| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| Other Sizes |
|
| 靶点 |
Antifungal
|
|---|---|
| 体外研究 (In Vitro) |
即使浓度高达 100 μM,Manogepix 对人 Pig-Wp 也没有抑制作用,但它确实降低了白色念珠菌 Gwt1p 和烟曲霉 Gwt1p 的肌醇酰化活性,IC50 为 0.3 至 0.6 μM。对用 Manogepix 处理的白色念珠菌细胞表面 GPI 锚定蛋白 ALS1 的表达进行了检查,结果显示其表达远低于未处理的细胞,证实了真菌糖基磷脂酰肌醇 (GPI) 生物合成的抑制。当浓度高于其最低抑菌浓度 (MIC) 时,manogepix 会抑制白色念珠菌的芽管产生、聚苯乙烯表面粘附以及生物膜形成 [1]。
|
| 体内研究 (In Vivo) |
通过 manogepix 治疗(口服给药;每天两次;持续三天;无特定病原体雌性 ICR 小鼠;2.5 mg/kg、5 mg/kg 和 10 mg/kg),活 C 的数量减少。口腔白色念珠菌细胞呈剂量依赖性[2]。
|
| 酶活实验 |
体外药敏试验。[2]
E1210和参比化合物的mic采用临床与实验室标准协会(CLSI) M27-A3和M38-A2文件中详细说明的肉汤微量稀释法测定。使用RPMI 1640培养基,用0.165 m3 -(N-morpholino)-丙磺酸(MOPS)缓冲至pH 7.0。结果表示为三个独立实验得出的每种化合物的中位数MIC。 对通过抑制糖基磷脂酰肌醇(GPI)生物合成而起作用的新型抗真菌药物的持续研究导致了E1210的设计。本研究通过评价E1210对白色念珠菌GWT1 (Orf19.6884)蛋白、烟曲霉GWT1 (AFUA_1G14870)蛋白和人猪- w蛋白抑制活性的选择性,在GPI生物合成途径早期催化GPI肌醇酰化,进而评价E1210对白色念珠菌关键毒力因子的影响。E1210在0.3 ~ 0.6 μM的50%抑制浓度(IC(50)s)范围内对白色念珠菌Gwt1p和烟曲霉Gwt1p肌醇酰化活性有抑制作用,但在100 μM的浓度下对人猪- wp无抑制作用。为了证实真菌GPI生物合成的抑制作用,研究了E1210处理后白色念珠菌细胞表面上GPI锚定蛋白ALS1蛋白的表达,结果表明E1210处理后白色念珠菌细胞表面上GPI锚定蛋白ALS1蛋白的表达明显低于未经处理的细胞。然而,粗提物中的ALS1蛋白水平与细胞表面的RHO1蛋白水平几乎相同。此外,当E1210浓度高于其MIC时,E1210可抑制白色念珠菌芽管的形成、对聚苯乙烯表面的粘附以及生物膜的形成。这些结果表明,E1210选择性地抑制了Gwt1p催化的真菌特异性GPI的肌醇酰化,从而抑制GPI锚定蛋白的成熟,并且E1210通过抑制GPI的生物合成抑制了一些重要毒力因子的表达。[1] |
| 细胞实验 |
同时测定了白念珠菌细胞粗提物中Als1p的含量。细胞在E1210存在下,35℃孵育1 h。孵育后,将培养物在4℃下1000 × g离心10分钟,将微球悬浮在含有真菌蛋白酶抑制剂鸡尾酒的50 mM磷酸钾缓冲液(pH 7.4)中。将细胞悬浮液与等重量的玻璃微珠混合,并用细胞干扰剂均匀化。然后将未破碎的细胞和玻璃珠离心取出。所得上清液为粗提物。用ELISA法测定粗提物中Als1蛋白的含量。捕获抗体为抗als1抗体,捕获抗体为抗c。白念珠菌用酶标兔抗体(ViroStat Inc., Portland, ME)作为二抗。每个浓度的酶联免疫吸附试验一式两份,最终值以三次测定的平均值表示。估计蛋白浓度是为了标准化Als1p的量。[1]
|
| 动物实验 |
Animal/Disease Models: Specific-pathogen-free female ICR mice (5 weeks; ~25 g) with C. albicans[2]
Doses: 2.5 mg/kg, 5 mg/kg and 10 mg /kg Route of Administration: Oral administration; twice (two times) daily; for 3 days Experimental Results: decreased the number of viable C. albicans cells in the oral cavity in a dose-dependent manner. Oropharyngeal candidiasis model. [2] C. albicans was used to infect mice that were immunosuppressed with cortisone, and the number of C. albicans cells in the oral cavity of each mouse was measured following drug treatment. ICR mice were immunosuppressed using 4 mg of subcutaneously administered cortisone acetate given 1 day before and 3 days after infection. The mice were also given 1 mg/ml tetracycline hydrochloride via their drinking water, starting on the day of cortisone administration and continuing throughout the experiment, in order to prevent bacterial infection. C. albicans IFM49971 was grown on Sabouraud dextrose agar (SDA) at 35°C for 2 days. The cells were suspended in sterile normal saline. The cells were counted with a hemocytometer and adjusted to the required density with sterile normal saline. The mice were then anesthetized with chlorpromazine hydrochloride (0.5 mg/mouse given subcutaneously). By use of a micropipette, aliquots (10 μl) of C. albicans IFM49971 suspension were inoculated into the oral cavities of the anesthetized mice. Then the challenge dose of 4 × 105 CFU of C. albicans (CFU)/mouse was given. This was followed with either E1210 orally administered twice daily (BID) or fluconazole orally administered once