| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| Other Sizes |
|
| 靶点 |
mTOR (IC50 = 5-6 nM)
|
|---|---|
| 体外研究 (In Vitro) |
依维莫司 (RAD001) 是一种口服活性雷帕霉素衍生物,可抑制 Ser/Thr 激酶 mTOR[1]。抗增殖浓度的依维莫司导致敏感的鼠 B16/BL6 黑色素瘤 (IC50, 0.7 nM) 和不敏感的人宫颈 KB-31 (IC50, 1,778 nM) 中 S6K1 和底物 S6 完全去磷酸化以及活动性的变化4E-BP1,这表明磷酸化状态降低[3]。尽管依维莫司在不同程度上抑制了 BT474 细胞系的总细胞、干细胞和原发性乳腺癌细胞的生长。与细胞总数相比,依维莫司在所有测试浓度下抑制干细胞生长的效果较差(P<0.001)。依维莫司对 BT474 和原代 CSC 的 IC50 分别为 2,054 和 3,227 nM,分别比相应总细胞的 IC50 高 29 和 21 倍[4]。
|
| 体内研究 (In Vivo) |
依维莫司在小鼠和大鼠中均具有口服活性,产生抗肿瘤作用,其特征是肿瘤生长速率显着降低,而不是产生肿瘤消退。依维莫司(0.5 或 2.5 mg/kg)每日治疗以剂量依赖性方式抑制大鼠 CA20498 模型中的肿瘤生长,间歇性施用较高剂量 5 mg/kg(每周一次或两次)也表现出相当的抗肿瘤功效。依维莫司抑制不伴随任何体重减轻,其特点是持续抑制而不是消退[1]。依维莫司治疗(0.1-10 mg/kg/d)具有不同于 PTK/ZK 治疗(100 mg/kg)的选择性作用。当存在任一生长因子时,依维莫司会增加血红蛋白含量,血红蛋白含量是衡量血管数量及其渗漏性的指标,当转换为血液当量时。然而,依维莫司会降低 Tie-2 含量,这对 VEGF 刺激很重要,但对 bFGF 刺激则不重要。根据依维莫司在小鼠体内的药代动力学,血浆水平仅在约 4 小时内达到 1 至 3 μM,而单次给药后在人类肿瘤异种移植物中的最高水平仅为 0.1 M[3]。
|
| 酶活实验 |
FKBP12 结合测定:ELISA 式竞争测定用于无意中测量与 FK 506 结合蛋白 (FKBP12) 的结合。每个实验均使用 FK 506 作为标准,抑制活性表示为与 FK 506 相比的相对 IC50(rIC50 = IC50 依维莫司/IC50 FK 506)。使用 BALB/c 和 CBA 小鼠的脾细胞,观察免疫抑制效果RAP 及其衍生物的检测采用双向混合淋巴细胞反应 (MLR)。由于 RAP 在每个实验中用作标准,因此抑制活性表示为与 RAP 相比的相对 IC50(rIC50 = IC50 依维莫司/IC50 RAP)。
|
| 细胞实验 |
在 96 孔板中,肿瘤细胞的铺板密度为 500 至 5,000/100 μL/孔。然后以最佳细胞密度(通常每孔 1,000 至 2,000 个细胞)进行重复实验,并孵育过夜。在细胞暴露于依维莫司并孵育 4 天后,使用亚甲蓝染色对细胞进行计数。为此,向孔中注入 50 μL [20% (v/v)] 戊二醛,并在室温下静置 10 分钟。吸出培养基、用蒸馏水洗涤细胞并添加染料后,在 37°C 下孵育 100 L 亚甲基蓝 [0.05% (w/v) 水溶液] 10 分钟。
|
| 动物实验 |
Mice: Everolimus, PTK/ZK, and their respective vehicles are prepared each day just before administration to animals and the administration volume is individually adjusted based on animal body weight. Everolimus is given to C57/BL6 mice at doses ranging from 0.1 to 10 mg/kg/d orally (10 mL/kg), with 2.5 to 10 mg/kg being the most frequently used dose because it has the greatest impact. PTK/ZK is given orally at a dose of 50 to 100 mg/kg/d.
