| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| 5g |
|
||
| 10g |
|
||
| Other Sizes |
|
| 靶点 |
Leishmania;Plasmodium
|
|---|---|
| 体外研究 (In Vitro) |
两性霉素 B 的输注相关毒性(包括发烧和寒战)限制了其给药。这种效应被认为是由产生促炎细胞因子的先天免疫细胞引起的。当暴露于两性霉素 B 时,TLR2 和 CD14 表达细胞会释放炎症细胞因子并进行信号转导[1]。两性霉素 B 的相对毒性限制了其用途,因为它会与胆固醇(哺乳动物细胞膜中发现的主要甾醇)相互作用。在亚相中,两性霉素 B 以高度聚集状态或前胶束状态分布[2]。两性霉素 B 仅杀死单细胞利什曼原虫前鞭毛体 (LP),当它们形成可渗透小阳离子和阴离子的水孔时。两性霉素 B (0.1 mM) 在负载 KCl 的脂质体中诱导极化电位,并悬浮在等渗蔗糖溶液中,表明 K+ 渗漏。当添加两性霉素 B (0.05 mM) 时,负膜电位几乎完全崩溃,表明 Na+ 进入细胞[3]。
|
| 体内研究 (In Vivo) |
在仓鼠痒病模型中,两性霉素 B 导致潜伏期延长,PrPSc 的积累减少。在患有传染性亚急性海绵状脑病 (TSSE) 的小鼠中,两性霉素 B 显着降低 PrPSc 水平[4]。在小鼠疟疾中,两性霉素 B 直接影响恶性疟原虫,并对寄生虫血症、宿主存活和受感染红细胞的红细胞凋亡产生影响。在感染伯氏疟原虫的小鼠中,两性霉素 B 往往会推迟寄生虫血症的发生,并大大推迟宿主死亡[5]。
|
| 酶活实验 |
Polyfect试剂和DEAE-葡聚糖分别用于瞬时转染THP-1和HEK293细胞。编码 NF-κB 依赖性 pELAM-luc 荧光素酶报告基因、TLR2、TLR4、CD14 和 MD2 的基因存在于转染的质粒中。在12孔板中加入细胞(5×105 THP-1或1×105 HEK293),18小时后洗涤并刺激5小时。按照说明,在报告裂解缓冲液中裂解细胞,并使用 Monolight 3010 发光计和 Promega 荧光素酶底物对裂解物进行发光分析。
|
| 细胞实验 |
AmB 诱导的针对利什曼原虫前鞭毛体的细胞死亡动力学通过使用溴化乙锭 (EB)(一种结合 DNA 的化合物)的荧光测定法进行监测。 SPEX Fluorolog II 分光光度计用于测量 365–580 nm 激发发射波长的荧光。将前鞭毛体添加到含有 2 mL 各种缓冲溶液(始终含有 10 mM 葡萄糖和 50 mM EB)的荧光比色皿中,并以 25×106 个细胞/mL 的终浓度轻轻搅拌孵育 5 分钟。获得信号后为了稳定,引入 AmB 并溶解在二甲亚砜中。始终添加洋地黄皂苷 (50 mg/mL) 以实现最大程度的 EB 掺入。将 75 mM TRIS (pH 4 7.6) 缓冲液应用于所有溶液,其中还含有 150 mM KCl (BK+)、150 mM NaCl (BNa+)、150 mM 氯化胆碱、100 mM 蔗糖和 100 mM NaCl。始终使用称为 SW2 渗透压计的精密仪器将所有溶液的渗透压调整至 390±5 mOsm。
|
| 动物实验 |
Efficacy of PEO-b-p(HASA)/AmB. Efficacy was assessed by organism killing in the kidneys of a neutropenic murine model of disseminated fungal infection as described previously by Andes et al. A clinical isolate of Candida albicans (K-1) was grown and quantified on SDA. For 24 h prior to infection, the organism was subcultured at 35 °C on SDA slants. A 106 CFU/mL inoculum (CFU, colony forming units) was prepared by placing six fungal colonies into 5 mL of sterile, depyrogenated normal (0.9%) saline warmed to 35 °C. Six-week-old ICR/Swiss specific-pathogen-free female mice were obtained from Harlan Sprague Dawley . All animal studies were approved by the Animal Research Committee of the William S. Middleton Memorial VA Hospital (Madison, WI). The mice were weighed (23−27 g) and given intraperitoneal injections of cyclophosphamide to render neutropenia. (For the purposes of this study, neutropenia was defined as <100 polymorphonuclear leukocytes/mm3.) Each mouse was dosed with 150 mg/kg of cyclophosphamide 4 days prior to infection and 100 mg/kg 1 day before infection. Disseminated candidiasis was induced via tail vein injection of 100 μL of inoculum. [5]
The AmB/polymeric micelle formulations or micelle blanks were reconstituted with 1.0 mL of 5% dextrose. The treatment group was given single 200 μL intravenous (iv) injections of reconstituted AmB/PEO-b-p(HASA), 91% 2 h postinfection. Doses were calculated in terms of mg of AmB/kg of body weight. Control animals were given a placebo of “blank” polymeric micelles. Over time, two animals per experimental condition were sacrificed by CO2 asphyxiation. The kidneys from each animal were removed and homogenized. The homogenate was diluted 10-fold with 9% saline and plated on SDA. The plates were then incubated for 24 h at 35 °C and inspected for CFU determination. The lower limit of detection for this technique is 100 CFU/mL. To compare the antifungal activity of the AmB/ micelle formulations with that of Fungizone, animals were dosed with equivalent doses of AmB as Fungizone as described above. The control animals for the Fungizone group received 200 μL iv injections of 5% dextrose. All results are expressed as the mean CFU per kidney for two animals (four kidneys total). The change in the area under the time−kill curves was calculated by ΔAUCTK = AUCcontrol − AUCtreatment. Outcomes were compared using ANOVA on ranks.