| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 500mg |
|
||
| 2g |
|
||
| 5g |
|
||
| 10g |
|
||
| 25g | |||
| Other Sizes |
| 靶点 |
M2 channel
|
|---|---|
| 体外研究 (In Vitro) |
研究人员报告了离子通道抑制剂金刚烷胺、美金刚和金刚乙胺(Rimantadine)对严重急性呼吸综合征冠状病毒2(SARS-CoV-2)的体外效力。在VeroE6细胞中,金刚乙胺效力最强,其次是美金刚和金刚烷胺(50%有效浓度分别为36、80和116 µM)。金刚乙胺还显示出最高的选择性指数,其次是金刚烷胺和美金刚(分别为17.3、12.2和7.6)。在人肝癌Huh7.5和肺癌A549-hACE2细胞中观察到类似结果。这些抑制剂与瑞德西韦的相互作用方式相似且均为拮抗作用,对病毒逃逸的屏障也相似。金刚乙胺主要在病毒进入后阶段发挥作用,部分在病毒进入阶段发挥作用。基于这些结果,金刚乙胺显示出治疗SARS-CoV-2的最大潜力。[3]
金刚烷胺、美金刚和金刚乙胺在体外对SARS-CoV-2显示活性[3] 为确定金刚烷衍生物对SARS-CoV-2的效力,我们基于SARS-CoV-2刺突蛋白免疫染色定量感染细胞,进行了96孔板短期浓度-反应实验。实验在非洲绿猴VeroE6细胞(评估抗SARS-CoV-2药物活性的原型细胞系)、人肝癌Huh7.5和人肺癌A549-hACE2细胞中进行。所用抑制剂浓度未导致细胞活力降低(相对细胞活力>90%),如图S2-S4所示。所有细胞类型中均获得类似结果,EC50值在微摩尔范围内。金刚乙胺效力最强,在VeroE6、Huh7.5和A549-hACE2细胞中的EC50分别为36、26和70 µM。美金刚显示中等效力(EC50为80、86和70 µM),金刚烷胺效力最低(EC50为116、118和80 µM)(图1,表1)。在最高使用浓度下,所有抑制剂在VeroE6和A549-hACE2细胞中均能完全抑制SARS-CoV-2,而在Huh7.5细胞中抑制效果略低(图1)。金刚烷胺的细胞毒性低于美金刚和金刚乙胺(表1,图S2-S4)。然而,由于其相对较高的效力,金刚乙胺在所有三种细胞系中具有最高的选择性指数(SI),而美金刚的SI最低(表1)。 金刚烷胺、美金刚和金刚乙胺与瑞德西韦的相互作用方式相似且均为拮抗作用[3] 为研究离子通道抑制剂与瑞德西韦的相互作用,进行了96孔板联合处理实验。SARS-CoV-2感染的VeroE6细胞分别用离子通道抑制剂单药、与瑞德西韦联用或单用瑞德西韦处理。抑制剂浓度根据先前确定的EC50值选择:离子通道抑制剂的EC50见表1,瑞德西韦的EC50为2.5 µM,如先前报道。对于所有三种离子通道抑制剂,联合处理的效果未超过单药处理的效果(图2,补充结果,表S1)。使用CompuSyn软件中Chou和Talalay方法进行的分析(补充方法中描述)显示,离子通道抑制剂与瑞德西韦之间主要为拮抗相互作用(补充结果,图S5、S6和表S2)。 金刚烷衍生物对病毒逃逸的屏障无显著差异[3] 为比较离子通道抑制剂在治疗条件下防止SARS-CoV-2传播的能力,我们根据抑制剂细胞毒性(图S2),使用金刚烷胺、美金刚和金刚乙胺在最高可能等效浓度(3倍EC50)下对感染的VeroE6细胞进行了长期处理。所有抑制剂处理均导致感染后第1天早期病毒传播动力学的类似延迟,而到第3-5天≥80%的培养细胞被感染,与未处理的对照培养物相当(图3)。然而,与未处理和美金刚处理的培养物相比,金刚烷胺和金刚乙胺处理的培养物中观察到细胞病变效应略有减轻。因此,总体而言,三种抑制剂在病毒逃逸屏障方面未显示重大差异。金刚乙胺的有利SI使其能够以7倍EC50进行处理,导致第3-5天额外的病毒抑制,而到第7天≥80%的培养细胞被感染。为研究是否获得替代可能促进病毒逃逸,对图3所示所有培养物在感染高峰期获得的病毒进行了NGS分析。在美金刚和金刚乙胺处理的培养物中,检测到未在未处理培养物中发现的替代,但无明显替代热点(表S3)。因此,抑制剂只能暂时抑制SARS-CoV-2。 |
| 体内研究 (In Vivo) |
