| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| 5g |
|
||
| Other Sizes |
|
| 靶点 |
5-HT
Fluoxetine HCl (LY-110140) is a selective serotonin reuptake inhibitor (SSRI) that primarily targets the serotonin transporter (SERT). It exhibits a Ki of 0.8 nM for recombinant human SERT (using [³H]-paroxetine as the radioligand) [1] - For rat brain SERT, Fluoxetine HCl shows an IC50 of 2.1 nM in [³H]-5-HT uptake inhibition assays (rat cortical synaptosomes) [5] - It has weak affinity for 5-HT2C receptors (Ki = 350 nM, human recombinant) and no significant binding to dopamine transporters (DAT) or norepinephrine transporters (NET) at concentrations up to 1 μM [1,5] |
|---|---|
| 体外研究 (In Vitro) |
氟西汀可阻断海马细胞不可避免的休克 (IS) 引起的细胞增殖下调。氟西汀增加成年大鼠海马齿状回新生细胞的数量。氟西汀还可以增加前边缘皮质中增殖细胞的数量。氟西汀加速未成熟神经元的成熟。氟西汀增强齿状回神经发生依赖性长时程增强 (LTP)。氟西汀(但不是西酞普兰、氟伏沙明、帕罗西汀和舍曲林)会增加前额皮质中去甲肾上腺素和多巴胺的细胞外水平。急性全身给药后,氟西汀会导致去甲肾上腺素和多巴胺细胞外浓度的强劲和持续增加。细胞测定:在表达克隆的 5HT2C 受体或 5HT 受体的爪蟾细胞中,微摩尔浓度的氟西汀(百忧解)抑制血清素(5-羟色胺;5HT)引起的膜电流。对于 1 μM 5-HT 引起的反应,氟西汀的 IC50 约为 20 μM。 Fluoxetine 还抑制 [3H]5HT 与 HeLa 细胞中表达的 5HT2C 受体的结合,以及 [3H]5HT 与大鼠皮质膜中 5HT 受体的结合,Ki 分别为约 65–97 nM 和约 56 μM。服用氟西汀可阻断因不可避免的休克(IS)导致的海马细胞增殖的下调,从而导致行为绝望的状态。氟西汀增加了成年大鼠海马齿状回新生细胞的数量。氟西汀还增加了前边缘皮质中增殖细胞的数量。氟西汀加速未成熟神经元的成熟。氟西汀增强齿状回神经发生依赖性长时程增强(LTP)。氟西汀,而不是其他选择性血清素摄取抑制剂,如西酞普兰、氟伏沙明、帕罗西汀和舍曲林,可以增加前额皮质的去甲肾上腺素和多巴胺细胞外水平。急性全身给药后,氟西汀使细胞外去甲肾上腺素和多巴胺浓度强劲且持续增加。
HEK293细胞SERT介导的5-羟色胺摄取抑制:转染人SERT的HEK293细胞经盐酸氟西汀(0.1–10 nM)处理30分钟,1 nM时[³H]-5-羟色胺摄取较溶媒对照组抑制78%,IC50为0.9 nM(液体闪烁计数)[1] - 原代皮质神经元BDNF上调:体外培养7天的大鼠原代皮质神经元经盐酸氟西汀(1–10 μM)处理48小时,BDNF蛋白水平呈剂量依赖性升高。5 μM时BDNF表达增加2.4倍(Western blot),BDNF mRNA水平增加1.8倍(qPCR)[3] - 抗谷氨酸诱导的神经毒性:HT22海马细胞经盐酸氟西汀(0.5–5 μM)预处理2小时后,暴露于谷氨酸(5 mM)的细胞死亡减少。2 μM时凋亡率从45%(溶媒)降至12%(Annexin V-FITC/PI染色),caspase-3活化水平降低60%(活化型caspase-3 Western blot)[6] - 不依赖5-羟色胺受体的神经发生调节:小鼠神经干细胞(NSCs)经盐酸氟西汀(0.1–1 μM)处理72小时,增殖能力增强。0.5 μM时BrdU⁺(增殖标志物)NSCs增加35%(免疫荧光),Nestin(NSC标志物)表达无变化[6] |
| 体内研究 (In Vivo) |
氟西汀治疗还可以逆转成年雄性斯普拉格-道利大鼠暴露于不可避免的电击的动物中观察到的逃避潜伏期的缺陷。氟西汀与奥氮平联合使细胞外多巴胺 ([DA](ex)) 和去甲肾上腺素 ([NE](ex)) 水平强劲、持续增加,分别高达基线的 361% 和 272%,显着高于基线要么单独用药。
大鼠强迫游泳实验(FST)的抗抑郁样作用:雄性SD大鼠(250–300 g)口服盐酸氟西汀(5、10、20 mg/kg/天)14天。10 mg/kg/天剂量使FST中不动时间从180秒降至104秒,减少42%,对游泳或攀爬时间无影响[4] - 小鼠社交挫败模型的社交回避缓解:经10天社交挫败的C57BL/6小鼠口服盐酸氟西汀(10 mg/kg/天)21天,社交互动比(与陌生鼠相处时间/空笼时间)从0.3(溶媒)升至0.8,血浆皮质酮水平降低38%(ELISA)[2] - 慢性应激大鼠海马体积恢复:暴露于21天慢性不可预测应激(CUS)的雄性Wistar大鼠口服盐酸氟西汀(15 mg/kg/天)28天。MRI显示,CUS大鼠降低12%的海马体积恢复至正常的98%,海马BDNF蛋白水平增加2.1倍(Western blot)[3] - 小鼠高架十字迷宫(EPM)的抗焦虑作用:雌性ICR小鼠(20–25 g)在EPM测试前1小时口服盐酸氟西汀(5 mg/kg),开放臂停留时间占比从18%升至24%,增加35%[5] |
| 酶活实验 |
重组人SERT结合实验:200 μL反应体系包含50 μg转染人SERT的HEK293膜蛋白、0.5 nM [³H]-帕罗西汀(放射性配体)及盐酸氟西汀(0.01–10 nM)。25°C孵育60分钟后,通过预浸泡0.3%聚乙烯亚胺的玻璃纤维滤膜过滤,滤膜用冷50 mM Tris-HCl(pH 7.4,含120 mM NaCl和5 mM KCl)洗涤3次,液体闪烁计数仪检测放射性。非特异性结合通过加入10 μM丙咪嗪确定,采用Cheng-Prusoff方程计算Ki[1]