daily (QD) for three consecutive days starting 3 days after infection. The control group was given the equivalent volume of 5% glucose BID. The mice were anesthetized with chlorpromazine hydrochloride (0.5 mg/mouse subcutaneously) the day after the final dose of the study drug. Efficacy was assessed by determination of the number of C. albicans cells in the oral cavity of each mouse after study drug treatment. The oral cavity (that is, the cheek, tongue, and soft palate) was thoroughly swabbed using a fine-tipped cotton swab. After swabbing, the cotton end was placed into a test tube containing 1 ml sterile normal saline. The cells recovered were suspended in sterile normal saline by mixing them on a vortex mixer before being cultured, after serial 10-fold dilutions, on SDA plates supplemented with ampicillin (0.1 mg/ml). The SDA plates were incubated at 35°C overnight, and then the viable cells were counted as the number of CFU. The cell number was expressed in units of log10 CFU/swab. The lowest detectable number of cells in the oral cavity was 10 CFU (1 log10 CFU). The viable cell counts were performed in duplicate.[2] Disseminated candidiasis model. [2] ICR mice were immunosuppressed utilizing 5-fluorouracil (5-FU) at 200 mg/kg of body weight subcutaneously administered 6 days prior to infection. These mice were also administered 0.1 mg/ml ciprofloxacin orally via their drinking water, from 2 to 3 days prior to infection to 5 to 7 days after infection, in order to prevent endogenous bacterial infections. C. albicans IFM49971, C. albicans IFM49738, and C. tropicalis E83037 were each cultured on an SDA plate at 35°C for 2 days. The cells from the surface of the agar plate were suspended in sterile normal saline, and the cells were counted with a hemocytometer. The final inoculum was adjusted to the required density using sterile normal saline. Infection was induced in the neutropenic mice by the intravenous administration of 0.2 ml of a C. albicans cell suspension (0.8 to 1.4 × 104 CFU/mouse or 5.3 × 104 CFU/mouse for IFM49971) or of a C. tropicalis cell suspension (3.0 × 105 CFU/mouse) injected into the lateral tail vein. Antifungal therapy was initiated 1 h or 24 h after infection and was continued for three consecutive days (days 0 to 2 or 1 to 3). E1210 or voriconazole was each orally administered two or three times daily, fluconazole was orally administered once daily, and caspofungin or liposomal amphotericin B was intravenously administered once daily. The control group received an equivalent volume of vehicle (5% glucose, 10 ml/kg) orally two or three times daily. In our preliminary studies, the survival curve of control mice receiving vehicle orally was similar to that of mice receiving vehicle intravenously. Therefore, we did not set up the control group to receive vehicle intravenously. The survival rate and survival period were determined over 14 days.[2] View More