[5] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Bioavailability is 100% for intravenous infusion. 39 +/- 22 mL/hr/kg [febrile neutropenic cancer and bone marrow transplant patients receiving infusion of 1 mg/kg/day at Day 1] 17 +/- 6 mL/hr/kg [febrile neutropenic cancer and bone marrow transplant patients receiving infusion of 1 mg/kg/day 3-20 days later] 51 +/- 44 mL/hr/kg [febrile neutropenic cancer and bone marrow transplant patients receiving infusion of 2.5 mg/kg/day at Day 1] 22 +/- 15 mL/hr/kg [febrile neutropenic cancer and bone marrow transplant patients receiving infusion of 2.5 mg/kg/day 3-20 days later] 21 +/- 14 mL/hr/kg [febrile neutropenic cancer and bone marrow transplant patients receiving infusion of 5 mg/kg/day at Day 1] 11 +/- 6 mL/hr/kg [febrile neutropenic cancer and bone marrow transplant patients receiving infusion of 5 mg/kg/day 3-20 days later] The pharmacokinetics of amphotericin B vary substantially depending on whether the drug is administered as conventional amphotericin B (formulated with sodium desoxycholate), amphotericin B cholesteryl sulfate complex, amphotericin B lipid complex, or amphotericin B liposomal, and pharmacokinetic parameters reported for one amphotericin B formulation should not be used to predict the pharmacokinetics of any other amphotericin B formulation. Amphotericin B is poorly absorbed from the GI tract and must be given parenterally to treat systemic fungal infections. In one study, immediately after completion of iv infusion of 30 mg of amphotericin B (administered over a period of several hours), average peak serum concentrations were about 1 ug/ml; when the dose was 50 mg, average peak serum concentrations were approximately 2 ug/ml. Immediately after infusion, no more than 10% of the amphotericin B dose can be accounted for in serum. Average minimum serum concentrations (recorded just prior to the next drug infusion) of approximately 0.4 ug/ml have been reported when doses of 30 mg were given daily or when doses of 60 mg were given every other day. Information on the distribution of amphotericin B is limited, although distribution is apparently multicompartmental. The volume of distribution of the drug following administration of conventional amphotericin B has been reported to be 4 L/kg; the volume of distribution at steady state after administration of amphotericin B cholesteryl sulfate is reported to be 3.8-4.1 L/kg. Amphotericin B concentrations attained in inflamed pleura, peritoneum, synovium, and aqueous humor following IV administration of conventional amphotericin B reportedly are about 60% of concurrent plasma concentrations; the drug also is distributed into vitreous humor, pleural, pericardial, peritoneal, and synovial fluid. Amphotericin B reportedly crosses the placenta and low concentrations are attained in amniotic fluid. Following IV administration of conventional amphotericin B, CSF concentrations of the drug are approximately 3% of concurrent serum concentrations. To achieve fungistatic CSF concentrations, the drug must usually be administered intrathecally. In patients with meningitis, intrathecal administration of 0.2-0.3 mg of conventional amphotericin B via a subcutaneous reservoir has produced peak CSF