Rats: Based on body weight, Wistar-Furth rats are divided into two equal groups and given either a control dose of the drug or Everolimus (10 mg/kg/d orally in mice and 5 mg/kg three times per week orally in rats). Everolimus or vehicle is given orally by gavage (10 mL/kg) for a maximum of 7 days, with subsequent magnetic resonance measurements taken within 30 minutes of the last dose. This is done immediately after the initial measurement at baseline (day 0). |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
In patients with advanced solid tumors, peak everolimus concentrations are reached 1 to 2 hours after administration of oral doses ranging from 5 mg to 70 mg. Following single doses, Cmax is dose-proportional between 5 mg and 10 mg. At doses of 20 mg and higher, the increase in Cmax is less than dose-proportional, however AUC shows dose-proportionality over the 5 mg to 70 mg dose range. Steady-state was achieved within 2 weeks following once-daily dosing. Dose Proportionality in Patients with SEGA (subependymal giant-cell astrocytomas) and TSC (tuberous sclerosis complex): In patients with SEGA and TSC, everolimus Cmin was approximately dose-proportional within the dose range from 1.35 mg/m2 to 14.4 mg/m2. After a single dose of radiolabeled everolimus was given to transplant patients receiving cyclosporine, the majority (80%) of radioactivity was recovered from the feces and only a minor amount (5%) was excreted in urine. The blood-to-plasma ratio of everolimus is 17% to 73%. Following a 3 mg radiolabeled dose of everolimus, 80% of the radioactivity was recovered from the feces, while 5% was excreted in the urine. The blood-to-plasma ratio of everolimus is concentration dependent ranging from 17% to 73% over the range of 5 ng/mL to 5000 ng/mL. Plasma protein binding is approximately 74% in healthy subjects and in patients with moderate hepatic impairment. The apparent distribution volume associated with the terminal phase (Vz/F) from a single-dose pharmacokinetic study in maintenance kidney transplant patients is 342 to 107 L (range 128 to 589 L). The blood-to-plasma ratio of everolimus, which is concentration-dependent over the range of 5 to 5000 ng/mL, is 17% to 73%. The amount of everolimus confined to the plasma is approximately 20% at blood concentrations observed in cancer patients given Afinitor 10 mg/day. Plasma protein binding is approximately 74% both in healthy subjects and in patients with moderate hepatic impairment. After administration of Afinitor tablets in patients with advanced solid tumors, peak everolimus concentrations are reached 1 to 2 hours after administration of oral doses ranging from 5 mg to 70 mg. Following single doses, Cmax is dose-proportional with daily dosing between 5 mg and 10 mg. With single doses of 20 mg and higher, the increase in Cmax is less than dose-proportional, however AUC shows dose-proportionality over the 5 mg to 70 mg dose range. Steady-state was achieved within 2 weeks following once-daily dosing. No specific elimination studies have been undertaken in cancer patients. Following the administration of a 3 mg single dose of radiolabeled everolimus in patients who were receiving cyclosporine, 80% of the radioactivity was recovered from the feces, while 5% was excreted in the urine. The parent substance was not detected in urine or feces. The mean elimination half-life of everolimus is approximately 30 hours. For more Absorption, Distribution and Excretion (Complete) data for EVEROLIMUS (7 total), please visit the HSDB record page. Metabolism / Metabolites Everolimus is a substrate of CYP3A4 and PgP (phosphoglycolate phosphatase). Three monohydroxylated metabolites, two hydrolytic ring-opened products, and a phosphatidylcholine conjugate of everolimus were the 6 primary metabolites detected in human blood. In vitro, everolimus competitively inhibited the metabolism of CYP3A4 and was a mixed inhibitor of