- 大鼠脑突触体5-羟色胺摄取实验:50 μg蛋白的大鼠皮层突触体悬浮于含0.1 nM [³H]-5-羟色胺和盐酸氟西汀(0.1–10 nM)的Krebs-Ringer-HEPES缓冲液(pH 7.4)中,37°C孵育10分钟后,加入2 mL冰浴缓冲液终止反应,玻璃纤维滤膜过滤。滤膜洗涤2次后定量放射性,非特异性摄取通过加入10 μM西酞普兰确定,从剂量-反应曲线推导IC50[5] |
| 细胞实验 |
在表达克隆的 5HT2C 受体或 5HT 受体的爪蟾细胞中,微摩尔浓度的氟西汀 (Prozac) 抑制血清素(5-羟色胺;5HT)诱导的膜电流。对于 1 μM 5-HT 引起的反应,氟西汀的 IC50 约为 20 μM。此外,[3H]5HT 与大鼠皮质膜中 5HT 受体的结合以及 [3H]5HT 与 HeLa 细胞中表达的 5HT2C 受体的结合均被氟西汀抑制,Ki 值分别约为 65-97 nM 和 56 μM。氟西汀的使用可以防止不可避免的休克(IS)引起的海马细胞增殖下调,从而导致行为绝望的状态。在成年大鼠海马齿状回中,氟西汀增加了增殖细胞的数量。氟西汀也增加了前边缘皮层的增殖细胞计数。服用氟西汀时,中性粒细胞成熟得更快。氟西汀以神经发生依赖性方式增强齿状回的 LTP。在前额皮质中,氟西汀增加去甲肾上腺素和多巴胺细胞外水平,但不增加其他选择性血清素摄取抑制剂,如西酞普兰、氟伏沙明、帕罗西汀和舍曲林。急性全身给药后,氟西汀会显着且持久地增加多巴胺和去甲肾上腺素细胞外浓度。
HEK293-SERT细胞[³H]-5-羟色胺摄取实验:稳定表达人SERT的HEK293细胞以2×10⁵细胞/孔接种于24孔板,含10% FBS的DMEM培养24小时。加入盐酸氟西汀(0.1–10 nM)37°C孵育30分钟,更换为含0.1 nM [³H]-5-羟色胺的缓冲液继续孵育15分钟。冷缓冲液洗涤细胞3次,0.1 M NaOH裂解细胞,检测放射性,相对于溶媒对照组计算摄取抑制率[1] - 原代皮质神经元BDNF Western blot:从E18大鼠胚胎分离原代皮质神经元,含B27的神经基础培养基培养7天。加入盐酸氟西汀(1–10 μM)处理48小时,含蛋白酶抑制剂的RIPA缓冲液裂解细胞,30 μg蛋白经12% SDS-PAGE电泳后转移至PVDF膜,一抗孵育BDNF和β-肌动蛋白,HRP标记二抗结合后ECL显色,ImageJ定量条带灰度[3] - HT22细胞凋亡实验:HT22细胞以1×10⁶细胞/孔接种于6孔板,含10% FBS的DMEM培养。盐酸氟西汀(0.5–5 μM)预处理2小时后加入谷氨酸(5 mM),24小时后收集细胞,Annexin V-FITC和PI室温染色15分钟,流式细胞术分析,凋亡率以Annexin V阳性细胞百分比计算[6] - 神经干细胞增殖实验:从P0小鼠脑室下区(SVZ)分离神经干细胞(NSCs),在NSC培养基(DMEM/F12+EGF+bFGF)中培养。加入盐酸氟西汀(0.1–1 μM)处理72小时,最后24小时加入BrdU(10 μM)。4%多聚甲醛固定细胞,抗BrdU(FITC标记)和抗Nestin(Cy3标记)抗体染色,荧光显微镜计数BrdU⁺Nestin⁺细胞[6] |
| 动物实验 |
Male Sprague-Dawley rats, weighing between 250 and 300 grams, are kept in housing with a 12-hour light/dark cycle (lights on at 7:00 am and lights off at 7:00 pm), constant humidity, and unrestricted access to food and water. For long-term medication therapy, rats receive intraperitoneal (IP) injections of fluoxetine (5 mg/kg/day) or saline, along with olanzapine or vehicle in their drinking water for 21 days (vehicle-treated control, fluoxetine, and olanzapine alone, as well as fluoxetine plus olanzapine). Olanzapine is the drug of choice for combination therapy because fluoxetine has the ability to disrupt olanzapine's metabolism and increase blood levels of the drug by up to 4-6 times. Olanzapine is dissolved in hydrochloric acid (HCl), and the stock solution with a concentration of 3 mg/mL is made by adjusting the pH back to 6 with 1 N sodium hydroxide. For the control animals, the same volume of vehicle solution is added to the water. Three times a week, the amount of fluid consumed is measured, and drinking bottles are refilled with pharmaceutical solution. The amount of fluid consumed by each treatment group is the same. The same dosage schedule applies to subchronic treatment, but the duration is extended to seven days.