concentrations of 0.5-0.8 ug/mL; 24 hours after the dose, CSF concentrations were 0.11-0.29 ug/mL. Amphotericin B is removed from the CSF by arachnoid villi and appears to be stored in the extracellular compartment of the brain, which may act as a reservoir for the drug. For more Absorption, Distribution and Excretion (Complete) data for AMPHOTERICIN B (14 total), please visit the HSDB record page. Metabolism / Metabolites Exclusively renal Biological Half-Life An elimination half-life of approximately 15 days follows an initial plasma half-life of about 24 hours. Amphotericin B cholesteryl sulfate complex has a distribution half-life of 3.5 minutes and an elimination half-life of 27.5-28.2 hours. /Amphotericin B cholesteryl sulfate complex/ Following IV administration of conventional amphotericin B in patients whose renal function is normal prior to therapy, the initial plasma half-life is approximately 24 hours. After the first 24 hours, the rate at which amphotericin B is eliminated decreases and an elimination half-life of approximately 15 days has been reported. Elimination, half life: Neonates: Variable (range, 18 to 62.5 hours). Children: Variable (range, 5.5 to 40.3 hours). Adults: Approximately 24 hours. Terminal half life: Approximately 15 days. NOTE: There is large interindividual variation among neonates in the elimination of amphotericin B. Amphotericin B may persist in the circulation of neonates for up to 17 days after it has been discontinued. . The half life of elimination of amphotericin B from the lungs /of rats/ was 4.8 days according to serial sacrifices done after a single dose of 3.2 mg of aerosol doses of amphotericin B per kg. |
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation Although no information exists on the milk excretion of amphotericin B, it is highly protein bound, has a large molecular weight, is virtually unabsorbed orally and has been use directly in the mouths of infants; therefore, most reviewers consider it acceptable to use in nursing mothers. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding Highly bound (>90%) to plasma proteins. Interactions Since nephrotoxic effects may be additive, the concurrent or sequential use of amphotericin B and other drugs with similar toxic potentials (eg, aminoglycosides, capreomycin, colistill, cisplatin, cyclosporine, methoxyflurane, pentamidine, polymyxin B, vancomycin) should be avoided, if possible. Corticosteroids reportedly may enhance the potassium depletion caused by amphotericin B and should not be used concomitantly unless necessary to control adverse reactions to amphotericin B. Antineoplastic agents (eg, mechlorethamine) may enhance the potential for renal toxicity, bronchospasm, and hypotension in patients receiving amphotericin B and such concomitant therapy should be used only with great caution. In a randomized, double-blind study that evaluated use of conventional IV amphotericin B and amphotericin B cholesteryl sulfate complex in febrile neutropenic patients with normal baseline serum creatinine concentrations, the incidence of renal toxicity (defined as a doubling or an increase of 1 mg/dL or more from baseline serum creatinine or a 50% or greater decrease from baseline in calculated creatinine clearance) was 31% in adults and pediatric patients who received amphotericin B cholesteryl sulfate complex concomitantly with cyclosporine or tacrolimus compared with 68% in those who received conventional amphotericin B concomitantly with these agents. In adults and pediatric patients who did not receive cyclosporine or tacrolimus therapy, the incidence of renal toxicity was 8% in those who received amphotericin B cholesteryl sulfate complex and 35% in those who received conventional amphotericin B. For more Interactions (Complete) data for AMPHOTERICIN B (15 total), please visit the HSDB record page. Non-Human Toxicity Values LD50 Mouse iv 4 mg/kg LD50 Mouse ip 88 mg/kg |
