| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 1mg |
|
||
| 2mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| Other Sizes |
|
| 靶点 |
IDO (IC50 = 4.52 nM)
|
|---|---|
| 体外研究 (In Vitro) |
PCC0208009 可作为一种间接 IDO1 抑制剂,因为它能抑制 HeLa 细胞中的 IDO1 活性,IC50 值为 4.52 nM,同时对体外酶活性没有影响[1]。 PCC0208009(0-200 nM;48 小时)剂量依赖性地抑制 IFN-γ 诱导的 IDO 蛋白和 mRNA 表达 [3]。
PCC-0208009/PCC对HeLa细胞存活和增殖的影响[3] 单独用IFN-γ和PCC-0208009/PCC或PCC加IFN-γ处理HeLa细胞后,检查细胞的存活率和增殖情况。存活率测定的结果如图2(a)所示;PCC和IFN-γ单独组或联合治疗组的活细胞百分比与赋形剂组相比没有显著差异(P>0.05)。增殖试验结果如图2(b)所示;PCC和IFN-γ单独或联合治疗组的IR与赋形剂组相比也没有显著差异(P > 0.05), IRs小于8%。这些结果表明,25-200nM PCC或/和100ng/mL IFN-γ对HeLa细胞的存活率和增殖没有明显影响。 PCC-0208009/PCC对HeLa细胞IDO活性和表达的影响[3] IDO在IFN-γ诱导的HeLa细胞中高度表达,广泛用于IDO抑制剂的活性筛选。用100ng/mL IFN-γ诱导10-20小时后,通过Kyn/Trp测定观察到IDO在HeLa细胞中高度表达。本研究在IFN-γ诱导24小时后检测了PCC-0208009/PCC对HeLa细胞的IDO抑制作用。如图2(c)所示,IFN-γ组IDO活性(Kyn/Trp)维持在高水平,10小时后高度表达。在PCC组中,从药物添加到至少72小时,IDO的活性被有效抑制到载体组的水平。 用IFN-γ或IFN-γ加PCC-0208009/PCC处理HeLa细胞48小时,检测IDO在蛋白质和mRNA水平的表达。蛋白质印迹分析的结果如图2(d)和(e)所示;在载体组中几乎检测不到IDO蛋白的表达水平,但经IFN-γ治疗后显著升高。PCC剂量依赖性地抑制IFN-γ诱导的IDO蛋白表达,在100和200 nM时显示出显著差异(P<0.05)。qRT-PCR的结果如图2(f)所示;载体组IDO mRNA表达水平较低,与载体组相比,IFN-γ治疗显著增加(P < 0.05). PCC可剂量依赖性地抑制IFN-γ诱导的IDO mRNA表达,与IFN-γ组相比,在所有剂量下均显示出显著差异(P < 0.05). |
| 体内研究 (In Vivo) |
在体重为 180-200 克的成年雄性 Sprague Dawley 大鼠中,给药 60、120 和 240 分钟后,在血浆和脑样本中发现了 PCC-0208009(单次口服管饲;50 毫克/千克)。给药后 60 分钟,血浆和大脑中 PCC0208009 的浓度达到最大。 Kyn/Trp 比率也在给药后 60、120 和 240 分钟同时下降,在大脑和血浆中于 60 分钟达到峰值[1]。在成年雄性 Sprague Dawley 大鼠(180 g–200 g)中,给药后 30、60 和 90 分钟检测 PCC0208009(口服灌胃;一次;12–50 mg/kg),以评估 PCC0208009 对神经性疼痛的镇痛作用 [1]。