Rat Forced Swim Test (FST): Male Sprague-Dawley rats (8–10 weeks old, 250–300 g) were housed under SPF conditions (22±2°C, 12-hour light/dark cycle). Rats were randomized into 4 groups (n=8/group): 1. Vehicle: Oral gavage of 0.5% carboxymethylcellulose sodium (CMC-Na, 10 mL/kg/day); 2. Fluoxetine 5 mg/kg: Oral gavage of Fluoxetine HCl (5 mg/kg/day, dissolved in 0.5% CMC-Na); 3. Fluoxetine 10 mg/kg: Oral gavage of Fluoxetine HCl (10 mg/kg/day, dissolved in 0.5% CMC-Na); 4. Fluoxetine 20 mg/kg: Oral gavage of Fluoxetine HCl (20 mg/kg/day, dissolved in 0.5% CMC-Na). Treatment lasted 14 days. On day 15, rats were placed in a cylindrical tank (50 cm tall, 20 cm diameter, 25°C water) for 6 minutes. Immobility time (floating without active movement) was recorded during the final 4 minutes [4] - Mouse Social Defeat Model: Male C57BL/6 mice (6–8 weeks old, 20–25 g) were subjected to 10 days of social defeat (5 minutes of physical interaction with an aggressive CD1 mouse, followed by 24 hours of sensory contact). Mice were then randomized into 2 groups (n=10/group): 1. Vehicle: Oral gavage of 0.5% CMC-Na (10 mL/kg/day); 2. Fluoxetine: Oral gavage of Fluoxetine HCl (10 mg/kg/day, dissolved in 0.5% CMC-Na). Treatment lasted 21 days. On day 32, social interaction was tested: mice were placed in a 3-chamber arena, and time spent in the chamber with a stranger CD1 mouse (vs. empty chamber) was recorded for 10 minutes [2] - Rat Chronic Unpredictable Stress (CUS) Model: Male Wistar rats (8 weeks old, 220–250 g) were exposed to CUS for 21 days (random stressors: food/water deprivation, cage tilt, cold water swim). Rats were then randomized into 2 groups (n=6/group): 1. CUS+Vehicle: Oral gavage of 0.5% CMC-Na (10 mL/kg/day); 2. CUS+Fluoxetine: Oral gavage of Fluoxetine HCl (15 mg/kg/day, dissolved in 0.5% CMC-Na). Treatment lasted 28 days. On day 50, rats were anesthetized with isoflurane for MRI (hippocampal volume measurement). Rats were then euthanized, and hippocampi were dissected for BDNF Western blot [3] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Fluoxetine hydrochloride appears to be well absorbed from the GI tract following oral administration. The oral bioavailability of fluoxetine in humans has not been fully elucidated to date, but at least 60-80% of an oral dose appears to be absorbed. However, the relative proportion of an oral dose reaching systemic circulation unchanged currently is not known. Limited data from animals suggest that the drug may undergo first-pass metabolism and extraction in the liver and/or lung following oral administration. In these animals (beagles), approximately 72% of an oral dose reached systemic circulation unchanged. Food appears to cause a slight decrease in the rate, but not the extent of absorption of fluoxetine in humans. Distribution of fluoxetine and its metabolites into human body tissues and fluids has not been fully characterized. Limited pharmacokinetic data obtained during long term administration of fluoxetine to animals suggest that the drug and some of its metabolites, including norfluoxetine, are widely distributed in body tissues, with highest concentrations occurring in the lungs and liver. The drug crosses the blood-brain barrier in humans and animals. In animals, fluoxetine: norfluoxetine ratios reportedly were similar in the cerebral cortex, corpus striatum, hippocampus, hypothalamus, brain stem, and cerebellum 1 hr after administration of single dose of the drug. In order to confirm embryonic/fetal exposure to fluoxetine and/or metabolites, dissection and whole-body autoradiographic techniques were utilized to determine the placental transfer and fetal distribution in 12 and 18 day pregnant Wistar rats 1, 4, 8, and 24 hr following a single oral 12.5 mg/kg dose of (14)C fluoxetine. On gestation Days 12 (organogenesis) and 18 (postorganogenesis), peak concentrations of radiocarbon occurred 4-8 hr after dose administration in the placenta, embryo/fetus, amniotic fluid, and maternal kidney, brain, and lung, and declined slightly at 24 hr postdose. Maternal lung contained the highest tissue concentration of radiocarbon at all time points. Placenta and maternal brain, kidney, and liver contained moderate levels of radioactivity, while embryonic/fetal tissue, amniotic fluid, and maternal plasma contained low levels of radioactivity. Mean fetal concentrations of radiocarbon at 4, 8, and 24 hr on gestation Day 18 were higher than mean embryonic concentrations on Day 12 of gestation. Analytical characterization of radioactivity indicated that combined fluoxetine and norfluoxetine concentrations accounted for 63-80% of the total radiocarbon concentrations in embryonic/fetal tissue. Results indicated that embryonic/fetal and maternal tissue levels of fluoxetine were greatest at early time points and declined with time, while norfluoxetine tissue levels were highest at the 24 hr time point. Whole-body autoradiographic techniques demonstrated that radioactivity associated with (14)C fluoxetine and/or its metabolites traversed the placenta and distributed throughout the 18 day fetus 4 hr following dose administration. Visual and quantitative evaluations of the autoradiograms indicated that the highest fetal concentrations of radiocarbon were associated with brain and thymus. Results from these studies indicate that fluoxetine and norfluoxetine traverse the placenta and distribute within the embryo/fetus during the periods of organogenesis and postorganogenesis and confirm embryonic/fetal exposure of parent and metabolite in previous negative rat teratology and reproductive studies. Elimination: Renal: 80% excreted in the urine (11.6% fluoxetine, 7.4% fluoxetine glucuronide, 6.8% norfluoxetine, 8.2% norfluoxetine glucuronide, >20% hippuric acid, 46% other); Biliary: Approximately 15% in the feces; In dialysis--Not dialyzable because of high protein binding and large volume of distribution. For more Absorption, Distribution