| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 2mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| Other Sizes |
|
| 靶点 |
Cardiac Late Sodium Current (INa,L) (IC50 = 0.3 μM, hiPSC-CMs voltage-clamp assay for INa,L inhibition; IC50 for peak sodium current (INa,peak) = 32 μM, hiPSC-CMs), indicating >100-fold selectivity for INa,L over INa,peak [3]
Sodium Channel (Nav1.5, cardiac isoform) [2][3] |
|---|---|
| 体外研究 (In Vitro) |
eclazine 的 IC50 为 2.5 μM,可抑制 hiPSC 来源的心肌细胞中的钠电流[3]。
1. 抑制hiPSC-CMs中的晚期钠电流(INa,L):Eleclazine HCl以剂量依赖性方式抑制人诱导多能干细胞衍生心肌细胞(hiPSC-CMs)中的INa,L,IC50=0.3 μM,对峰值钠电流(INa,peak)影响极小(IC50=32 μM),对INa,L的选择性>100倍。1 μM剂量下,INa,L降低85%,而INa,peak无显著抑制(降低<10%)(全细胞膜片钳技术)[3] 2. 兔离体心脏的抗心律失常作用:Eleclazine HCl(0.1、0.3、1.0 μM)剂量依赖性抑制哇巴因诱导的兔离体心脏室性心律失常。1.0 μM剂量下,8/8只心脏完全避免室性心动过速(VT)和室颤(VF)发生,而溶媒组仅2/8只;同时使动作电位时程(APD90)缩短15%-20%,且不延长QT间期[2] 3. 抑制INa,L的效果优于氟卡尼:在hiPSC-CMs中,1 μM Eleclazine HCl可抑制85%的INa,L,而10 μM氟卡尼仅抑制40%,显示更强的INa,L抑制效力。与氟卡尼不同,Eleclazine HCl在兔离体心脏中未显著减慢传导速度(通过ECG间期检测评估)[2][3] 4. 减少心肌细胞钙超载:Eleclazine HCl(0.3 μM)在氧化应激(H2O2处理)条件下,使hiPSC-CMs的细胞内钙瞬变(Ca2+ i)降低35%,预防钙超载诱导的细胞功能障碍(荧光钙指示剂实验)[3] |
| 体内研究 (In Vivo) |
Eleclazine(0.3 和 0.9 mg/kg;静脉注射;输注超过 15 分钟)可缩短心房 PTa 和心室 QT 间期,并降低肾上腺素引起的室性早搏和双联频率[1]。
1. 抑制猪模型中儿茶酚胺诱导的室性心动过速(VT)和T波交替:麻醉猪静脉注射Eleclazine HCl(0.3、1.0 mg/kg)或氟卡尼(2 mg/kg),30分钟后输注异丙肾上腺素(0.4 μg/kg/min)+肾上腺素(0.2 μg/kg/min)诱导VT。Eleclazine HCl剂量依赖性抑制VT:0.3 mg/kg组VT发作减少55%,1.0 mg/kg组减少90%,且所有动物的T波交替(心律失常风险预测指标)完全消失;而氟卡尼仅减少30% VT发作,且无法消除T波交替。Eleclazine HCl对平均动脉压和心率无显著影响,氟卡尼则使QRS间期延长25%[1] |
| 酶活实验 |
1. hiPSC-CMs晚期钠电流(INa,L)记录实验:人诱导多能干细胞衍生心肌细胞(hiPSC-CMs)接种于盖玻片,成熟培养30-45天。37℃下采用膜片钳放大器进行全细胞膜片钳记录,电极内液为氯化铯基缓冲液,细胞外液为氯化钠基缓冲液。Eleclazine HCl(0.01-100 μM)加入细胞外液,通过电压 protocol 诱发INa,L:从-80 mV静息电位去极化至-20 mV持续50 ms,随后复极化至-40 mV持续500 ms。INa,peak在初始去极化阶段记录,INa,L在复极化阶段记录为持续电流。电流振幅按细胞电容标准化,通过剂量-反应曲线推导IC50值[3]
2. 兔心室肌细胞钠电流实验:酶解法分离兔心室肌细胞,维持在生理缓冲液中。采用全细胞膜片钳技术记录Eleclazine HCl(0.1-10 μM)存在下的INa,L和INa,peak,电压 protocol 与hiPSC-CMs实验一致,通过INa,peak与INa,L的IC50比值计算选择性[2] |
| 细胞实验 |
1. hiPSC-CMs钙瞬变实验:成熟hiPSC-CMs用荧光钙指示剂负载30分钟(37℃),经Eleclazine HCl(0.1-3 μM)处理1小时后,暴露于100 μM H2O2诱导氧化应激。荧光显微镜记录钙瞬变,定量峰值荧光强度和衰减时间以评估细胞内钙处理功能[3]
2. hiPSC-CMs活力实验:hiPSC-CMs接种于96孔板,Eleclazine HCl(0.01-100 μM)处理24小时后,MTT法检测细胞活力,测定570 nm处吸光度。浓度高达30 μM时未观察到显著细胞毒性[3] |
| 动物实验 |
Animal/Disease Models: Male Yorkshire pigs (35.20 ± 0.46 kg; injected with epinephrine via a jugular vein)[1]
Doses: 0.3 and 0.9 mg/kg Route of Administration: IV; infused over 15 minutes Experimental Results: decreased the incidence of epinephrine-induced ventricular premature beats and couplets by 51% (from 31.3 shortened ventricular QT and atrial PTa intervals by 7%, and decreased atrial repolarization alternans and heterogeneity without attenuation of the inotropic response to catecholamine. 1. Porcine in vivo arrhythmia model: Female domestic pigs (25-30 kg) were anesthetized with isoflurane, intubated, and instrumented with ECG leads and arterial catheters for hemodynamic monitoring. After a 30-minute stabilization period, pigs were randomly divided into 3 groups (n=6/group): vehicle control (saline), Eleclazine HCl 0.3 mg/kg, Eleclazine HCl 1.0 mg/kg, or flecainide 2 mg/kg (positive control). Drugs were administered intravenously over 10 minutes. Thirty minutes after drug administration, a catecholamine challenge (isoproterenol 0.4 μg/kg/min + epinephrine 0.2 μg/kg/min) was infused for 30 minutes to induce VT. ECG was continuously recorded, and VT episodes (duration >5 seconds) and T-wave alternans were quantified. Hemodynamic parameters (mean arterial pressure, heart rate) were measured at baseline and every 15 minutes during the experiment [1] 2. Rabbit isolated heart preparation: New Zealand White rabbits (2.0-2.5 kg) were euthanized, and hearts were rapidly excised and mounted on a Langendorff perfusion system. Hearts were perfused with oxygenated Krebs-Henseleit buffer at 37℃. A pacing electrode was placed on the right atrium to maintain a heart rate of 240 beats/min. After stabilization, Eleclazine HCl (0.1, 0.3, 1.0 μM) was added to the perfusate. Ouabain (1 μM) was added to induce arrhythmias. ECG was recorded, and the incidence of VT/VF, action potential duration, and QRS interval were measured [2] |