在接受脊髓神经结扎(SNL)的大鼠中,ACC和杏仁核中的IDO1表达水平升高。PCC-0208009在福尔马林试验和SNL模型中减弱了疼痛相关行为,并在不影响运动活动和睡眠的剂量下增加了SNL大鼠的认知和焦虑行为。PCC028009通过抑制IL-6-JAK2/STAT3-ID01-GCN2-IL-6通路抑制ACC和杏仁核中IDO1的表达。此外,PCC028009通过抑制ACC和杏仁核中的NMDA2B受体和CDK5/MAP2或CDK5/Tau通路,在功能和结构水平上逆转了突触可塑性。[1] 结论和意义:这些结果支持IDO1介导的分子机制在神经性疼痛中的作用,并表明IDO1抑制剂PCC0208009具有选择性疼痛抑制作用,可能是治疗神经性疼痛的有用药物。[1] 在小鼠胶质瘤GL261异位模型中,检测了PCC-0208009对l-犬尿氨酸/色氨酸(Kyn/Trp)、肿瘤生长、肿瘤内T细胞流式细胞术以及IDO和Ki67免疫组织化学的影响。在大鼠胶质瘤C6原位模型中,检查了动物存活率、肿瘤内T细胞的流式细胞术以及增殖细胞核抗原(PCNA)和IDO的免疫组织化学。结果表明,PCC028009是一种高效的IDO抑制剂,不仅直接抑制IDO活性,而且在转录和翻译水平上参与IDO表达的基因调控。PCC028009通过增加肿瘤内CD3+、CD4+和CD8+T细胞的百分比并抑制肿瘤增殖,显著增强了替莫唑胺在GL261和C6模型中的抗肿瘤作用。这些发现表明,PCC0208009可以增强替莫唑胺的抗肿瘤疗效,并表明基于IDO抑制剂的免疫治疗与化疗的联合是治疗脑肿瘤的潜在策略。[3] PCC-0208009在福尔马林试验中的作用[1] 足底注射福尔马林(2.5%,20μL)诱导了典型的双相伤害反应,包括退缩和舔舐。PCC028009以剂量依赖的方式显著抑制了第二阶段(15分钟-45分钟)(25、50、100 mg·kg-1,图2;F(5,78)=18.10,p<0.001)。此外,60 mg·kg-1普瑞巴林组与50或100 mg·kg-1PCC-0208009组之间没有显著差异(p>0.05)。 PCC-0208009对SNL大鼠持续疼痛的影响[1] 持续疼痛是神经性疼痛的主要症状。在这里,我们测试了PCC-0208009是否可以使用CPP和开放式现场测试方法来减轻持续的疼痛,这两种方法是检测持续疼痛的两种广泛使用的方法。 在预处理阶段,所有大鼠都喜欢黑色墙壁和光滑地板的房间,各组之间没有显著差异。与赋形剂组相比,12.5、25和50 mg·kg-1 PCC028009显著增加了大鼠在药物配对室中的时间(图3A;F(5,66)=17.43,p<0.001)。此外,25和50 mg·kg-1 PCC028009在诱导CPP方面与30 mg·kg−1普瑞巴林表现出相似的效果(p>0.05)。 由于疼痛的存在会减少一般运动,我们使用开放场试验直接测量PCC-0208009是否可以恢复SNL大鼠疼痛抑制的运动。如图3所示,与假手术大鼠相比,车辆处理的SNL大鼠的运动和饲养频率较低。普瑞巴林和50 mg·kg-1 PCC028009均显著逆转了疼痛引起的低运动(图3B-C;运动,F(5,66)=2.48,p<0.05;饲养,F(5,66)=2.34,p=0.051),而所有三个剂量的PCC028009在增加运动活动和饲养行为方面与普瑞巴林(30mg·kg-1)表现出相似的程度(p>0.05)。 PCC-0208009对SNL诱导的机械和热超敏反应的影响 [1] 在单次PCC028009剂量后,对大鼠进行机械性异常性疼痛测试。SNL组术后10天内平均PWT降至2.83 g±0.76 g,与假手术组(12.09 g±0.30 g)有显著差异。12.5、25和50 mg·kg-1 PCC028009在单次给药后30、60和90分钟剂量依赖性地增加了PWT,给药后60分钟观察到峰值抗异常性疼痛作用(图3D;F(7,88)=143.53,p<0.001;普瑞巴林,F(7,88)=78.77,p<0.001;12.5 mg·kg-1 PCC028009,F(7,88)=12.00,p<0.01;25 mg·kg-1 PCC028009,F(7,88)=21.53,p<0.001;50 mg·kg-1 PCC028009,F(7,88)=42.76,p<0.001) 我们进一步测试了PCC-0208009在给药后60分钟对接受重复药物治疗的大鼠的镇痛作用。