| 参考文献 |
|
| 其他信息 |
Therapeutic Uses
Ambecides; Antibiotics, Antifungal; Antibiotics, Macrolide; Antiprotozoal Agents MEDICATION: Antifungal; (VET): Antifungal MEDICATION (VET): ... Blastomycosis, histoplasmosis. Parenteral amphotericin B is used as a secondary agent in the treatment of paracoccidioidomycosis caused by Paracoccidioide brasillensis. /NOT included in US product labeling/ For more Therapeutic Uses (Complete) data for AMPHOTERICIN B (19 total), please visit the HSDB record page. Drug Warnings Rash (including maculopapular or vesiculobullous rash), purpura, pruritus, urticaria, sweating, exfoliative dermatitis, erythema multiforme, alopecia, dry skin, and skin discoloration or ulcer, have been reported in patients receiving amphotericin B. IV administration of conventional amphotericin B, amphotericin B cholesteryl sulfate complex, amphotericin B lipid complex, or amphotericin B liposomal may cause erythema, pain, or inflammation at the injection site. Phlebitis or thrombophlebitis has been reported with conventional IV amphotericin B. The manufacturer of conventional IV amphotericin B and some clinicians suggest that the addition of 500-1000 units of heparin to the amphotericin B infusion, the use of a pediatric scalp-vein needle, or alternate-day therapy may decrease the incidence of thrombophlebitis. Extravasation of the drug causes local irritation. Conventional IV amphotericin B is associated with a high incidence of adverse effects, and most patients who receive the drug experience potentially severe adverse effects at some time during the course of therapy. Acute infusion reactions (e.g., fever, chills, headache, nausea, vomiting) and nephrotoxicity are the most frequent adverse reactions to conventional IV amphotericin B. Although clinical experience with amphotericin B cholesteryl sulfate complex, amphotericin B lipid complex, and amphotericin B liposomal is limited to date, these drugs appear to be better tolerated than conventional IV amphotericin B. As with conventional IV amphotericin B, the most frequent adverse reactions to amphotericin B cholesteryl sulfate complex, amphotericin B lipid complex, or amphotericin B liposomal are acute infusion reactions; however, data accumulated to date indicate that lipid-based and liposomal formulations of amphotericin B may be associated with a lower overall incidence of adverse effects and a lower incidence of hematologic and renal toxicity than the conventional formulation of the drug. Acute infusion reactions consisting of fever, shaking chills, hypotension, anorexia, nausea, vomiting, headache, dyspnea, and tachypnea may occur 1-3 hours after initiation of IV infusions of conventional amphotericin B, amphotericin B cholesteryl sulfate, amphotericin B lipid complex, or amphotericin B liposomal. These reactions are most severe and occur most frequently with initial doses and usually lessen with subsequent doses. Fever (with or without shaking chills) may occur as soon as 15-20 minutes after IV infusions of conventional amphotericin B are started. The majority of patients receiving conventional