| 毒性/毒理 (Toxicokinetics/TK) |
1. Cardiac safety profile: In porcine in vivo studies, Eleclazine HCl (0.3-1.0 mg/kg, i.v.) did not significantly prolong QRS duration or QT interval, while flecainide (2 mg/kg) increased QRS duration by 25% [1]
2. No hemodynamic toxicity: Eleclazine HCl (0.3-1.0 mg/kg, i.v.) had no significant effect on mean arterial pressure or heart rate in anesthetized pigs, indicating minimal impact on systemic hemodynamics [1] 3. Cellular toxicity: Eleclazine HCl at concentrations up to 30 μM did not reduce viability of hiPSC-CMs (MTT assay), suggesting low cytotoxicity [3] |
| 参考文献 |
|
| 其他信息 |
1. Eleclazine HCl (formerly GS-6615) is a selective inhibitor of the cardiac late sodium current (INa,L), a small inward sodium current that persists during the plateau phase of the cardiac action potential. Abnormal enhancement of INa,L leads to intracellular calcium overload, which contributes to arrhythmias, particularly in conditions of catecholamine stress [1][2][3]
2. Its mechanism of action involves blocking the late component of the cardiac sodium channel (Nav1.5), reducing intracellular sodium accumulation and subsequent calcium overload via the Na+/Ca2+ exchanger. This mechanism suppresses arrhythmic substrates such as T-wave alternans and ventricular tachycardia [1][3] 3. Eleclazine HCl exhibits superior anti-arrhythmic efficacy compared to flecainide (a class Ic anti-arrhythmic) in preclinical models, with higher selectivity for INa,L over peak sodium current, resulting in fewer conduction abnormalities (e.g., QRS prolongation) [1][2] 4. Potential therapeutic applications include the treatment of catecholamine-induced ventricular arrhythmias, such as those associated with long QT syndrome type 3 (LQT3) or myocardial ischemia. Its favorable cardiac safety profile supports further clinical development for life-threatening ventricular arrhythmias [1][3] |
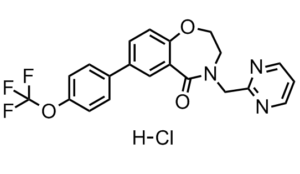
| 分子式 |
C₂₁H₁₇CLF₃N₃O₃
|
|
|---|---|---|
| 分子量 |
451.83
|
|
| 精确质量 |
451.091
|
|
| 元素分析 |
C, 55.82; H, 3.79; Cl, 7.85; F, 12.61; N, 9.30; O, 10.62
|
|
| CAS号 |
1448754-43-5
|
|
| 相关CAS号 |
1443211-72-0;1448754-43-5 (HCl);
|
|
| PubChem CID |
90479986
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| tPSA |
64.6
|
|
| 氢键供体(HBD)数目 |
1
|
|
| 氢键受体(HBA)数目 |
8
|
|
| 可旋转键数目(RBC) |
4
|
|
| 重原子数目 |
31
|
|
| 分子复杂度/Complexity |
578
|
|
| 定义原子立体中心数目 |
0
|
|
| SMILES |
Cl[H].FC(OC1C([H])=C([H])C(=C([H])C=1[H])C1C([H])=C([H])C2=C(C=1[H])C(N(C([H])([H])C1=NC([H])=C([H])C([H])=N1)C([H])([H])C([H])([H])O2)=O)(F)F
|
|
| InChi Key |
ZRYHNOXHGYUHFF-UHFFFAOYSA-N
|
|
| InChi Code |
InChI=1S/C21H16F3N3O3.ClH/c22-21(23,24)30-16-5-2-14(3-6-16)15-4-7-18-17(12-15)20(28)27(10-11-29-18)13-19-25-8-1-9-26-19;/h1-9,12H,10-11,13H2;1H
|
|
| 化学名 |
4-(pyrimidin-2-ylmethyl)-7-[4-(trifluoromethoxy)phenyl]-2,3-dihydro-1,4-benzoxazepin-5-one;hydrochloride
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.03.00
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (5.53 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (5.53 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (5.53 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.2132 mL | 11.0661 mL | 22.1322 mL | |
| 5 mM | 0.4426 mL | 2.2132 mL | 4.4264 mL | |
| 10 mM | 0.2213 mL | 1.1066 mL | 2.2132 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。