Pulmonary aspergillosis model. [2] Disseminated fusariosis model. [2] DBA/2N mice were immunosuppressed with 200 mg/kg of subcutaneously administered 5-FU, 6 days prior to infection. The mice were also administered 0.1 mg/ml ciprofloxacin orally in their drinking water, from 3 days prior to infection until 7 days after infection, to prevent bacterial infections. F. solani IFM50956 was cultured on a PDA plate at 30°C for 7 days. The cells from the surface of the agar plate were suspended in sterile normal saline containing 0.05% Tween 80, and the cells were counted using a hemocytometer. The final inoculum was adjusted to the required density using sterile normal saline containing 0.05% Tween 80. Infection was induced in the neutropenic mice by the intravenous inoculation of a 0.2-ml F. solani cell suspension (5.0 × 103 cells/mouse) into the lateral tail vein. Antifungal therapy was initiated 1 h after infection and was continued for five consecutive days (days 0 to 4). E1210 was orally administered three times a day (TID). The control group received an equivalent volume of 5% glucose orally TID. The survival rate and survival period were determined over 14 days.[2] Pharmacokinetic study. [2] E1210 was intravenously or orally administered to male ICR mice. After administration of E1210, blood samples were drawn from the vena cava of each mouse at designated time points (0.08, 0.25, 0.5, 1, 2, 4, 6, 8 h). Plasma samples were obtained by centrifuging blood. After deproteinization with methanol, the extracted sample was analyzed by liquid chromatography-tandem mass spectrometry (LC/MS/MS). The concentrations of E1210 in plasma were determined by an internal standard method using MassLynx. The pharmacokinetic parameters of E1210 were calculated by model independent analysis.[2] Toxicology study. [2] E1210 was administered orally by gavage once a day for 7 days to male and female Sprague-Dawley rats (3 animals/group/gender) at doses of 100, 300, or 1,000 mg/kg. A control group received an equivalent volume (10 ml/kg) of vehicle (0.4 mol/liter hydrochloric acid). All rats found dead or moribund were necropsied as soon as they were discovered, and all surviving animals were necropsied after 7 days of administration. The following were evaluated: mortality, clinical signs, body weight, food consumption, hematology, blood chemistry, toxicokinetics, hepatic drug-metabolizing enzymes, and macroscopic and microscopic pathologies.[2] |
| 参考文献 |
|
| 其他信息 |
E1210 is a first-in-class, broad-spectrum antifungal with a novel mechanism of action-inhibition of fungal glycosylphosphatidylinositol biosynthesis. In this study, the efficacies of E1210 and reference antifungals were evaluated in murine models of oropharyngeal and disseminated candidiasis, pulmonary aspergillosis, and disseminated fusariosis. Oral E1210 demonstrated dose-dependent efficacy in infections caused by Candida species, Aspergillus spp., and Fusarium solani. In the treatment of oropharyngeal candidiasis, E1210 and fluconazole each caused a significantly greater reduction in the number of oral CFU than the control treatment (P < 0.05). In the disseminated candidiasis model, mice treated with E1210, fluconazole, caspofungin, or liposomal amphotericin B showed significantly higher survival rates than the control mice (P < 0.05). E1210 was also highly effective in treating disseminated candidiasis caused by azole-resistant