and Excretion (Complete) data for FLUOXETINE HYDROCHLORIDE (6 total), please visit the HSDB record page. Metabolism / Metabolites The present study was designed to define the kinetic behavior of fluoxetine N-demethylation in human liver microsomes and to identify the isoforms of cytochrome p450 (CYP) involved in this metabolic pathway. The kinetics of Ne formation of norfluoxetine was determined in human liver microsomes from six genotyped CYP2C19 extensive metabolizers (EM). The correlation studies between the fluoxetine N-demethylase activity and various CYP enzyme activities were performed. Selective inhibitors or chemical probes of various cytochrome P-450 isoforms were also employed. The kinetics of norfluoxetine formation in all liver microsomes were fitted by a single-enzyme Michaelis-Menten equation (mean Km=32 umol/L +/- 7 umol/L). Significant correlations were found between N-demethylation of fluoxetine at both 25 umol/L and 100 umol/L and 3-hydroxylation of tolbutamide at 250 micromol/L (r1=0.821, P1=0.001; r2=0.668, P2=0.013), respectively, and S-mephenytoin 4'-hydroxylase activity (r=0.717, P=0.006) at high substrate concentration of 100 umol/L. S-mephenytoin (SMP) (a CYP2C19 substrate) at high concentration and sulfaphenazole (SUL) (a selective inhibitor of CYP2C9) substantially inhibited norfluoxetine formation. The reaction was minimally inhibited by coincubation with chemical probe, inhibitor of CYP3A4 (triacetyloleandomycin, TAO). The inhibition of fluoxetine N-demethylation at high substrate concentration (100 umol/L) was greater in PM livers than in EM livers (73 % vs 45 %, P < 0.01) when the microsomes were precoincubated with SUL plus TAO. Cytochrome p450 CYP2C9 is likely to be a major CYP isoform catalyzing fluoxetine N-demethylation in human liver microsomes at a substrate concentration close to the therapeutic level, while polymorphic CYP2C19 may play a more important role in this metabolic pathway at high substrate concentration. The exact metabolic fate of fluoxetine has not been fully elucidated. The drug appears to be metabolized extensively, probably in the liver, to norfluoxetine and several other metabolites. Norfluoxetine (desmethylfluoxetine) the principal metabolite, is formed by N-demethylation of fluoxetine, which may be under polygenic control. The potency and selectivity of norfluoxetine's serotonin-reuptake inhibiting activity appear to be similar to those of the parent drug. Both fluoxetine and norfluoxetine undergo conjugation with glucuronic acid in the liver, and limited evidence from animals suggests that both the parent drug and its principal metabolite also undergo O-dealkylation to form p-trifluoromethylphenol, which subsequently appears to be metabolized to hippuric acid. Biological Half-Life The half-life of fluoxetine reportedly is prolonged (to approximately 4-5 days) after administration of multiple versus single doses, suggesting a nonlinear pattern of drug accumulation during long-term administration. Following a single oral dose of fluoxetine in healthy adults, the elimination half-life of fluoxetine reportedly averages approximately 2-3 days (range: 1-9 days) and that of norfluoxetine averages about 7-9 days (range: 3-15 days). The mean half-life /for fluoxetine/ was 6.6 vs 2.2 days ... for patients with cirrhosis vs normal volunteers. Oral bioavailability: In male Sprague-Dawley rats, oral administration of Fluoxetine HCl (10 mg/kg) showed an oral bioavailability of 72% compared to intravenous administration (5 mg/kg) [1] - Plasma pharmacokinetics: Rats intravenously injected with Fluoxetine HCl (5 mg/kg) had a Cmax of 1.8 μg/mL, Tmax of 5 minutes, and elimination half-life (t1/2) of 16 hours. Oral administration (10 mg/kg) resulted in a Cmax of 0.9 μg/mL, Tmax of 6 hours, and t1/2 of 18 hours [1] - Tissue distribution: In mice, 2 hours after oral administration of Fluoxetine HCl (10 mg/kg), the brain/plasma concentration ratio was 0.9, with highest accumulation in the liver and kidneys (HPLC detection of fluoxetine in tissue homogenates) [2] - Plasma protein binding: Fluoxetine HCl exhibited 94% protein binding in human plasma (ultrafiltration method, plasma concentration range: 0.1–10 μg/mL) [1] |
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation The average amount of drug in breastmilk is higher with fluoxetine than with most other SSRIs and the long-acting, active metabolite, norfluoxetine, is detectable in the serum of most breastfed infants during the first 2 months postpartum and in a few thereafter. Adverse effects such as colic, fussiness, and drowsiness have been reported in some breastfed infants. Decreased infant weight gain was found in one study, but not in others. No adverse effects on development have been found in a few infants followed for up to a year. If fluoxetine is required by the mother, it is not a reason to discontinue breastfeeding. A safety scoring system finds fluoxetine use to be possible during breastfeeding, although others do not recommend its use. If the mother was taking fluoxetine during pregnancy or if other antidepressants have been ineffective, most experts recommend against changing medications during breastfeeding. Otherwise, agents with lower excretion into breastmilk may be preferred, especially while nursing a newborn or preterm infant. The breastfed infant should be monitored for behavioral side effects such as colic, agitation, irritability, poor feeding, and poor weight gain. Mothers taking an SSRI during pregnancy and postpartum may have more difficulty breastfeeding, although this might be a reflection of their disease state. These mothers may need additional breastfeeding support. Breastfed infants exposed to an SSRI during the third trimester of pregnancy have a lower risk of poor neonatal adaptation than formula-fed infants. ◉ Effects in Breastfed Infants Colic, decreased sleep, vomiting and watery stools occurred in a 6-day-old