金刚烷胺和金刚乙胺是口服抗病毒药物,可用于预防和治疗甲型流感病毒感染。本文综述了这些药物的药理学、抗病毒活性和作用机制、药代动力学、毒性、疗效和临床应用。当以等效剂量(每天200mg)给药时,金刚乙胺的预防效果与金刚烷胺相当,但产生不良反应的可能性较低。尽管结构相似,但这些药物的药代动力学存在显著差异,这些差异可能解释了金刚乙胺更有利的毒性特征。如果在无并发症的流感早期服用这两种药物,都能提供治疗益处,目前正在进行研究,以确定口服金刚乙胺在预防或治疗甲型流感病毒感染的严重并发症方面的有效性。[1]
以前没有研究过使用利曼他定治疗儿童流感以及与治疗相关的临床分离株的潜在耐药性发展。我们在一项针对91名流感样疾病儿童的对照双盲研究中比较了金刚乙胺和对乙酰氨基酚治疗。在69名确诊感染甲型H3N2流感的儿童中,37名接受了金刚乙胺治疗,32名接受了对乙酰氨基酚治疗,为期五天。在最初的三天里,接受金刚乙胺治疗的儿童发烧明显减少,症状和疾病严重程度的每日评分也有所改善。在头两天内,病毒脱落也显著减少,但随后增加,因此到第6天和第7天,金刚乙胺组中脱落病毒的儿童比例以及脱落的病毒数量显著增加。在为期七天的研究中,在金刚乙胺组的22名儿童中,有10名(45.5%)有耐药菌株,而对乙酰氨基酚组有2名(12.5%)有耐药性菌株(P小于.03)。因此,在金刚乙胺组的37名儿童中,27%的儿童被发现有耐药性,而接受对乙酰氨基酚治疗的总组为6%(P小于.04)。此外,在金刚乙胺组中,金刚乙胺的平均抑制浓度随时间增加(r=0.4,P=0.002),但在对乙酰氨基酚组中没有。因此,在改善儿童流感的临床体征和症状方面,利曼他定治疗似乎比对乙酰氨基酚更有效。金刚乙胺治疗还与停药后病毒脱落增加以及临床分离株耐药性的发展有关,其意义尚不清楚。[2] 在儿童中,利曼他定(RMT)在治疗的第三天有效地缓解了发烧。金刚烷胺(AMT)显示出对甲型流感感染的预防作用。AMT和RMT与不良反应发生率的增加无关。RMT也被认为对老年人具有良好的耐受性,但没有显示出预防作用。不同剂量在预防老年人流感以及报告不良反应方面具有可比性。在老年人中,扎那米韦比RMT更有效地预防甲型流感。 作者结论:AMT可有效预防儿童甲型流感。由于混杂因素可能影响了我们的研究结果,在考虑哪些患者应该服用这种预防药物时应该谨慎。我们关于这两种抗病毒药物治疗儿童甲型流感的有效性的结论仅限于RMT在治疗第三天退热方面的有效性。由于可用研究数量较少,我们无法就AMT的安全性或RMT在预防儿童和老年人流感方面的有效性得出明确结论[4]。 |
| 细胞实验 |
Rimantadine添加实验时间[3]
将96孔板中的VeroE6细胞接种MOI为0.01的严重急性呼吸系统综合征冠状病毒-2,感染期为2小时,并在接种后的不同时间点用230μM金刚乙胺处理。对于进入治疗,在接种后0小时将Rimantadine/金刚乙胺与病毒一起加入,并在2小时病毒感染阶段结束时将其清除。对于入组后治疗,接种后2、4或6小时加入金刚乙胺。在6个重复中测试了处理条件。治疗板包括12个感染的未治疗井和12个未感染的未处理井。孵育46-50小时后,对细胞进行严重急性呼吸系统综合征冠状病毒2型刺突蛋白免疫染色。数据点用SEM表示为抑制百分比。抑制百分比确定为100%–%的残余感染性(见前一节)。 96孔板短期治疗和添加时间实验的免疫染色和评估[3] 短期治疗板用1:5000稀释的第一抗体严重急性呼吸系统综合征冠状病毒2型刺突嵌合单克隆抗体、第二抗体F(ab')2-山羊抗人IgG Fc交叉吸附的第二抗体、HRP或山羊F(ab')2抗人IgG–Fc(HRP)、1:2000稀释的预吸附抗体和DAB底物BrightDAB试剂盒染色。使用ImmunoSpot系列5紫外线分析仪自动计数单个严重急性呼吸系统综合征冠状病毒2型刺突蛋白阳性细胞。感染治疗井的计数与感染非治疗井的平均计数相关,以计算单一抑制剂治疗的残余感染率百分比,此外,还计算联合治疗的抑制率百分比和添加时间实验。 |
| 动物实验 |
Background: Although amantadine (AMT) and rimantadine (RMT) are used to relieve or treat influenza A symptoms in healthy adults, little is known about the effectiveness and safety of these antivirals in preventing and treating influenza A in children and the elderly.
