| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 5g |
|
||
| Other Sizes |
| 体外研究 (In Vitro) |
在与中枢敏化密切相关的脊髓背角区域,盐酸布比卡因可阻断 NMDA 受体介导的突触传递 [1]。盐酸布比卡因将半最大激活/失活膜电位移向稍微更负的膜电位,这对通道激活和稳态失活的电压依赖性有影响。 SCN5A 通道对盐酸布比卡因的 IC50 为 2.18±0.16 μM,这表明在非活性状态下有轻微的敏感性[2]。盐酸布比卡因的 IC50 为 16.5 μM,剂量依赖性且可逆地抑制 SK2 通道 [3]。
|
||
|---|---|---|---|
| 体内研究 (In Vivo) |
Bupivacaine 不仅能诱导大鼠肌浆网 (SR) 释放 Ca2+,还能抑制 SR 对 Ca2+ 的摄取,这主要受 SR Ca2+ 三磷酸腺苷酶活性的调节。
|
||
| 细胞实验 |
细胞活力测定[3]
细胞类型:转染SK2基因的HEK 293细胞(转染细胞命名为SK2细胞) 测试浓度:10、 100, 1000 µM 孵育时间: 实验结果: IC50 值为 16.5 µM。 |
||
| 动物实验 |
|
||
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Systemic absorption of local anesthetics is dose- and concentration-dependendent on the total drug administered. Other factors that affect the rate of systemic absorption include the route of administration, blood flow at the administration site, and the presence or absence of epinephrine in the anesthetic solution. Bupivacaine formulated for instillation with [meloxicam] produced varied systemic measures following a single dose of varying strength. In patients undergoing bunionectomy, 60 mg of bupivacaine produced a Cmax of 54 ± 33 ng/mL, a median Tmax of 3 h, and an AUC∞ of 1718 ± 1211 ng\*h/mL. For a 300 mg dose used in herniorrhaphy, the corresponding values were 271 ± 147 ng/mL, 18 h, and 15,524 ± 8921 ng\*h/mL. Lastly, a 400 mg dose used in total knee arthroplasty produced values of 695 ± 411 ng/mL, 21 h, and 38,173 ± 29,400 ng\*h/mL. Only 6% of bupivacaine is excreted unchanged in the urine. After absorption into the blood, bupivacaine hydrochloride is more highly bound to plasma proteins than are any other local anesthetics; bupivacaine is reportedly 82-96% bound. Bupivacaine hydrochloride has the lowest degree of placental transmission of parenteral local anesthetics and may cause the least fetal depression. Pregnant rats received an intravenous infusion of bupivacaine at a rate of 0.33 mg. kg-1. min-1 over a period of 15 min. The fetuses were delivered either at the end of infusion or at 2 or 4 hr after dosing. Maternal and fetal blood and tissue samples were obtained for the assays of bupivacaine and its metabolites using capillary gas chromatography-mass spectrometry. The elimination half-life of bupivacaine was 37.7 min. The major metabolite was 3'-hydroxybupivacaine. Bupivacaine and 3'-hydroxybupivacaine were present in all samples at the end of administration. The fetal to maternal concentration ratio of bupivacaine in plasma was 0.29, and in the placenta was 0.63. The amnion contained the highest bupivacaine concentration: threefold higher in the maternal and 11-fold higher than in the fetal plasma. At 4 hr after dosing, bupivacaine was no longer detectable in any maternal and fetal samples, whereas 3'-hydroxybupivacaine was still present in all tissues except the fetal plasma and heart. These data indicate that a considerable amount of bupivacaine is taken up by both sides of the placenta, as well as the amnion and myometrium. 3'-Hydroxybupivacaine was present in all tissues except the fetal plasma and heart samples, even after the parent compound became no longer detectable. After injection of Bupivacaine Hydrochloride for caudal, epidural, or peripheral nerve block in man, peak levels of bupivacaine in the blood are reached in 30 to 45 minutes, followed by a decline to insignificant levels during the next three to six hours. Pharmacokinetic studies on the plasma profile of Bupivacaine Hydrochloride after direct intravenous injection suggest a three-compartment open model. The first compartment is represented by the rapid intravascular distribution of the drug. The second compartment represents the equilibration of the drug throughout the highly perfused organs such as the brain, myocardium, lungs, kidneys, and liver. The third compartment represents an equilibration of the drug with poorly perfused tissues, such as muscle and fat. The elimination of drug from tissue distribution depends largely upon the ability of binding sites in the circulation to carry it to the liver where it is metabolized. For more Absorption, Distribution and Excretion (Complete) data for Bupivacaine (6 total), please visit the HSDB record page. Metabolism / Metabolites Amide-type local anesthetics such as bupivacaine are metabolized primarily in the liver via conjugation with glucuronic acid. The major metabolite of bupivacaine is 2,6-pipecoloxylidine, which is mainly catalyzed via cytochrome P450 3A4. Pregnant rats received an intravenous infusion of bupivacaine at a rate of 0.33 mg. kg-1. min-1 over a period of 15 min. The fetuses were delivered either at the end of infusion or at 2 or 4 hr after dosing. Maternal and fetal blood and tissue samples were obtained for the assays of bupivacaine and its metabolites using capillary gas chromatography-mass spectrometry. The elimination half-life of bupivacaine was 37.7 min. The major metabolite was 3'-hydroxybupivacaine. Bupivacaine and 3'-hydroxybupivacaine were present in all samples at the end of administration. The fetal to maternal concentration ratio of bupivacaine in plasma was 0.29, and in the placenta was 0.63. The amnion contained the highest bupivacaine concentration: threefold higher in the maternal and 11-fold higher than in the fetal plasma. At 4 hr after dosing, bupivacaine was no longer detectable in any maternal and fetal samples, whereas 3'-hydroxybupivacaine was still present in all tissues except the fetal plasma and heart. These data indicate that a considerable amount of bupivacaine is taken up by both sides of the placenta, as well as the amnion and myometrium. 