PCC028009(12.5、25、50 mg·kg−1)以剂量依赖的方式显著增加了POD17和POD24的PWT(图3F;F(5,66)=109.59,p<0.001;普瑞巴林,F(5,66)=81.36,p<0.001;12.5 mg·kg-1 PCC028009,F(5,66)=12.04,p<0.01;25 mg·kg-1 PCC028009,F(5,66)=34.96,p<0.001;50 mg·kg-1 PCC028009,F(5,66)=53.69,p<0.001)。此外,高剂量PCC0208009(50 mg·kg-1)对POD17和POD24的影响与30 mg·kg−1普瑞巴林相似(p>0.05) 在POD11上单剂量注射PCC-0208009后测试热异常性疼痛。SNL载体大鼠的PWL从10.76 s±0.56 s显著降低到6.40 s±0.45 s。PCC028009在12.5、25和50 mg·kg-1的剂量下,以剂量依赖的方式增加了给药后30、60和90 min的PWL(图3E;F(7,88)=39.91,p<0.001;普瑞巴林,F(7,88)=35.88,p<0.001;25 mg·kg-1 PCC028009,F(7,88)=23.13,p<0.05;50 mg·kg-1 PCC028009,F(7,88)=29.37,p<0.001)。 在POD18和POD25上也检查了PCC-0208009对热异常性疼痛的重复治疗。与赋形剂组相比,25和50 mg·kg-1 PCC028009均显著增加了PWL(图3G;F(5,66)=45.05,p<0.001;普瑞巴林,F(5,66)=51.82,p<0.001;12.5 mg·kg-1 PCC028009,F(5,66)=14.63,p<0.01;25 mg·kg-1 PCC028009,F(5,66)=34.24,p<0.001;50 mg·kg-1 PCC028009,F(5,66)=33.08,p<0.001)。PCC028009(50 mg·kg-1)的镇痛效果优于30 mg·kg−1普瑞巴林(p>0.05),尽管在统计学上并不显著。 PCC-0208009对SNL诱导的认知缺陷和焦虑行为的影响[1] 认知障碍和焦虑等情绪障碍是临床上慢性神经性疼痛的重要共病表现,尽管在临床前疼痛研究中很少与疼痛敏感性一起进行评估。每天用PCC-0208009治疗大鼠28天,以检查其对神经性疼痛引起的认知改变和焦虑效应的影响。 在Morris水迷宫测试中,SNL大鼠比假大鼠花更多的时间搜索平台,50 mg·kg-1 PCC-0208009阻止了这种效果(图4C;F(23216)=9.03,p<0.001)。在探针测试(POD25)期间,SNL大鼠在目标象限的时间比假大鼠少,12.5、25和50 mg·kg-1 PCC028009组防止了这种损伤(图4D;F(5,54)=5.82,p<0.001) 在EOM测试中,SNL大鼠在开放区域停留的时间比假大鼠少(图4E;F(5,66)=4.37,p<0.01),活动性也比假大白鼠低(图4F;F(5-66)=5.57,p<0.001),表明存在焦虑样表型。25和50 mg·kg-1 PCC028009显著增加了大鼠在开放区域的时间,而不会改变SNL大鼠的运动活动。 PCC-0208009对运动、镇静和翻正反射丧失的影响[1] 在旋转棒试验中,SNL大鼠在转子鼓上花费的时间和从鼓上脱落的速度显著减少。50 mg·kg-1 PCC028009显著增加了脱落前的持续时间和最大速度(图5A;F(5,66)=4.29,p<0.01;图5B;F(5,66)=4.18,p<0.01),而30 mg·kg-1普瑞巴林未能达到统计学意义(p>0.05)。 