| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 1mg |
|
||
| 2mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| Other Sizes |
|
| 靶点 |
SGLT1/2 (sodium/glucose cotransporter 1/2)
|
||
|---|---|---|---|
| 体外研究 (In Vitro) |
体外活性:LX4211 抑制 [14C]AMG 摄取,小鼠 SGLT1 的 IC50 为 62.0 nM,小鼠 SGLT2 的 IC50 为 0.6 nM。
在体外,LX4211是SGLT1和SGLT2的强效双重抑制剂,对人SGLT1的抑制浓度(IC50)为36 nmol/l,对人SGLT2的抑制浓度为1.8 nmol/l。[1] |
||
| 体内研究 (In Vivo) |
为了更好地了解LX4211如何增加GLP-1和PYY水平,我们用口服葡萄糖挑战SGLT1敲除(-/-)小鼠、SGLT2-/-小鼠和LX4211治疗的小鼠。LX4211治疗的小鼠和SGLT1-/-小鼠在含葡萄糖餐后6小时内血浆GLP-1、血浆PYY和肠葡萄糖水平升高,如曲线下面积(AUC)值所示,而SGLT2-/-小鼠没有反应。LX4211治疗的小鼠和SGLT1-/-小鼠在单独口服葡萄糖后6小时内,GLP-1 AUC值增加,葡萄糖依赖性促胰岛素多肽(GIP)AUC值降低,血糖波动减少。然而,在口服葡萄糖5分钟后,LX4211治疗的小鼠中GLP-1和GIP水平没有增加,而SGLT1-/-小鼠中GLP-1-/-水平降低,这与口服葡萄糖5 min后肠道SGLT1活性降低与GLP-1和GIM水平降低的研究一致。这些数据表明,LX4211通过抑制SGLT1减少肠道葡萄糖吸收,导致GLP-1和PYY释放净增加,GIP释放和血糖波动减少。抑制肠道SGLT1和肾脏SGLT2的能力为LX4211提供了一种新的双重作用机制,可改善2型糖尿病患者的血糖控制。[2]
在小鼠中,LX4211(60 mg/kg,口服)通过抑制 SGLT1 减少肠道葡萄糖吸收,导致 GLP-1 和 PYY 释放净增加,并减少 GIP 释放和血糖波动。在患有 1 型糖尿病的非肥胖易患糖尿病的小鼠中,Sotagliflozin (30 mg/kg) 显着改善血糖控制,而不增加低血糖测量的发生率。 |
||
| 酶活实验 |
血浆中LX4211的定量。[1]
在给药前以及给药后第1、14和28天的0.25、0.5、0.75、1、1.5、2、3、4、6、8、12和24小时收集血液样本,用于测定<强>索格列净(LX4211)血浆浓度。在第7天和第21天给药前立即收集了额外的血液样本,并在第36天收集了一个样本。采集后,立即将血液样本放入冰/水浴中;然后在4°C下以2000g离心15分钟分离血浆。在采集后90分钟内,血浆样本被储存在-70°C的温度下。使用液相色谱-串联质谱检测定量血浆LX4211水平。[1] Sotagliflozin(LX4211)通过抑制肠道钠/葡萄糖共转运蛋白1(SGLT1)减少餐后葡萄糖波动,并通过抑制肾脏SGLT2增加尿葡萄糖排泄(UGE)。在2型糖尿病患者的临床研究中,LX4211似乎通过双重SGLT1/SGLT2抑制来改善血糖控制并促进体重减轻。在这里,研究人员展示了临床前研究,探索了LX4211改善血糖控制和促进减肥的能力。研究人员发现1)LX4211抑制了小鼠、大鼠和狗SGLT1和SGLT2介导的体外葡萄糖转运[3]。 |
||
| 细胞实验 |
LX4211已被证明可以抑制过表达小鼠或人SGLT1或SGLT2的HEK293细胞的葡萄糖转运。如表1所示,LX4211还抑制大鼠和狗SGLT1和SGLT2介导的葡萄糖转运[3]。
|
||
| 动物实验 |
|
||
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Following a single dose, the Tmax of sotagliflozin ranged from 1.25 to 3 hours. Following multiple doses, the Tmax ranged from 2.5 to 4 hours. The estimated oral bioavailability of sotagliflozin is 71%. Sotagliflozin is primarily eliminated via the renal route, with 57% of administered drug material appearing in the urine and 37% appearing in the feces. Sotagliflozin has a mean apparent volume of distribution of 9392 L. In healthy volunteers, the mean apparent clearance of sotagliflozin ranged from 261 to 374 L/h. The mean apparent clearance estimated in a population of mostly type 1 diabetic patients was 239 L/h. Metabolism / Metabolites The major metabolite of sotagliflozin is a 3-O-glucuronide (M19), which comprised ~94% of of the radioactivity in plasma following the oral administration of a radiolabeled dose of sotagliflozin. The M19 metabolite is effectively inactive, with >275-fold less activity at SGLT1 and SGLT2 compared to the parent drug. The primary route of metabolism is via glucuronidation by UGT1A9 (and both UGT1A1 and UGT2B7, to a lesser extent) as well as oxidation via CYP3A4. Biological Half-Life The mean terminal half-life of sotagliflozin ranged from 21 to 35 hours and from 19 to 26 hours for its M19 metabolite. Pharmacokinetic parameters and mean plasma concentration–time profiles are summarized in Table 4. For each LX4211 dose, plasma concentrations were detected within 15 min, increased with increasing dose, and decreased in a biphasic pattern. The maximum plasma LX4211 concentration (Cmax) appeared at 0.5–2.0 h after dosing, and ranged from 82.5–115 ng/ml and 230–307 ng/ml in the 