IV amphotericin B (50-90%) exhibit some degree of intolerance to initial doses of the drug, even when therapy is initiated with low doses. Although these reactions become less frequent following subsequent doses or administration of the drug on alternate days, they recur if conventional IV amphotericin B therapy is interrupted and then reinstituted. For more Drug Warnings (Complete) data for AMPHOTERICIN B (18 total), please visit the HSDB record page. Pharmacodynamics Amphotericin B shows a high order of in vitro activity against many species of fungi. Histoplasma capsulatum, Coccidioides immitis, Candida species, Blastomyces dermatitidis, Rhodotorula, Cryptococcus neoformans, Sporothrix schenckii, Mucor mucedo, and Aspergillus fumigatus are all inhibited by concentrations of amphotericin B ranging from 0.03 to 1.0 mcg/mL in vitro. While Candida albicans is generally quite susceptible to amphotericin B, non-albicans species may be less susceptible. Pseudallescheria boydii and Fusarium sp. are often resistant to amphotericin B. The antibiotic is without effect on bacteria, rickettsiae, and viruses. |
| 精确质量 |
923.487
|
|---|---|
| 元素分析 |
C, 61.09; H, 7.96; N, 1.52; O, 29.43
|
| CAS号 |
1397-89-3
|
| 相关CAS号 |
Amphotericin B trihydrate;1202017-46-6;Amphotericin B-13C6
|
| PubChem CID |
5280965
|
| 外观&性状 |
Light yellow to yellow solid
|
| 密度 |
1.3±0.1 g/cm3
|
| 沸点 |
1140.4±65.0 °C at 760 mmHg
|
| 熔点 |
>170°C
|
| 闪点 |
643.5±34.3 °C
|
| 蒸汽压 |
0.0±0.6 mmHg at 25°C
|
| 折射率 |
1.614
|
| LogP |
1.16
|
| tPSA |
319.61
|
| 氢键供体(HBD)数目 |
12
|
| 氢键受体(HBA)数目 |
18
|
| 可旋转键数目(RBC) |
3
|
| 重原子数目 |
65
|
| 分子复杂度/Complexity |
1670
|
| 定义原子立体中心数目 |
19
|
| SMILES |
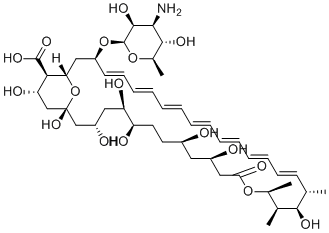
C[C@H]1/C=C/C=C/C=C/C=C/C=C/C=C/C=C/[C@@H](C[C@H]2[C@@H]([C@H](C[C@](O2)(C[C@H](C[C@H]([C@@H](CC[C@H](C[C@H](CC(=O)O[C@H]([C@@H]([C@@H]1O)C)C)O)O)O)O)O)O)O)C(=O)O)O[C@H]3[C@H]([C@H]([C@@H]([C@H](O3)C)O)N)O
|
| InChi Key |
APKFDSVGJQXUKY-INPOYWNPSA-N
|
| InChi Code |
InChI=1S/C47H73NO17/c1-27-17-15-13-11-9-7-5-6-8-10-12-14-16-18-34(64-46-44(58)41(48)43(57)30(4)63-46)24-38-40(45(59)60)37(54)26-47(61,65-38)25-33(51)22-36(53)35(52)20-19-31(49)21-32(50)23-39(55)62-29(3)28(2)42(27)56/h5-18,27-38,40-44,46,49-54,56-58,61H,19-26,48H2,1-4H3,(H,59,60)/b6-5+,9-7+,10-8+,13-11+,14-12+,17-15+,18-16+/t27-,28-,29-,30+,31+,32+,33-,34-,35+,36+,37-,38-,40+,41-,42+,43+,44-,46-,47+/m0/s1
|
| 化学名 |
(1R,3S,5R,6R,9R,11R,15S,16R,17R,18S,19E,21E,23E,25E,27E,29E,31E,33R,35S,36R,37S)-33-(((2R,3S,4S,5S,6R)-4-amino-3,5-dihydroxy-6-methyltetrahydro-2H-pyran-2-yl)oxy)-1,3,5,6,9,11,17,37-octahydroxy-15,16,18-trimethyl-13-oxo-14,39-dioxabicyclo[33.3.1]nonatriaconta-19,21,23,25,27,29,31-heptaene-36-carboxylic acid
|
| 别名 |
Amphotericin B;NSC 527017;Ambisome NSC527017;Amphozone FungilinFungizoneAMPH-B Fungizone Liposomal Amphotericin B NSC-527017
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 本产品在运输和储存过程中需避光。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO :~50 mg/mL (~54.11 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 10 mg/mL (10.82 mM) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 悬浮液; 超声和加热处理
例如,若需制备1 mL的工作液,可将100 μL 100.0 mg/mL澄清DMSO储备液加入400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: 10 mg/mL (10.82 mM) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 悬浮液; 超声和加热处理 例如,若需制备1 mL的工作液,可将 100 μL 100.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
CAMB/MAT2203 in Patients With Mucocutaneous Candidiasis
CTID: NCT02629419
Phase: Phase 2 Status: Completed
Date: 2024-08-07