3'-Hydroxybupivacaine was present in all tissues except the fetal plasma and heart samples, even after the parent compound became no longer detectable. Bupivacaine hydrochloride is principally metabolized to pipecolylxylidine (PPX) by N-dealkylation, probably in the liver. Bupivacaine is excreted in urine as small amounts of PPX, unchanged drug (5%), and other metabolites as yet unidentified. Amide-type local anesthetics such as bupivacaine are metabolized primarily in the liver via conjugation with glucuronic acid. The major metabolite of bupivacaine is 2,6-pipecoloxylidine, which is mainly catalyzed via cytochrome P450 3A4. Route of Elimination: Only 6% of bupivacaine is excreted unchanged in the urine. Half Life: 2.7 hours in adults and 8.1 hours in neonates Biological Half-Life 2.7 hours in adults and 8.1 hours in neonates. Bupivacaine applied together with [meloxicam] for postsurgical analgesia had a median half-life of 15-17 hours, depending on dose and application site. Pregnant rats received an intravenous infusion of bupivacaine at a rate of 0.33 mg. kg-1. min-1 over a period of 15 min. The fetuses were delivered either at the end of infusion or at 2 or 4 hr after dosing. Maternal and fetal blood and tissue samples were obtained for the assays of bupivacaine and its metabolites using capillary gas chromatography-mass spectrometry. The elimination half-life of bupivacaine was 37.7 min. The elimination half-life of bupivacaine hydrochloride is 1.5-5.5 hours in adults and 8.1 hours in neonates. |
||
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
Bupivacaine is a cholinesterase or acetylcholinesterase (AChE) inhibitor. A cholinesterase inhibitor (or 'anticholinesterase') suppresses the action of acetylcholinesterase. Because of its essential function, chemicals that interfere with the action of acetylcholinesterase are potent neurotoxins, causing excessive salivation and eye-watering in low doses, followed by muscle spasms and ultimately death. Nerve gases and many substances used in insecticides have been shown to act by binding a serine in the active site of acetylcholine esterase, inhibiting the enzyme completely. Acetylcholine esterase breaks down the neurotransmitter acetylcholine, which is released at nerve and muscle junctions, in order to allow the muscle or organ to relax. The result of acetylcholine esterase inhibition is that acetylcholine builds up and continues to act so that any nerve impulses are continually transmitted and muscle contractions do not stop. Among the most common acetylcholinesterase inhibitors are phosphorus-based compounds, which are designed to bind to the active site of the enzyme. The structural requirements are a phosphorus atom bearing two lipophilic groups, a leaving group (such as a halide or thiocyanate), and a terminal oxygen. Toxicity Data The mean seizure dosage of bupivacaine in rhesus monkeys was found to be 4.4 mg/kg with mean arterial plasma concentration of 4.5 mcg/mL. LD50: 6 to 8 mg/kg (intravenous, mice) LD50: 38 to 54 mg/kg (subcutaneous, mice) Interactions Solutions of Bupivacaine Hydrochloride containing a vasoconstrictor, such as epinephrine, should be used with extreme caution in patients receiving monoamine oxidase inhibitors (MAOI) or antidepressants of the triptyline or imipramine types, because severe prolonged hypertension may result. Bupivacaine Hydrochloride with epinephrine 1:200,000 or other vasopressors should not be used concomitantly with ergot-type oxytocic drugs, because a severe persistent hypertension may occur. Non-Human Toxicity Values LD50 Mouse sc 38-54 mg/kg LD50 Mouse iv 6-8 mg/kg |
||
| 参考文献 |
|
||
| 其他信息 |
Therapeutic Uses