150-mg and 300-mg dose groups, respectively. The increases in Cmax and AUC for plasma concentration over time curve were slightly more than dose-proportional. The median time to reach Cmax (i.e., tmax) was similar on days 14 and 28 for the two dose groups (1.00–1.50 h), with individual values ranging from 0.48 to 2.02 h. Mean plasma LX4211 concentrations at the end of the dosage interval (Cmin) were similar on days 7, 14, 21, and 28, and all were higher than values on day 1, in both the 150- and 300-mg dose groups (Table 4; Supplementary Table S11 online). Cmax and AUC0–tau values, as determined on days 1, 14, and 28, were similar on days 14 and 28, and each was higher than values on day 1 in both dose groups. Collectively, these data support the view that steady state was reached by day 14, and possibly even by day 7, based on the Cmin value. Apparent total clearance of LX4211 from plasma after oral administration (CL/F) and CL/F at steady state (CL/Fss) were similar across dose groups. After multiple doses, CL/Fss was lower on days 14 and 28 than the value observed after a single dose. CL/F on day 1 and CL/Fss on days 14 and 28 were higher than the sum of hepatic blood flow and renal blood flow, suggesting the possibility of unabsorbed LX4211 in the gastrointestinal tract. Mean ± SD values for t1/2 (half-life) were 20.7 ± 13.7 and 13.5 ± 5.3 h in the 150-mg and 300-mg dose groups, respectively. [1] The pharmacokinetic parameters derived for plasma LX4211 are summarized in Table 5. The absorption rate for the LX4211 liquid formulation was approximately threefold faster than for the tablets, with the median Tmax being 3.00 h for each tablet treatment group and 0.875 h for the liquid treatment group (Figure 2f). Also, the mean Cmax was 2- to 2.5-fold lower for the tablet treatments than for the liquid formulation. Although the AUC values associated with each tablet treatment group were similar, both were lower than that of the liquid formulation; this finding suggests that the tablet formulation has lower bioavailability. The mean ± SD values for t1/2 were 13.2 ± 2.8, 19.8 ± 8.8, and 17.9 ± 9.0 h for the 2 × 150-mg tablets, 6 × 50-mg tablets, and liquid formulation, respectively, consistent with once-daily dosing of LX4211. [1] |
||
| 毒性/毒理 (Toxicokinetics/TK) |
Protein Binding
Both sotagliflozin and its major metabolite, M19, are extensively (~98%) protein-bound in plasma, although the specific protein(s) to which they bind have not been elucidated. Sotagliflozin exerts its pharmacologic effects by slowing glucose absorption in the gastrointestinal tract and increasing the excretion of glucose in the urine. It is administered by mouth once daily before the first meal of the day. The use of SGLT2 inhibitors, including sotagliflozin, can cause diabetic ketoacidosis (DKA). Patients, especially those with a higher baseline risk of DKA, should be instructed on how and when to monitor for ketoacidosis and what actions to take when DKA is suspected. SGLT2 inhibitors, including sotagliflozin, also increase the risk of genital infections. This is due to the increase in urinary glucose excretion, which provides a relatively glucose-rich environment in which infectious agents may establish themselves. LX4211 was safe and well tolerated at the doses and schedule employed. There were no treatment-emergent urinary tract infections, genital infections, CV events, or episodes of hypoglycemia, and laboratory data provided no evidence of renal toxicity. Importantly, gastrointestinal AEs were mild and equally divided among the LX4211 and placebo groups. Serum magnesium rose slightly with LX4211 treatment but remained within the normal range, as was observed with dapagliflozin,15 and urinary calcium excretion did not increase in LX4211-treated patients.[1] |
