drug: Abexinostat | Lymphoma, Follicular | Xynomic Pharmaceuticals, Inc. | April 22, 2020 | Phase 2 |
| NCT03936153 | Recruiting | Drug: abexinostat | Diffuse Large B-cell Lymphoma (DLBCL) |
Xynomic Pharmaceuticals, Inc. | January 20, 2020 | Phase 2 |