the CYP2D6 substrate dextromethorphan. Everolimus is a substrate of CYP3A4 and PgP. Following oral administration, everolimus is the main circulating component in human blood. Six main metabolites of everolimus have been detected in human blood, including three monohydroxylated metabolites, two hydrolytic ring-opened products, and a phosphatidylcholine conjugate of everolimus. These metabolites were also identified in animal species used in toxicity studies, and showed approximately 100-times less activity than everolimus itself. Everolimus has known human metabolites that include (1R,9S,12S,15R,16Z,18R,19R,21R,23S,24E,30S,32S,35R)-1,18-dihydroxy-12-[(2R)-1-[(1S,3R,4R)-3-hydroxy-4-(2-hydroxyethoxy)cyclohexyl]propan-2-yl]-19,30-dimethoxy-15,17,21,23,29,35-hexamethyl-11,36-dioxa-4-azatricyclo[30.3.1.04,9]hexatriaconta-16,24,26,28-tetraene-2,3,10,14,20-pentone and (1R,9S,12S,15R,16Z,18R,19R,21R,23S,24E,26E,28E,30S,32S,35R)-1,18-Dihydroxy-12-[(2R)-1-[(1S,3R,4R)-4-hydroxy-3-methoxycyclohexyl]propan-2-yl]-19,30-dimethoxy-15,17,21,23,29,35-hexamethyl-11,36-dioxa-4-azatricyclo[30.3.1.04,9]hexatriaconta-16,24,26,28-tetraene-2,3,10,14,20-pentone. Biological Half-Life ~30 hours. The mean elimination half-life of everolimus is approximately 30 hours. |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
IDENTIFICATION AND USE: Everolimus, an inhibitor of mammalian target of rapamycin (mTOR) kinase, is an antineoplastic agent and macrolide immunosuppressive agent. Everolimus (brand name Afinitor) is used in the treatment of certain types of breast cancers, neuroendocrine tumors of pancreatic origin, renal cell carcinoma, renal angiomyolipoma with tuberous sclerosis complex, and subependymal giant cell astrocytoma with tuberous sclerosis complex. Everolimus (brand name Zortress) is used for the prophylaxis of organ rejection in adult patients at low-moderate immunologic risk receiving a kidney transplant. It is also used for the prophylaxis of allograft rejection in adult patients receiving a liver transplant. HUMAN EXPOSURE AND TOXICITY: Reported experience with overdose in humans is very limited. There is a single case of an accidental ingestion of 1.5 mg everolimus in a 2-year-old child where no adverse reactions were observed. Single doses up to 25 mg have been administered to transplant patients with acceptable acute tolerability. Single doses up to 70 mg (without cyclosporine) have been given with acceptable acute tolerability. Everolimus has immunosuppressive properties and may predispose patients to bacterial, fungal, viral, or protozoal infections, including opportunistic infections. Some of these infections have been severe (e.g., resulting in respiratory or hepatic failure) or fatal. Fatal noninfectious pneumonitis also has been reported with everolimus. Increases in serum creatinine concentrations and proteinuria have been reported in clinical trials with everolimus (Afinitor). Cases of renal failure (including acute renal failure), some with a fatal outcome, also have been observed in everolimus-treated patients. ANIMAL STUDIES: Everolimus was not carcinogenic in mice or rats when administered daily by oral gavage for 2 years at doses of 0.9 mg/kg. In animal reproductive studies, oral administration of everolimus to female rats before mating and through organogenesis induced embryo-fetal toxicities, including increased resorption, pre-implantation and post-implantation loss, decreased numbers of live fetuses, malformation (e.g., sternal cleft), and retarded skeletal development. These effects occurred in the absence of maternal toxicities. Embryo-fetal toxicities in rats occurred at doses greater than or equal to 0.1 mg/kg (0.6 mg/sq m). In rabbits, embryotoxicity evident as an increase in resorptions occurred at an oral dose of 0.8 mg/kg (9.6 mg/sq m. The effect in rabbits occurred in the presence of maternal toxicities. In a pre- and post-natal development