Objectives: The aim of this review was to systematically consider evidence on the effectiveness and safety of AMT and RMT in preventing and treating influenza A in children and the elderly.
Search strategy: We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library, 2007, issue 3); MEDLINE (1966 to July 2007) and EMBASE (1980 to July 2007).
Selection criteria: Randomised or quasi-randomised trials comparing AMT and/or RMT in children and the elderly with placebo, control, other antivirals or comparing different doses or schedules of AMT and/or RMT or no intervention.
Data collection and analysis: Two review authors independently selected trials for inclusion and assessed methodological quality. Disagreements were resolved by consensus. In all comparisons except for one, the trials in children and in the elderly were analysed separately. Data were analysed and reported using Cochrane Review Manager 4.2. software.[4]
|
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Well absorbed, with the tablet and syrup formulations being equally absorbed after oral administration. Following oral administration, rimantadine is extensively metabolized in the liver with less than 25% of the dose excreted in the urine as unchanged drug. Protein binding: Moderate (approximately 40%). Distribution: VolD - Adults: 17 to 25 L/kg. Children: MEan of 289 L. Concentrations in the nasal mucus average 50% higher than those in plasma. Well absorbed; tablets and syrup are absorbed equally well after oral administration. Time to peak concentration: 1 to 4 hours. For more Absorption, Distribution and Excretion (Complete) data for RIMANTADINE (11 total), please visit the HSDB record page. Metabolism / Metabolites Following oral administration, rimantadine is extensively metabolized in the liver with less than 25% of the dose excreted in the urine as unchanged drug. Glucuronidation and hydroxylation are the major metabolic pathways. Rimantadine hydrochloride is metabolized extensively in the liver to at least 3 hydroxylated metabolites. These have been designated as conjugated and unconjugated 3-, 4a-, and 4beta-hydroxylated metabolites. A glucuronide conjugate of rimantadine also has been identified. Extensively metabolized in the liver; glucuronidation and hydroxylation are the major metabolic pathways. Biological Half-Life 25 to 30 hours in young adults (22 to 44 years old). Approximately 32 hours in elderly (71 to 79 years old) and in patients with chronic liver disease. Approximately 13 to 38 hours in children (4 to 8 years old). Young adults (22 to 44 years old): 25 to 30 hours. Older adults (71 to 79 years old) and patients with chronic liver disease: Approximately 32 hours. Children (4 to 8 years old): 13 to 38 hours. |
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
Despite widespread use, there is little evidence that rimantadine when given orally causes liver injury, either in the form of serum enzyme elevations or clinically apparent liver disease. Likelihood score: E (unlikely cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation No information is available on rimantadine during breastfeeding. The manufacturer states that the drug should not be used during breastfeeding. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding Approximately 40% over typical plasma concentrations. Interactions Concurrent use of a single dose of rimantadine with cimetidine reduces rimantadine clearance by 18% in healthy adults; the clinical significance si thought to be minimal at this time. Because influenza antiviral agents reduce replication of influenza viruses, do not administer influenza virus vaccine live intranasal until at least 48 hours after rimantadine is discontinued and do not administer rimantadine until at least 2 weeks after administration of influenza virus vaccine live intranasal. Cimetidine Concurrent use of acetaminophen or aspirin with rimantadine reduces the peak serum concentration of rimantadine by approximately 11%; the clinical significance is thought to be minimal at this time. |
| 参考文献 |
|
| 其他信息 |
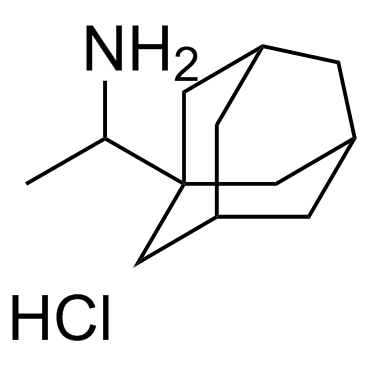
Rimantadine hydrochloride is an organic molecular entity.