breastfed infant probably caused by maternal fluoxetine. Two other reports of colic in breastfed infants, a 1.76-month-old and a 2-month-old, were possibly caused by fluoxetine in breastmilk. The older of the two also exhibited hyperactivity. Another case of possible increased irritability in a 3-month-old was noted by a pediatrician observer, who was the infant’s father. However, the mother and the infant’s pediatrician disagreed. Occurrence of hyperglycemia and glycosuria in a 5-month-old, possibly from fluoxetine in breastmilk was reported to the Australian Adverse Drug Reaction Advisory Committee. A 3-day-old breastfed infant was difficult to arouse, ceased rooting behavior, decreased nursing, and was moaning and grunting. Although the infant had been exposed in utero and was somewhat drowsy during the first 2 days of life, symptoms became worse after the mother's milk came in on day 3. These effects were probably caused by fluoxetine in breastmilk. Possible drug-induced seizure-like activity and cyanosis occurred in a breastfed 3-week-old breastfed infant whose mother was taking fluoxetine, carbamazepine and buspirone during pregnancy and breastfeeding. One observational report of 4 infants found no apparent neurological abnormalities following exposure to fluoxetine in milk for 12 to 52 weeks. A retrospective, case-control, cohort study compared the weights of the infants of mothers who took fluoxetine during pregnancy and breastfed for at least 2 weeks postpartum to the infants of mothers who took fluoxetine during pregnancy and did not breastfeed. Compared to controls, decreased weight gain occurred among the 26 infants exposed postpartum to fluoxetine in breastmilk, although the weights were still in the normal range. A prospective study of 51 nursing women taking fluoxetine and 63 nursing women who took no fluoxetine found no effect on weight gain, but reported a greater frequency of unspecified side effects in the infants of mothers who took fluoxetine. This study's results have been reported only in abstract form, so some details are lacking. In a prospective study of 40 women who took fluoxetine throughout pregnancy, 21 breastfed their infants (extent and duration not stated). Testing of the infants at 15 to 71 months of age found no differences in cognitive, language or temperament measurements between infants who were breastfed and those who were not. In a study comparing the 31 infants of depressed mothers who took an SSRI during pregnancy for major depression with 13 infants of depressed mothers who did not take an SSRI, mental development and most motor development in both groups was normal at follow-up averaging 12.9 months. Three of the treated mothers took fluoxetine in doses averaging 23.3 mg daily for an average of 3 months while breastfeeding their infants. Psychomotor development was slightly delayed compared to controls, but the contribution of breastfeeding to abnormal development could not be determined. Platelet serotonin levels were measured in 11 mothers and their breastfed infants after 4 to 12 weeks of fluoxetine therapy. Platelets and neurons both have the same serotonin transporter, so this effect on platelet serotonin might indicate potential effects on the nervous system of some breastfed infants. Maternal fluoxetine dosages ranged from 20 to 40 mg daily. Ten of the infants were under 6 months of age and 4 were under 3 months of age at the start of therapy; 6 were exclusively breastfed. Although maternal platelet serotonin levels were decreased from 157 mcg/L to 23 mcg/L by fluoxetine therapy, average infant serotonin levels were 217 mcg/L before and 230 mcg/L after maternal therapy. These findings indicate that the amount of fluoxetine ingested by the infants was not sufficient to affect serotonin transport in platelets in most breastfed infants. However, 3 infants experienced drops in platelet serotonin of 13, 24 and 60%, respectively. The latter infant was the only one with measurable fluoxetine plasma levels as well as norfluoxetine, but the infant had no discernible adverse effects. One other infant had a delay in motor development at 24 weeks, but had normal mental development; 6 other infants were within 1 standard deviation of normal in both measures when tested between 24 and 56 weeks of age. Twenty-nine mothers who took fluoxetine in an average dosage of 34.6 mg daily for depression or anxiety starting no later than 4 weeks postpartum, breastfed their infants exclusively for 4 months and at least 50% during months 5 and 6. Their infants had 6-month weight gains that were normal according to national growth standards and mothers reported no abnormal effects in their infants. One study of side effects of SSRI antidepressants in nursing mothers found no adverse reactions that required medical attention in one infant whose mother was taking fluoxetine. No specific information on maternal fluoxetine dosage, extent of breastfeeding or infant age was reported. Eleven infants who were breastfed (extent and duration not stated) during maternal use of fluoxetine for depression (n = 5) or panic disorder (n = 6) had normal weight gain at 12 months of age that was not significantly different from a control group of infants whose mothers took no psychotropic medications. Neurologic development was also normal at 12 months of age. In 1 breastfed (extent not stated) infant aged 11 weeks whose mother was taking fluoxetine 20 mg daily, no adverse reactions were noted clinically at the time of the study. A small study compared the reaction to pain in infants of depressed mothers who had taken an SSRI during pregnancy alone or during pregnancy and nursing to a control group of unexposed infants of nondepressed mothers. Infants exposed to an SSRI either prenatally alone or prenatally and postnatally via breastmilk had blunted responses to pain compared to control infants. Seven of the 30 infants were exposed to fluoxetine. Because