study in rats, animals were dosed from implantation through lactation. At the dose of 0.1 mg/kg (0.6 mg/sq m), there were no adverse effects on delivery and lactation or signs of maternal toxicity; however, there were reductions in body weight (up to 9% reduction from the control) and in survival of offspring (approximately 5% died or missing). There were no drug-related effects on the developmental parameters (morphological development, motor activity, learning, or fertility assessment) in the offspring. In a 13-week male fertility oral gavage study in rats, testicular morphology was affected at 0.5 mg/kg and above, and sperm motility, sperm head count and plasma testosterone concentrations were diminished at 5 mg/kg which caused a decrease in male fertility. There was evidence of reversibility of these findings in animals examined after 13 weeks post-dosing. The 0.5 mg/kg dose in male rats resulted in AUCs in the range of clinical exposures, and the 5 mg/kg dose resulted in AUCs approximately 5 times the AUCs in humans receiving 0.75 mg twice daily. Everolimus did not affect female fertility in nonclinical studies, but everolimus crossed the placenta and was toxic to the conceptus. Everolimus was not mutagenic in the bacterial reverse mutation, the mouse lymphoma thymidine kinase assay, or the chromosome aberration assay using V79 Chinese hamster cells, or in vivo following two daily doses of 500 mg/kg in the mouse micronucleus assay. Hepatotoxicity Serum enzyme elevations occur in up to a quarter of patients taking everolimus, but the abnormalities are usually mild, asymptomatic and self-limiting, rarely requiring dose modification or discontinuation. Liver test elevations above 5 times ULN occur in only 1% to 2% of treated patients. In contrast, idiosyncratic, clinically apparent acute liver injury has not been linked to everolimus therapy despite its wide scale use in several malignant and non-malignant syndromes. Elevations in serum enzymes and bilirubin and hepatitis are listed as potential adverse events in the product label for everolimun. Thus, acute clinically apparent liver injury with jaundice due to everolimus is probably quite rare, if it occurs at all. Importantly, everolimus is immunosuppressive and therapy in patients with cancer has been associated with episodes of reactivation of hepatitis B, which can be severe and even fatal. Reverse seroconversion (development of HBsAg in a person with preexisting antibody to hepatitis B, either anti-HBs or anti-HBc) has also been reported. Likelihood score: E* (unproven and also unlikely cause of clinically apparent liver injury but capable of inducing reactivation of hepatitis B). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation In two women, everolimus was either undetectable or detectable in very small amounts in the colostrum. However, no information is available on the use of everolimus during breastfeeding. An alternate drug may be preferred, especially while nursing a newborn or preterm infant. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding ~ 74% in both healthy patients and those with moderate hepatic impairment. Interactions Use of HMG-CoA reductase inhibitors such as lovastatin or simvastatin was strongly discouraged in clinical trials of everolimus with cyclosporine in renal transplant patients because of an interaction between HMG-CoA reductase inhibitors and cyclosporine. The manufacturer of Zortress recommends that patients receiving everolimus and cyclosporine therapy who are concurrently receiving an HMG-CoA reductase inhibitor and/or fibric acid derivative be monitored for the possible development of rhabdomyolysis and other adverse effects, which are described in the prescribing information for these antilipemic agents. Studies in healthy individuals indicate that there are no clinically important pharmacokinetic interactions between single-dose everolimus and atorvastatin (a CYP3A4 substrate) or pravastatin (a non-CYP3A4 substrate and P-gp substrate); HMG-CoA reductase bioactivity in plasma also was not substantially affected. Therefore, dosage adjustments are not necessary when everolimus and atorvastatin or pravastatin are used concurrently. In a population pharmacokinetic analysis, simvastatin (a CYP3A4 substrate) did not affect clearance of everolimus. The manufacturer of Zortress cautions that these results cannot be extrapolated to other HMG-CoA reductase inhibitors. Concomitant use of angiotensin-converting enzyme (ACE) inhibitors with everolimus may increase the risk of angioedema. The use of alternative antihypertensive agents should be considered in everolimus-treated patients, if necessary. If coadministration of a P-gp inhibitor is required in patients with SEGA, everolimus dosage should be reduced by approximately 50% to maintain trough everolimus concentrations of 5-10 ng/mL. If dosage reduction is required in patients receiving 2.5 mg daily, alternate-day dosing should be considered. Subsequent dosing should be individualized based on therapeutic drug monitoring. Trough everolimus concentrations should be assessed approximately 2 weeks after the addition of the P-gp inhibitor. If the P-gp inhibitor is discontinued, the everolimus dosage should be returned to the dosage used prior to initiation of the P-gp inhibitor and the trough everolimus concentration should be reassessed approximately 2 weeks later. For more Interactions (Complete) data for EVEROLIMUS (23 total), please visit the HSDB record page. |
| 参考文献 |
|
| 其他信息 |
Therapeutic Uses
Immunosuppressive Agents /CLINICAL TRIALS/ ClinicalTrials.gov is a registry and results database of publicly and privately supported clinical studies of human participants conducted around the world. The Web site is maintained by the National Library of Medicine (NLM) and the National Institutes of Health(NIH). Each ClinicalTrials.gov record presents summary information about a study protocol and includes the following: Disease or condition; Intervention (for example, the medical product, behavior, or procedure being studied); Title, description, and design of the study; Requirements for participation (eligibility criteria); Locations where the study is being conducted; Contact information for the study locations; and Links to relevant information on other health Web sites, such as NLM's MedlinePlus for patient health information and PubMed for citations and abstracts for scholarly articles in the field of medicine. Everolimus is included in the database. Afinitor is indicated for the treatment of postmenopausal women with advanced hormone receptor-positive, HER2-negative breast cancer (advanced HR+ BC) in combination with exemestane, after failure of treatment with letrozole or anastrozole. /Included in US product label/ Afinitor Tablets and Afinitor Disperz are indicated in pediatric and adult patients with tuberous sclerosis complex (TSC) for the treatment of subependymal giant cell astrocytoma (SEGA) that requires therapeutic intervention but cannot be curatively resected. /Included in US product label/c For more Therapeutic Uses (Complete) data for EVEROLIMUS (9 total), please visit the HSDB record page. Drug Warnings /BOXED WARNING/ WARNING: MALIGNANCIES AND SERIOUS INFECTIONS. Only physicians experienced in immunosuppressive therapy and management of transplant patients should prescribe Zortress. Patients receiving the drug should be managed in facilities equipped and staffed with adequate laboratory and supportive medical resources. The physician responsible for maintenance therapy should have complete information requisite for the follow-up of the patient. Increased susceptibility to infection and the possible development of malignancies such as lymphoma and skin cancer may result from immunosuppression. /BOXED WARNING/ WARNING: KIDNEY GRAFT THROMBOSIS. An increased