Candida albicans or Candida tropicalis. A 24-h delay in treatment onset minimally affected the efficacy outcome of E1210 in the treatment of disseminated candidiasis. In the Aspergillus flavus pulmonary aspergillosis model, mice treated with E1210, voriconazole, or caspofungin showed significantly higher survival rates than the control mice (P < 0.05). E1210 was also effective in the treatment of Aspergillus fumigatus pulmonary aspergillosis. In contrast to many antifungals, E1210 was also effective against disseminated fusariosis caused by F. solani. In conclusion, E1210 demonstrated consistent efficacy in murine models of oropharyngeal and disseminated candidiasis, pulmonary aspergillosis, and disseminated fusariosis. These data suggest that further studies to determine E1210's potential for the treatment of disseminated fungal infections are indicated.[2]
|
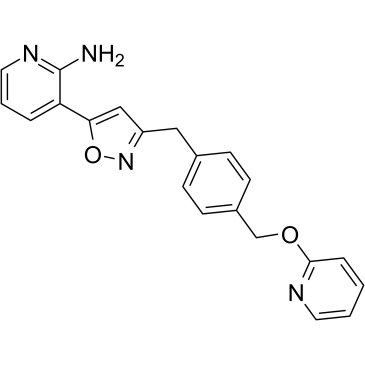
| 分子式 |
C21H18N4O2
|
|---|---|
| 分子量 |
358.4
|
| 精确质量 |
358.142
|
| 元素分析 |
C, 70.38; H, 5.06; N, 15.63; O, 8.93
|
| CAS号 |
936339-60-5
|
| 相关CAS号 |
Fosmanogepix;2091769-17-2
|
| PubChem CID |
16719049
|
| 外观&性状 |
White to light yellow solid powder
|
| 密度 |
1.3±0.1 g/cm3
|
| 沸点 |
569.4±45.0 °C at 760 mmHg
|
| 闪点 |
298.1±28.7 °C
|
| 蒸汽压 |
0.0±1.6 mmHg at 25°C
|
| 折射率 |
1.640
|
| LogP |
3.75
|
| tPSA |
87.1
|
| 氢键供体(HBD)数目 |
1
|
| 氢键受体(HBA)数目 |
6
|
| 可旋转键数目(RBC) |
6
|
| 重原子数目 |
27
|
| 分子复杂度/Complexity |
444
|
| 定义原子立体中心数目 |
0
|
| InChi Key |
WSEKTEUGRLFBSE-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C21H18N4O2/c22-21-18(4-3-11-24-21)19-13-17(25-27-19)12-15-6-8-16(9-7-15)14-26-20-5-1-2-10-23-20/h1-11,13H,12,14H2,(H2,22,24)
|
| 化学名 |
(3-(3-(4-(((Pyridin-2-yl)oxy)methyl)benzyl)isoxazol-5-yl)pyridin-2-)amine
|
| 别名 |
E1210; APX001A; E-1210; APX 001 A; APX001A; E1210; Manogepix; E-1210; 3-(3-(4-((Pyridin-2-yloxy)methyl)benzyl)isoxazol-5-yl)pyridin-2-amine; (3-(3-(4-(((Pyridin-2-yl)oxy)methyl)benzyl)isoxazol-5-yl)pyridin-2-)amine; 7B1P18ID9L; E 1210; APX-001-A; APX001-A; Manogepix
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ~100 mg/mL (~279.03 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.08 mg/mL (5.80 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 20.8 mg/mL澄清DMSO储备液加入400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.08 mg/mL (5.80 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 20.8 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.08 mg/mL (5.80 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.7902 mL | 13.9509 mL | 27.9018 mL | |
| 5 mM | 0.5580 mL | 2.7902 mL | 5.5804 mL | |
| 10 mM | 0.2790 mL | 1.3951 mL | 2.7902 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT05491733 | Completed | Drug: APX001 Drug: APX001A |
Invasive Fungal Infections | Basilea Pharmaceutica | 2021-03-02 | Phase 1 |
| NCT04166669 | Completed | Drug: APX001 Drug: Itraconazole Drug: Rifampin |
Fungal Infection | Basilea Pharmaceutica | 2019-11-12 | Phase 1 |
| NCT04240886 | Terminated | Drug: fosmanogepix | Invasive Fungal Infections | Basilea Pharmaceutica | 2020-01-04 | Phase 2 |
| NCT05582187 | Recruiting | Drug: Fosmanogepix | Hepatic Impairment | Basilea Pharmaceutica | 2022-10-31 | Phase 1 |
|
|
|