Bupivacaine hydrochloride is used for infiltration anesthesia and for peripheral, sympathetic nerve, and epidural (including caudal) block anesthesia. A 0.75% solution of the drug in 8.25% dextrose is used for spinal anesthesia. Bupivacaine is not used for obstetric paracervical block or topical anesthesia. /Use Included in US product label/ Bupivacaine Hydrochloride is indicated for the production of local or regional anesthesia or analgesia for surgery, dental and oral surgery procedures, diagnostic and therapeutic procedures, and for obstetrical procedures. Only the 0.25% and 0.5% concentrations are indicated for obstetrical anesthesia. /Use Included in US product label/ Drug Warnings The 0.75% solution of bupivacaine hydrochloride is no longer recommended for obstetric anesthesia, since use of this concentration for epidural anesthesia in obstetric patients has been associated with cardiac arrest with difficult resuscitation or death. Cardiac arrest has occurred after seizures resulting from systemic toxicity, apparently following inadvertent intravascular injection. Local anesthetics should only be employed by clinicians who are well versed in diagnosis and management of dose-related toxicity and other acute emergencies which might arise from the block to be employed, and then only after insuring the immediate availability of oxygen, other resuscitative drugs, cardiopulmonary resuscitative equipment, and the personnel resources needed for proper management of toxic reactions and related emergencies. delay in proper management of dose-related toxicity, under ventilation from any cause, and/or altered sensitivity may lead to the development of acidosis, cardiac arrest and, possibly, death. /Local anesthetics/ Pending accumulation of further data on the use of the drug in pediatric patients, bupivacaine hydrochloride solutions should not be used in children younger than 12 years of age and the solution for spinal anesthesia should not be used in children younger than 18 years of age. Some commercially available formulations of bupivacaine hydrochloride contain sodium metabisulfite, a sulfite that may cause allergic-type reactions, including anaphylaxis and life-threatening or less severe asthmatic episodes, in certain susceptible individuals. The overall prevalence of sulfite sensitivity in the general population is unknown but probably low; such sensitivity appears to occur more frequently in asthmatic than in nonasthmatic individuals. For more Drug Warnings (Complete) data for Bupivacaine (18 total), please visit the HSDB record page. Pharmacodynamics Bupivacaine is a widely used local anesthetic agent. Bupivacaine is often administered by spinal injection prior to total hip arthroplasty. It is also commonly injected into surgical wound sites to reduce pain for up to 20 hours after surgery. In comparison to other local anesthetics it has a long duration of action. It is also the most toxic to the heart when administered in large doses. This problem has led to the use of other long-acting local anaesthetics:ropivacaine and levobupivacaine. Levobupivacaine is a derivative, specifically an enantiomer, of bupivacaine. Systemic absorption of local anesthetics produces effects on the cardiovascular and central nervous systems. At blood concentrations achieved with therapeutic doses, changes in cardiac conduction, excitability, refractoriness, contractility, and peripheral vascular resistance are minimal. However, toxic blood concentrations depress cardiac conduction and excitability, which may lead to atrioventricular block, ventricular arrhythmias and to cardiac arrest, sometimes resulting in fatalities. In addition, myocardial contractility is depressed and peripheral vasodilation occurs, leading to decreased cardiac output and arterial blood pressure. Following systemic absorption, local anesthetics can produce central nervous system stimulation, depression or both. |
| 分子式 |
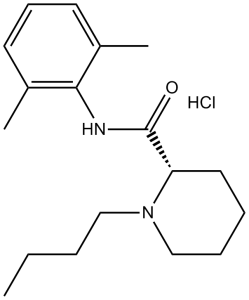
C18H28N2O.HCL
|
|
|---|---|---|
| 分子量 |
324.89
|
|
| 精确质量 |
324.196
|
|
| CAS号 |
18010-40-7
|
|
| 相关CAS号 |
Bupivacaine;38396-39-3;Bupivacaine hydrochloride monohydrate;73360-54-0
|
|
| PubChem CID |
2474
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 沸点 |
423.4ºC at 760 mmHg
|
|
| 熔点 |
107.5 to 108ºC
|
|
| 闪点 |
209.9ºC
|
|
| LogP |
4.709
|
|
| tPSA |
32.34
|
|
| 氢键供体(HBD)数目 |
1
|
|
| 氢键受体(HBA)数目 |
2
|
|
| 可旋转键数目(RBC) |
5
|
|
| 重原子数目 |
21
|
|
| 分子复杂度/Complexity |
321
|
|
| 定义原子立体中心数目 |
0
|
|
| InChi Key |
SIEYLFHKZGLBNX-UHFFFAOYSA-N
|
|
| InChi Code |
InChI=1S/C18H28N2O.ClH/c1-4-5-12-20-13-7-6-11-16(20)18(21)19-17-14(2)9-8-10-15(17)3;/h8-10,16H,4-7,11-13H2,1-3H3,(H,19,21);1H
|
|
| 化学名 |
1-butyl-N-(2,6-dimethylphenyl)piperidine-2-carboxamide hydrochloride
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中(例如氮气保护),避免吸湿/受潮和光照。 |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (7.69 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (7.69 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL 澄清 DMSO 储备液加入到 900 μL 玉米油中并混合均匀。 View More
配方 3 中的溶解度: 13 mg/mL (40.01 mM) in PBS (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶. 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 3.0780 mL | 15.3898 mL | 30.7796 mL | |
| 5 mM | 0.6156 mL | 3.0780 mL | 6.1559 mL | |
| 10 mM | 0.3078 mL | 1.5390 mL | 3.0780 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Liposomal Bupivacaine Vs Bupivacaine with Dexmedetomidine in Erector Spinae Plane Blocks for Mastectomies
CTID: NCT06252662
Phase: Phase 4 Status: Recruiting
Date: 2024-11-19