||
| 参考文献 |
|
||
| 其他信息 |
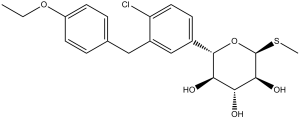
Sotagliflozin is an S-glycosyl compound that is 1-thio-beta-L-xylopyranose in which the anomeric hydroxy group is replaced by a 4-chloro-3-[(4-ethoxyphenyl)methyl]phenyl group and the thiol is replaced by a methylsulfanediyl group. It is an inhibitor of SGLT1 and SGLT2 that is approved to reduce the risk of cardiovascular death, hospitalization for heart failure, and urgent heart failure visit in adults with heart failure or type 2 diabetes mellitus, chronic kidney disease, and other cardiovascular risk. It has a role as a sodium-glucose transport protein subtype 2 inhibitor, a hypoglycemic agent, an antihypertensive agent, a cardioprotective agent and a sodium-glucose transport protein subtype 1 inhibitor. It is a C-glycosyl compound, an aromatic ether, a member of monochlorobenzenes and a S-glycosyl compound.
Sotagliflozin is a dual inhibitor of SGLT1 and SGLT2, the first of its kind, which is approved for use in the EU, in combination with insulin, to improve glycemic control in patients with type 1 diabetes mellitus (T1DM) and a BMI ≥27 kg/m2. Its potency in inhibiting SGLT2 is similar to that of other SGLT2 inhibitors, such as [canagliflozin] and [dapagliflozin], but its potency in inhibiting SGLT1 is >10-fold higher than its predecessors. The added inhibition of intestinal SGLT1 delays glucose absorption in the distal small intestine and colon, thereby reducing post-prandial glucose levels. Sotagliflozin was approved by the EMA under the brand name "Zynquista" on April 26, 2019, for the treatment of type 1 diabetes. A similar approval has also been sought in the US, but the FDA has since published a proposal to refuse the approval because the data submitted did not show that it was safe under the proposed conditions of use. On March 22, 2022, the marketing authorization of sotagliflozin for the treatment of type 1 diabetes mellitus was withdrawn by the EMA due to commercial reasons. In May 2023, sotagliflozin was approved by the FDA to reduce the risk of cardiovascular death and heart failure in patients with high risk factors.[] Sotagliflozin is a Sodium-Glucose Cotransporter 2 Inhibitor. The mechanism of action of sotagliflozin is as a Sodium-Glucose Transporter 2 Inhibitor, and P-Glycoprotein Inhibitor. Sotagliflozin is an orally bioavailable inhibitor of the sodium-glucose co-transporter subtype 1 (SGLT1) and 2 (SGLT2), with potential antihyperglycemic activity. Upon oral administration, sotagliflozin binds to and blocks both SGLT1 in the gastrointestinal (GI) tract and SGLT2 in the kidneys, thereby suppressing the absorption of glucose from the GI tract and the reabsorption of glucose by the proximal tubule into the bloodstream, respectively. This decreases glucose uptake and enhances the urinary excretion of glucose, which lowers and/or normalizes blood glucose levels. SGLT1 