there was no control group of depressed, nonmedicated mothers, an effect due to maternal behavior caused by depression could not be ruled out. The authors stressed that these findings did not warrant avoiding drug treatment of depression during pregnancy or avoiding breastfeeding during SSRI treatment. An infant was born to a mother taking fluoxetine 40 mg daily, oxycodone 20 mg 3 times daily, and quetiapine 400 mg daily. The infant was breastfed 6 to 7 times daily and was receiving 120 mcg of oral morphine 3 times daily for opiate withdrawal. Upon examination at 3 months of age, the infant's weight was at the 25th percentile for age, having been at the 50th percentile at birth. The authors attributed the weight loss to opiate withdrawal. The infant's Denver developmental score was equal to his chronological age. An uncontrolled online survey compiled data on 930 mothers who nursed their infants while taking an antidepressant. Infant drug discontinuation symptoms (e.g., irritability, low body temperature, uncontrollable crying, eating and sleeping disorders) were reported in about 10% of infants. Mothers who took antidepressants only during breastfeeding were much less likely to notice symptoms of drug discontinuation in their infants than those who took the drug in pregnancy and lactation. A cohort of 247 infants exposed to an antidepressant in utero during the third trimester of pregnancy were assessed for poor neonatal adaptation (PNA). Of the 247 infants, 154 developed PNA. Infants who were exclusively given formula had about 3 times the risk of developing PNA as those who were exclusively or partially breastfed. Fifteen of the infants were exposed to fluoxetine in utero. A late preterm infant was born to a mother who took fluoxetine 60 mg daily throughout pregnancy and during exclusive breastfeeding. At 7 days of age, the infant was found to be having jerking movements, with hypertonia and hyperreflexia as well as tachypnea and compensated metabolic acidosis. The infant's Finnegan scores were the range of 7 to 10. On day 8 of life, the infant had a serum fluoxetine level of 120 mcg/L, which is similar to therapeutic adult levels. Breastfeeding was discontinued and after 5 days of formula feeding the infant's Finnegan scores had decreased to a range of 3 to 6. After 10 days of formula, most symptoms had subsided. At 3 months of age, the infant was growing and developing normally. The infant's symptoms were attributed to serotonin syndrome caused by the high levels of fluoxetine rather than to withdrawal. The reaction was probably caused by fluoxetine and breastfeeding might have contributed to maintaining the high fluoxetine levels after birth. A woman with narcolepsy took sodium oxybate 4 grams each night at 10 pm and 2 am as well as fluoxetine 20 mg and cetirizine 5 mg daily throughout pregnancy and postpartum. She breastfed her infant except for 4 hours after the 10 pm oxybate dose and 4 hours after the 2 am dose. She either pumped breastmilk or breastfed her infant just before each dose of oxybate. The infant was exclusively breastfed or breastmilk fed for 6 months when solids were introduced. The infant was evaluated at 2, 4 and 6 months with the Ages and Stages Questionnaires, which were withing the normal range as were the infant's growth and pediatrician's clinical impressions regarding the infant's growth and development. Two women were treated with fluoxetine 20 mg daily during the third trimester of pregnancy and during breastfeeding. Pediatric evaluations including neurologic assessments and brain ultrasound were conducted during the first 24 hours postpartum. Further follow-up was conducted at 6 or more months of age. Infant clinical status was comparable to unexposed infants from the same pediatric department. A woman was taking fluoxetine 40 mg daily during pregnancy and postpartum for depression. She breastfed (extent not stated) her infant. A venous cord gas taken at delivery showed a pH of 7.38. At 45 minutes postpartum, the baby developed respiratory distress syndrome with mixed respiratory and metabolic acidosis, becoming cyanosed and floppy requiring admission to the neonatal unit. Glucose was 3.4 mmol/L on admission. Abnormal movements, tremor, and extensor posturing were present initially, but resolved within hours, although irritability and poor sleep were noted subsequently. The mother discontinued breastfeeding and the infant’s symptoms improved, although the infant had low levels of fluoxetine and norfluoxetine in his blood. The infant was discharged at age 16 days of age. The authors attributed the infant’s symptoms to a serotonin syndrome caused by fluoxetine. ◉ Effects on Lactation and Breastmilk Fluoxetine has caused increased prolactin levels and galactorrhea in nonpregnant, nonnursing patients. Euprolactinemic galactorrhea has also been reported. In a study of cases of hyperprolactinemia and its symptoms (e.g., gynecomastia) reported to a French pharmacovigilance center, fluoxetine was found to have a 3.6-fold increased risk of causing hyperprolactinemia compared to other drugs. Preliminary animal and in vitro studies found that fluoxetine may have some estrogenic activity. The prolactin level in a mother with established lactation may not affect her ability to breastfeed. In a small prospective study, 8 primiparous women who were taking a serotonin reuptake inhibitor (SRI; 3 taking fluoxetine and 1 each taking citalopram, duloxetine, escitalopram, paroxetine or sertraline) were compared to 423 mothers who were not taking an SRI. Mothers taking an SRI had an onset of milk secretory activation (lactogenesis II) that was delayed by an average of 16.7 hours compared to controls (85.8 hours postpartum in the SRI-treated mothers and 69.1 h in the untreated mothers), which doubled the risk of delayed feeding behavior compared to the untreated group. However, the delay in lactogenesis II may not be clinically