Rimantadine Hydrochloride is the hydrochloride salt form of rimantadine, a cyclic amine and alpha-methyl derivative of amantadine with antiviral activity. Although the exact mechanism of action of rimantadine is not understood, this agent appears to exert its antiviral effect against influenza A virus by interfering with the function of the transmembrane domain of the viral M2 protein, thereby preventing the uncoating of the virus and subsequent release of infectious viral nucleic acids into the cytoplasm of infected cells. An RNA synthesis inhibitor that is used as an antiviral agent in the prophylaxis and treatment of influenza. See also: Rimantadine (has active moiety). 1-(1-adamantyl)ethanamine is an alkylamine. An RNA synthesis inhibitor that is used as an antiviral agent in the prophylaxis and treatment of influenza. Rimantadine is an Influenza A M2 Protein Inhibitor. The mechanism of action of rimantadine is as a M2 Protein Inhibitor. Rimantadine is an antiviral agent used as therapy for influenza A. Rimantadine has not been associated with clinically apparent liver injury. Rimantadine is a cyclic amine and alpha-methyl derivative of amantadine with antiviral activity. Although the exact mechanism of action of rimantadine is not understood, this agent appears to exert its antiviral effect against influenza A virus by interfering with the function of the transmembrane domain of the viral M2 protein, thereby preventing the uncoating of the virus and subsequent release of infectious viral nucleic acids into the cytoplasm of infected cells. An RNA synthesis inhibitor that is used as an antiviral agent in the prophylaxis and treatment of influenza. See also: Rimantadine Hydrochloride (has salt form). Drug Indication For the prophylaxis and treatment of illness caused by various strains of influenza A virus in adults. FDA Label Mechanism of Action The mechanism of action of rimantadine is not fully understood. Rimantadine appears to exert its inhibitory effect early in the viral replicative cycle, possibly inhibiting the uncoating of the virus. The protein coded by the M2 gene of influenza A may play an important role in rimantadine susceptibility. Rimantadine is thought to exert its inhibitory effect early in the viral replicative cycle, possibly by blocking or greatly reducing the uncoating of viral RNA within host cells. Genetic studies suggest that a single amino acid change on the transmembrane portion of the M2 protein can completely eliminate influenza A virus susceptibility to rimantadine. Rimantadine, like amantadine, inhibits viral replication by interfering with the influenza A virus M2 protein, an integral membrane protein. The M2 protein of influenza A functions as an ion channel and is important in at least 2 aspects of virus replication, disassembly of the infecting virus particle and regulation of the ionic environment of the transport pathway. By interfering with the ion channel function of the M2 protein, rimantadine inhibits 2 stages in the replicative cycle of influenza A. Early in the virus reproductive cycle, rimantadine inhibits uncoating of the virus particle, presumably by inhibiting the acid-mediated dissociation of the virion nucleic acid and proteins, which prevents nuclear transport of viral genome material. Rimantadine also prevents viral maturation in some strains of influenza A (e.g., H7 strains) by promoting pH-induced conformational changes in influenza A hemagglutinin during its intracellular transport late in the replicative cycle. Adsorption of the virus to and penetration into cells do not appear to be affected by rimantadine. In addition, rimantadine does not interfere with the synthesis of viral components (e.g., RNA-directed RNA polymerase activity). Therapeutic Uses Rimantadine is indicated for the prophylaxis of respiratory tract infections caused by influenza A virus in adults and children, and the treatment of respiratory tract infections caused by influenza A virus in adults./Included in US product labeling/ Prevent infection with various strains of influenza A virues Drug Warnings Swine influenza (H1N1) viruses