is the primary transporter responsible for glucose absorption from the GI tract. SGLT2, a transport protein exclusively expressed in the proximal renal tubules, mediates approximately 90% of renal glucose reabsorption from tubular fluid. Drug Indication In the US, sotagliflozin is indicated to reduce the risk of cardiovascular death and heart failure in adults with heart failure, type 2 diabetes mellitus, chronic kidney disease, and other cardiovascular risk factors. Zynquista is indicated as an adjunct to insulin therapy to improve glycaemic control in adults with type 1 diabetes mellitus with a Body Mass Index (BMI) ⥠27 kg/m2, who have failed to achieve adequate glycaemic control despite optimal insulin therapy. , Treatment of type I diabetes mellitus Treatment of type II diabetes mellitus Mechanism of Action Sodium-glucose co-transporter types 1 and 2 (SGLT1 and SGLT2) are integral in the transport of glucose in the body. SGLT1 is the major transporter for glucose absorption in the gastrointestinal tract, while SGLT2 is the predominant transporter responsible for reabsorption of glucose in the glomerulus. Sotagliflozin is a dual inhibitor of both SGLT1 and SGLT2. Inhibition of SGLT1 results in a delay in glucose absorption and a blunting of postprandial hyperglycemia, while inhibition of SGLT2 reduces renal reabsorption of filtered glucose, thereby increasing urinary glucose excretion. Thirty-six patients with type 2 diabetes mellitus (T2DM) were randomized 1:1:1 to receive a once-daily oral dose of placebo or 150 or 300 mg of the dual SGLT1/SGLT2 inhibitor LX4211 for 28 days. Relative to placebo, LX4211 enhanced urinary glucose excretion by inhibiting SGLT2-mediated renal glucose reabsorption; markedly and significantly improved multiple measures of glycemic control, including fasting plasma glucose, oral glucose tolerance, and HbA(1c); and significantly lowered serum triglycerides. LX4211 also mediated trends for lower weight, lower blood pressure, and higher glucagon-like peptide-1 levels. In a follow-up single-dose study in 12 patients with T2DM, LX4211 (300 mg) significantly increased glucagon-like peptide-1 and peptide YY levels relative to pretreatment values, probably by delaying SGLT1-mediated intestinal glucose absorption. In both studies, LX4211 was well tolerated without evidence of increased gastrointestinal side effects. These data support further study of LX4211-mediated dual SGLT1/SGLT2 inhibition as a novel mechanism of action in the treatment of T2DM.[1] Treatments that lower blood glucose levels and body weight should benefit patients with type 2 diabetes mellitus (T2DM). We developed LX4211 [(2S,3R,4R,5S,6R)-2-(4-chloro-3-(4-ethoxybenzyl)phenyl)-6-(methylthio)tetrahydro-2H-pyran-3,4,5-triol], an orally available small molecule that decreases postprandial glucose excursions by inhibiting intestinal sodium/glucose cotransporter 1 (SGLT1) and increases urinary glucose excretion (UGE) by inhibiting renal SGLT2. In clinical studies of patients with T2DM, LX4211 appears to act through dual SGLT1/SGLT2 inhibition to improve glycemic control and promote weight loss. Here, we present preclinical studies that explored the ability of LX4211 to improve glycemic control and promote weight loss. We found that 1) LX4211 inhibited in vitro glucose transport mediated by mouse, rat, and