important, since there was no statistically significant difference between the groups in the percentage of mothers experiencing feeding difficulties after day 4 postpartum. A case control study compared the rate of predominant breastfeeding at 2 weeks postpartum in mothers who took an SSRI antidepressant throughout pregnancy and at delivery (n = 167) or an SSRI during pregnancy only (n = 117) to a control group of mothers who took no antidepressants (n = 182). Among the two groups who had taken an SSRI, 33 took citalopram, 18 took escitalopram, 63 took fluoxetine, 2 took fluvoxamine, 78 took paroxetine, and 87 took sertraline. Among the women who took an SSRI, the breastfeeding rate at 2 weeks postpartum was 27% to 33% lower than mother who did not take antidepressants, with no statistical difference in breastfeeding rates between the SSRI-exposed groups. An observational study looked at outcomes of 2859 women who took an antidepressant during the 2 years prior to pregnancy. Compared to women who did not take an antidepressant during pregnancy, mothers who took an antidepressant during all 3 trimesters of pregnancy were 37% less likely to be breastfeeding upon hospital discharge. Mothers who took an antidepressant only during the third trimester were 75% less likely to be breastfeeding at discharge. Those who took an antidepressant only during the first and second trimesters did not have a reduced likelihood of breastfeeding at discharge. The antidepressants used by the mothers were not specified. A retrospective cohort study of hospital electronic medical records from 2001 to 2008 compared women who had been dispensed an antidepressant during late gestation (n = 575; fluoxetine n = 21) to those who had a psychiatric illness but did not receive an antidepressant (n = 1552) and mothers who did not have a psychiatric diagnosis (n = 30,535). Women who received an antidepressant were 37% less likely to be breastfeeding at discharge than women without a psychiatric diagnosis, but no less likely to be breastfeeding than untreated mothers with a psychiatric diagnosis. In a study of 80,882 Norwegian mother-infant pairs from 1999 to 2008, new postpartum antidepressant use was reported by 392 women and 201 reported that they continued antidepressants from pregnancy. Compared with the unexposed comparison group, late pregnancy antidepressant use was associated with a 7% reduced likelihood of breastfeeding initiation, but with no effect on breastfeeding duration or exclusivity. Compared with the unexposed comparison group, new or restarted antidepressant use was associated with a 63% reduced likelihood of predominant, and a 51% reduced likelihood of any breastfeeding at 6 months, as well as a 2.6-fold increased risk of abrupt breastfeeding discontinuation. Specific antidepressants were not mentioned. # Toxicity/Toxicokinetics - Acute in vivo toxicity: The LD50 of Fluoxetine HCl in male ICR mice (intraperitoneal injection) was 240 mg/kg. Mice treated with doses > 180 mg/kg showed symptoms of convulsions and respiratory depression, with mortality within 24 hours [5] - Subacute toxicity: Rats orally administered Fluoxetine HCl (10, 20, 40 mg/kg/day) for 28 days showed no significant changes in body weight (<5% variation) or serum ALT/AST/BUN/creatinine levels. Histopathological examination of the liver, kidneys, and brain revealed no tissue damage [1] - Drug-drug interaction: Co-administration of Fluoxetine HCl (10 mg/kg/day, oral) and diazepam (2 mg/kg/day, oral) in rats for 14 days resulted in a 25% increase in diazepam plasma concentrations, but no enhanced sedative effects (rotarod test) [2] |
| 参考文献 | |
| 其他信息 |
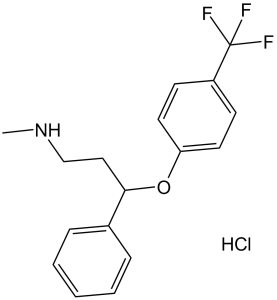
N-methyl-3-phenyl-3-[4-(trifluoromethyl)phenoxy]-1-propanamine hydrochloride (1:1) is a hydrochloride and a N-methyl-3-phenyl-3-[4-(trifluoromethyl)phenoxy]propan-1-amine.
Fluoxetine Hydrochloride is the hydrochloride salt form of fluoxetine, a diphenhydramine derivative and selective serotonin reuptake inhibitor with antidepressant, anti-anxiety, antiobsessional and antibulimic activity and with potential immunomodulating activity. Upon administration, fluoxetine binds to the presynaptic serotonin (5-HT) receptor resulting in negative allosteric modulation of the receptor complex, thereby blocking recycling of serotonin by the presynaptic receptor. Inhibition of serotonin reuptake by fluoxetine enhances serotonergic function through serotonin accumulation in the synaptic space, resulting in long-term desensitization and downregulation of 5-HT receptors, preventing 5-HT-mediated signaling and leading to antidepressant, anti-anxiety, antiobsessional and antibulimic effects. In addition, fluoxetine may inhibit the expression of pro-inflammatory cytokines, including interleukin-6 (IL-6). This may prevent IL-6-mediated inflammation and cytokine storm. The first highly specific serotonin uptake inhibitor. It is used as an antidepressant and often has a more acceptable side-effects profile than traditional antidepressants. See also: Fluoxetine (has active moiety); Fluoxetine Hydrochloride; Olanzapine (component of). Mechanism of Action The precise mechanism of antidepressant action of fluoxetine is unclear, but the drug has been shown to selectively inhibit the reuptake of serotonin (5-HT) at the presynaptic neuronal membrane. Fluoxetine-induced inhibition of serotonin reuptake causes increased synaptic concentrations of serotonin in the CNS, resulting in numerous functional changes associated with enhanced serotonergic neurotransmission. Monoamine oxidase-B has been determined to be the enzyme responsible for the conversion of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine into its toxic metabolite 1-methyl-4-phenylpyridine ion. Since this enzyme has been localized primarily in astrocytes and serotonergic neurons, it would appear that 1-methyl-4-phenylpyridine ion is being produced outside the dopaminergic neurons. To