contain a unique combination of gene segments that have not been reported previously among swine or human influenza viruses in the US or elsewhere. The H1N1 viruses are resistant to amantadine and rimantadine but not to oseltamivir or zanamivir. Elderly patients, particularly those in chronic care facilities, are more likely than younger adults or children to experience adverse effects associated with rimantadine, primarily central nervous system (CNS) and gastrointestinal side effects. FDA Pregnancy Risk Category: C /RISK CANNOT BE RULED OUT. Adequate, well controlled human studies are lacking, and animal studies have shown risk to the fetus or are lacking as well. There is a chance of fetal harm if the drug is given during pregnancy; but the potential benefits may outweigh the potential risk./ Adverse CNS effects (e.g., nervousness, anxiety, impaired concentration, lightheadedness) are less common with usual dosages of rimantadine than amantadine, probably in part because of differences in the pharmacokinetics of the drugs. In a 6-week study of daily 200-mg prophylactic doses of rimantadine hydrochloride or amantadine hydrochloride in healthy adults, about 6 or 13% of patients receiving the respective drug discontinued therapy because of adverse CNS effects versus about 4% of those receiving placebo. While neuropsychiatric (e.g., delirium, marked behavioral changes) or psychomotor dysfunction has occurred in patients receiving amantadine, these effects have not been reported in patients receiving rimantadine. For more Drug Warnings (Complete) data for RIMANTADINE (13 total), please visit the HSDB record page. Pharmacodynamics Rimantadine, a cyclic amine, is a synthetic antiviral drug and a derivate of adamantane, like a similar drug amantadine. Rimantadine is inhibitory to the in vitro replication of influenza A virus isolates from each of the three antigenic subtypes (H1N1, H2H2 and H3N2) that have been isolated from man. Rimantadine has little or no activity against influenza B virus. Rimantadine does not appear to interfere with the immunogenicity of inactivated influenza A vaccine. |
| 分子式 |
C12H22CLN
|
|---|---|
| 分子量 |
215.765
|
| 精确质量 |
215.144
|
| 元素分析 |
C, 66.80; H, 10.28; Cl, 16.43; N, 6.49
|
| CAS号 |
1501-84-4
|
| 相关CAS号 |
13392-28-4 (free); 1501-84-4 (HCl) |
| PubChem CID |
15165
|
| 外观&性状 |
White to off-white crystalline powder
|
| 沸点 |
247.8ºC at 760mmHg
|
| 熔点 |
300ºC
|
| 闪点 |
99.3ºC
|
| 蒸汽压 |
0.0251mmHg at 25°C
|
| LogP |
4.052
|
| tPSA |
26.02
|
| 氢键供体(HBD)数目 |
2
|
| 氢键受体(HBA)数目 |
1
|
| 可旋转键数目(RBC) |
1
|
| 重原子数目 |
14
|
| 分子复杂度/Complexity |
180
|
| 定义原子立体中心数目 |
0
|
| SMILES |
Cl[H].N([H])([H])C([H])(C([H])([H])[H])C12C([H])([H])C3([H])C([H])([H])C([H])(C([H])([H])C([H])(C3([H])[H])C1([H])[H])C2([H])[H]
|
| InChi Key |
OZBDFBJXRJWNAV-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C12H21N.ClH/c1-8(13)12-5-9-2-10(6-12)4-11(3-9)7-12;/h8-11H,2-7,13H2,1H3;1H
|
| 化学名 |
1-(1-adamantyl)ethanamine;hydrochloride
|
| 别名 |
Rimantadine Hydrochloride; 1501-84-4; Flumadine; Rimantadine HCL; 1-(1-ADAMANTYL)ETHYLAMINE HYDROCHLORIDE; Meradane; EXP 126; alpha-Methyl-1-adamantanemethylamine hydrochloride; Rimantadine; Flumadine; Rimantadine HCl
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : 43~50 mg/mL (199.3~231.7 mM)
H2O : ~33.3 mg/mL (~154.5 mM) |
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (11.59 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (11.59 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (11.59 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: 33.33 mg/mL (154.48 mM) in PBS (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶. 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 4.6346 mL | 23.1728 mL | 46.3456 mL | |
| 5 mM | 0.9269 mL | 4.6346 mL | 9.2691 mL | |
| 10 mM | 0.4635 mL | 2.3173 mL | 4.6346 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT01413490 | Completed | Drug: rimantadine | Hepatitis C | The Leeds Teaching Hospitals NHS Trust |
May 2012 | |
| NCT01172847 | Completed | Drug: oseltamivir [Tamiflu] Drug: rimantadine |
Healthy Volunteer | Hoffmann-La Roche | August 2009 | Phase 1 |