risk of kidney arterial and venous thrombosis, resulting in graft loss, was reported, mostly within the first 30 days post-transplantation. /BOXED WARNING/ WARNING: NEPHROTOXICITY. Increased nephrotoxicity can occur with use of standard doses of cyclosporine in combination with Zortress. Therefore reduced doses of cyclosporine should be used in combination with Zortress in order to reduce renal dysfunction. It is important to monitor the cyclosporine and everolimus whole blood trough concentrations. /BOXED WARNING/ WARNING: MORTALITY IN HEART TRANSPLANTATION. Increased mortality, often associated with serious infections, within the first three months post-transplantation was observed in a clinical trial of de novo heart transplant patients receiving immunosuppressive regimens with or without induction therapy. Use in heart transplantation is not recommended. For more Drug Warnings (Complete) data for EVEROLIMUS (32 total), please visit the HSDB record page. |
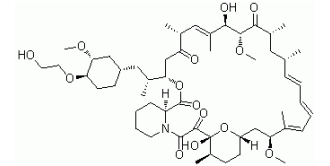
| 分子式 |
C53H83NO14
|
|---|---|
| 分子量 |
958.22
|
| 精确质量 |
957.581
|
| 元素分析 |
C, 66.43; H, 8.73; N, 1.46; O, 23.38
|
| CAS号 |
159351-69-6
|
| 相关CAS号 |
Everolimus-d4;1338452-54-2; Deprecated CAS 1245613-55-1
|
| PubChem CID |
6442177
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
1.2±0.1 g/cm3
|
| 沸点 |
998.7±75.0 °C at 760 mmHg
|
| 熔点 |
NA
|
| 闪点 |
557.8±37.1 °C
|
| 蒸汽压 |
0.0±0.6 mmHg at 25°C
|
| 折射率 |
1.548
|
| LogP |
3.35
|
| tPSA |
204.66
|
| 氢键供体(HBD)数目 |
3
|
| 氢键受体(HBA)数目 |
14
|
| 可旋转键数目(RBC) |
9
|
| 重原子数目 |
68
|
| 分子复杂度/Complexity |
1810
|
| 定义原子立体中心数目 |
15
|
| SMILES |
O=C1C([C@]2([C@@H](CC[C@@]([H])(C[C@@H](C(=CC=CC=C[C@H](C[C@H](C([C@@H]([C@@H](C(=C[C@H](C(C[C@]([H])(OC([C@]3([H])CCCCN31)=O)[C@H](C)C[C@@H]1CC[C@H]([C@@H](C1)OC)OCCO)=O)C)C)O)OC)=O)C)C)C)OC)O2)C)O)=O |t:11,13,15,23|
|
| InChi Key |
HKVAMNSJSFKALM-GKUWKFKPSA-N
|
| InChi Code |
InChI=1S/C53H83NO14/c1-32-16-12-11-13-17-33(2)44(63-8)30-40-21-19-38(7)53(62,68-40)50(59)51(60)54-23-15-14-18-41(54)52(61)67-45(35(4)28-39-20-22-43(66-25-24-55)46(29-39)64-9)31-42(56)34(3)27-37(6)48(58)49(65-10)47(57)36(5)26-32/h11-13,16-17,27,32,34-36,38-41,43-46,48-49,55,58,62H,14-15,18-26,28-31H2,1-10H3/b13-11+,16-12+,33-17+,37-27+/t32-,34-,35-,36-,38-,39+,40+,41+,43-,44+,45+,46-,48-,49+,53-/m1/s1
|
| 化学名 |
(1R,9S,12S,15R,16E,18R,19R,21R,23S,24E,26E,28E,30S,32S,35R)-1,18- dihydroxy-12-{(1R)-2-[(1S,3R,4R)-4-(2hydroxyethoxy)-3-methoxycyclohexyl]-1-methylethyl}-19,30-dimethoxy-15,17,21,23,29,35-hexamethyl-11,36-dioxa-4-aza-tricyclo[30.3.1.04,9]hexatriaconta16,24,26,28-tetraene-2,3,10,14,20-pentaone.
|
| 别名 |
SDZ-RAD; RAD-001; RAD001; RAD 001; Everolimus; Brand name Afinitor; Certican; Zortress; Xience V; Zortress; 001, RAD; 40-O-(2-hydroxyethyl)-rapamycin; 40-O-(2-Hydroxyethyl)rapamycin; Afinitor; Certican; Everolimus; RAD;
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (2.61 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: 2.5 mg/mL (2.61 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 悬浊液; 超声助溶。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (2.61 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: 2.5 mg/mL (2.61 mM) in 5% DMSO + 40% PEG300 + 5% Tween80 + 50% Saline (这些助溶剂从左到右依次添加,逐一添加), 悬浊液; 超声助溶。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 5 中的溶解度: 2.5 mg/mL (2.61 mM) in 5% DMSO + 95% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 悬浊液; 超声助溶。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 配方 6 中的溶解度: 30% Propylene glycol (dissolve first)+5% Tween 80+ddH2O: 5 mg/mL 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.0436 mL | 5.2180 mL | 10.4360 mL | |
| 5 mM | 0.2087 mL | 1.0436 mL | 2.0872 mL | |
| 10 mM | 0.1044 mL | 0.5218 mL | 1.0436 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Sotorasib Activity in Subjects With Advanced Solid Tumors With KRAS p.G12C Mutation (CodeBreak 101)
CTID: NCT04185883
Phase: Phase 1 Status: Recruiting
Date: 2024-11-29
|
 |
 |