investigate this possibility, the administration of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine was preceded by systemically administered fluoxetine. In keeping with its demonstrated ability to inhibit uptake into serotonergic neurons and serotonin uptake into astrocytes, fluoxetine pretreatment resulted in a significant attenuation of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine induced depletions of striatal dopamine and serotonin concentration. These results support the extra-dopaminergic production of 1-methyl-4-phenylpyridine ion. Fluoxetine is a potent and selective inhibitor of the neuronal serotonin-uptake carrier and is a clinically effective antidepressant. Although fluoxetine is used therapeutically as the racemate, there appears to be a small but demonstrable stereospecificity associated with its interactions with the serotonin-uptake carrier. The goals of this study were to determine the absolute configurations of the enantiomers of fluoxetine and to examine whether the actions of fluoxetine in behavioral tests were enantiospecific. (S)-Fluoxetine was synthesized from (S)-(-)-3-chloro-1-phenylpropanol by sequential reaction with sodium iodide, methylamine, sodium hydride, and 4-fluorobenzotrifluoride. (S)-Fluoxetine is dextrorotatory (+1.60) in methanol, but is levorotatory (-10.85) in water. Fluoxetine enantiomers were derivatized with (R)-1-(1-naphthyl)ethyl isocyanate, and the resulting ureas were assayed by 1H NMR or HPLC to determine optical purities of the fluoxetine samples. Both enantiomers antagonized writhing in mice; following sc administration of (R)- and (S)-fluoxetine, ED50 values were 15.3 and 25.7 mg/kg, respectively. Moreover, both enantiomers potentiated a subthreshold analgesic dose (0.25 mg/kg) of morphine, and ED50 values were 3.6 and 5.7 mg/kg, respectively. Following ip administration to mice, the two stereoisomers antagonized p-chloroamphetamine-induced depletion of whole brain serotonin concentrations. ED50 values for (S)- and (R)-fluoxetine were 1.2 and 2.1 mg/kg, respectively. The two enantiomers decreased palatability-induced ingestion following ip administration to rats; (R)- and (S)-fluoxetine reduced saccharin-induced drinking with ED50 values of 6.1 and 4.9 mg/kg, respectively. Thus, in all biochemical and pharmacological studies to date, the eudismic ratio for the fluoxetine enantiomers is near unity. Mechanism of action: Fluoxetine HCl (LY-110140) exerts antidepressant effects by selectively inhibiting SERT, which blocks serotonin reuptake into presynaptic neurons, increasing extracellular serotonin levels in the brain. It also modulates neurotrophic factors (e.g., BDNF) and neurogenesis in the hippocampus, contributing to long-term therapeutic effects [1,3,6] - Therapeutic potential: Fluoxetine HCl is clinically approved for the treatment of major depressive disorder (MDD), obsessive-compulsive disorder (OCD), panic disorder, and social anxiety disorder. Preclinical models (e.g., FST, social defeat) confirm its antidepressant and anxiolytic efficacy [2,4] - Chemical properties: Fluoxetine HCl (LY-110140) is soluble in water (10 mg/mL) and DMSO (50 mg/mL). It is stable in aqueous solution (pH 4.0–8.0) for 7 days at room temperature [1] - Safety note: Literature [2] mentions that Fluoxetine HCl may increase plasma concentrations of drugs metabolized by CYP2D6 (e.g., diazepam), requiring dose adjustment in clinical practice. [2] |
| 分子式 |
C17H19CLF3NO
|
|
|---|---|---|
| 分子量 |
345.79
|
|
| 精确质量 |
345.11
|
|
| 元素分析 |
C, 59.05; H, 5.54; Cl, 10.25; F, 16.48; N, 4.05; O, 4.63
|
|
| CAS号 |
56296-78-7
|
|
| 相关CAS号 |
Fluoxetine; 54910-89-3; (S)-Fluoxetine hydrochloride; 114247-06-2; (R)-Fluoxetine hydrochloride; 114247-09-5
|
|
| PubChem CID |
62857
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 沸点 |
395.1ºC at 760mmHg
|
|
| 熔点 |
158-159°C
|
|
| 闪点 |
192.8ºC
|
|
| LogP |
5.627
|
|
| tPSA |
21.26
|
|
| 氢键供体(HBD)数目 |
2
|
|
| 氢键受体(HBA)数目 |
5
|
|
| 可旋转键数目(RBC) |
6
|
|
| 重原子数目 |
23
|
|
| 分子复杂度/Complexity |
308
|
|
| 定义原子立体中心数目 |
0
|
|
| SMILES |
Cl[H].FC(C1C([H])=C([H])C(=C([H])C=1[H])OC([H])(C1C([H])=C([H])C([H])=C([H])C=1[H])C([H])([H])C([H])([H])N([H])C([H])([H])[H])(F)F
|
|
| InChi Key |
GIYXAJPCNFJEHY-UHFFFAOYSA-N
|
|
| InChi Code |
InChI=1S/C17H18F3NO.ClH/c1-21-12-11-16(13-5-3-2-4-6-13)22-15-9-7-14(8-10-15)17(18,19)20;/h2-10,16,21H,11-12H2,1H3;1H
|
|
| 化学名 |
N-methyl-3-phenyl-3-[4-(trifluoromethyl)phenoxy]propan-1-amine;hydrochloride
|
|
| 别名 |
|
|
| HS Tariff Code |
2922.39.4500
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中(例如氮气保护),避免吸湿/受潮和光照。 |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (7.23 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (7.23 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (7.23 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: 13 mg/mL (37.60 mM) in PBS (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶. 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.8919 mL | 14.4596 mL | 28.9193 mL | |
| 5 mM | 0.5784 mL | 2.8919 mL | 5.7839 mL | |
| 10 mM | 0.2892 mL | 1.4460 mL | 2.8919 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT03826875 | Recruiting | Drug: Fluoxetine Drug: Placebo |
Stroke Hemorrhagic Depression |
University of Washington | March 1, 2019 | Phase 2 |
| NCT05634707 | Recruiting | Drug: Fluoxetine Drug: Temozolomide |
Primary Brain Tumor Brain Tumor, Recurrent |
Duke University | August 5, 2023 | Early Phase 1 |
| NCT03228732 | Recruiting | Drug: Fluoxetine Drug: Fluoxetine and DHEA |
Type 1 Diabetes Mellitus | University of Maryland, Baltimore |
December 19, 2017 | Early Phase 1 |
| NCT05976347 | Not yet recruiting | Drug: Fluoxetine 20 MG Drug: Duloxetine 30 MG/td> | Depression | Wake Forest University Health Sciences |
February 2024 | Phase 4 |
| NCT06225011 | Not yet recruiting | Drug: Fluoxetine | Colorectal Adenocarcinoma | Jonsson Comprehensive Cancer Center |
June 1, 2024 | Phase 1 |
|
|
|
|
|
|
|