dog SGLT1 and SGLT2; 2) a single daily LX4211 dose markedly increased UGE for >24 hours in mice, rats, and dogs; and 3) in the KK.Cg-Ay/J heterozygous (KKA(y)) mouse model of T2DM, LX4211 lowered A1C and postprandial glucose concentrations while increasing postprandial glucagon-like peptide 1 concentrations. Also, long-term LX4211 treatment 1) decreased oral glucose tolerance test (OGTT) glucose excursions, increased OGTT 30-minute insulin concentrations and increased pancreatic insulin content in KKA(y) mice; and 2) decreased weight gain in dogs and rats but not in KKA(y) mice while increasing food consumption in dogs, rats, and KKA(y) mice; in these KKA(y) mice, calories lost through UGE were completely offset by calories gained through hyperphagia. These findings suggest that LX4211 improves glycemic control by dual SGLT1/SGLT2 inhibition in mice as in humans, and that the LX4211-mediated weight loss observed in patients with T2DM may be attenuated by LX4211-mediated hyperphagia in some of these individuals.[3] |
| 分子式 |
C21H25CLO5S
|
|
|---|---|---|
| 分子量 |
424.94
|
|
| 精确质量 |
424.111
|
|
| 元素分析 |
C, 59.36; H, 5.93; Cl, 8.34; O, 18.83; S, 7.55
|
|
| CAS号 |
1018899-04-1
|
|
| 相关CAS号 |
|
|
| PubChem CID |
24831714
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 密度 |
1.4±0.1 g/cm3
|
|
| 沸点 |
607.9±55.0 °C at 760 mmHg
|
|
| 闪点 |
321.4±31.5 °C
|
|
| 蒸汽压 |
0.0±1.8 mmHg at 25°C
|
|
| 折射率 |
1.642
|
|
| LogP |
5.63
|
|
| tPSA |
104.45
|
|
| 氢键供体(HBD)数目 |
3
|
|
| 氢键受体(HBA)数目 |
6
|
|
| 可旋转键数目(RBC) |
6
|
|
| 重原子数目 |
28
|
|
| 分子复杂度/Complexity |
476
|
|
| 定义原子立体中心数目 |
5
|
|
| SMILES |
ClC1C([H])=C([H])C(=C([H])C=1C([H])([H])C1C([H])=C([H])C(=C([H])C=1[H])OC([H])([H])C([H])([H])[H])[C@@]1([H])[C@@]([H])([C@]([H])([C@@]([H])([C@]([H])(O1)SC([H])([H])[H])O[H])O[H])O[H]
|
|
| InChi Key |
QKDRXGFQVGOQKS-CRSSMBPESA-N
|
|
| InChi Code |
InChI=1S/C21H25ClO5S/c1-3-26-15-7-4-12(5-8-15)10-14-11-13(6-9-16(14)22)20-18(24)17(23)19(25)21(27-20)28-2/h4-9,11,17-21,23-25H,3,10H2,1-2H3/t17-,18-,19+,20+,21-/m1/s1
|
|
| 化学名 |
(2S,3R,4R,5S,6R)-2-[4-chloro-3-[(4-ethoxyphenyl)methyl]phenyl]-6-methylsulfanyloxane-3,4,5-triol
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (5.88 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (5.88 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL 澄清 DMSO 储备液添加到 900 μL 玉米油中并混合均匀。 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.3533 mL | 11.7664 mL | 23.5327 mL | |
| 5 mM | 0.4707 mL | 2.3533 mL | 4.7065 mL | |
| 10 mM | 0.2353 mL | 1.1766 mL | 2.3533 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT05405556 | Recruiting | Diagnostic Test: eGFR reporting | Kidney Transplant | Martina McGrath, MD | October 17, 2022 | Phase 2 |
| NCT05562063 | Recruiting | Drug: Sotagliflozin Drug: Placebo |
Heart Failure With Preserved Ejection Fraction |
Juan Badimon | October 26, 2022 | Phase 4 |
| NCT06217302 | Not yet recruiting | Drug: Sotagliflozin Drug: Placebo |
Diabetic Nephropathies Kidney Failure, Chronic |
Alessandro Doria | May 2024 | Phase 3 |
| NCT06147232 | Not yet recruiting | Drug: Sotagliflozin Drug: Placebo |
Nephropathy Albuminuria |
Steno Diabetes Center Copenhagen |
February 2024 | Phase 4 |
| NCT05696366 | Not yet recruiting | Drug: Sotagliflozin Drug: Volagidemab |
Type 1 Diabetes | University of California, San Diego |
February 2023 | Phase 1 Phase 2 |