在单次给药后的开放场试验中,与对照组大鼠相比,12.5、25或50 mg·kg-1 PCC-0208009没有显著降低整体运动活性,但30 mg·kg−1普瑞巴林显著降低了大鼠的运动活性(p<0.001) 在戊巴比妥诱导的翻正反射丧失实验中,PCC028009在高达100 mg·kg-1的剂量下没有增强戊巴比妥诱导翻正反射的亚阈值剂量,因此与正常对照小鼠相比,小鼠表现出相似的睡眠潜伏期(图5E;F(5,66)=7.02,p<0.001)和睡眠持续时间(图5F;F(4,55)=27.19,p<0.001),以及进入睡眠的小鼠数量(图5D;Mann-Whitney检验,p<0.01)。相比之下,60 mg·kg-1普瑞巴林显著增加了小鼠翻正反射的丧失(p<0.001)。 PCC-0208009对SNL大鼠ACC和杏仁核IDO1酶活性的影响 与假手术组相比,SNL大鼠ACC和杏仁核中的Kyn/Trp比值显著增加,这在脊髓背角和海马中也有观察到,表明IDO1酶活性增加(图6A;脊髓背角,F(2,15)=4.84,p<0.05;海马,F(2,15)=8.21,p<0.01;ACC,F(2,15)=11.41,p<0.001;杏仁核,F(2,15)=5.05,p<0.05)。与假手术大鼠相比,SNL大鼠的Ido1 mRNA和Ido1蛋白表达也升高。PCC028009在显著降低SNL大鼠疼痛相关行为的剂量(50 mg·kg-1)下,显著降低了ACC、杏仁核、海马和脊髓背角中的Kyn/Trp比值,并显著降低了Ido1 mRNA(图6B;ACC,F(2,14)=8.41,p<0.005;杏仁核,F(2,14)=23.73,p<0.001)和蛋白质表达(图6C-D;ACC,F(2,24)=46.64;杏仁核,F(2,14)=16.45,均p<0.001)。 在NOR测试中,与假手术组相比,接受SNL手术的大鼠探索新物体的时间要少得多(图4A;F(5,66)=3.40,熟悉物体的p<0.01;F(5,66)=27.22,对于新对象,p<0.001),重复使用25或50 mg·kg-1 PCC028009可显著提高识别指数(图4B;F(5,6)=15.42,p<0.001)。 PCC-0208009对SNL大鼠ACC和杏仁核中IL-6-JAK2/STAT3-IDO-1-GCN2通路的影响[1] 由于IL-6的激活通过JAK2/STAT3途径增加IDO1的表达[8],我们研究了间接IDO1抑制剂PCC-0208009对SNL大鼠该途径的影响。 SNL手术上调了ACC和杏仁核星形胶质细胞中IDO1和GFAP的共表达(图6G),同时GFAP蛋白表达增加(图6E-F;ACC,F(2,12)=69.83;杏仁核,F(2,15)=23.21;均p<0.001)。SNL手术还显著增加了促炎细胞因子(IL-6、IL-1β)的产生及其相关受体(IL-6Rα、IL-1R1)的表达(图7A;ACC,F(2,15)=20.33;杏仁核,F(2,15)=10.61;所有p<0.001)(图7A;ACC,F(2,15)=40.12;杏仁核,F(2,15)=26.42;所有p均<0.001)(图7B-C;ACC,F(2,15)=36.89;杏仁核,F(2,15)=28.67;所有p<0.001)(图7D-E;ACC,F(2,12)=27.24;杏仁核,F(2,15)=24.21;所有p<0.001),Thr667处GCN2的磷酸化(图7F-G;ACC,F(2,15)=31.99;杏仁核,F(2,15)=55.71;所有p<0.001),Y1008时的JAK2(图7H-I;ACC,F(2,15)=26.61;杏仁核,F(2,15)=10.48;所有p<0.001)和Tyr705上的STAT3(图7J-K;ACC,F(2,15)=23.91;杏仁核,F(2,15)=38.39;均p<0.001)。50 mg·kg-1 PCC028009治疗显著减少了这些变化。 PCC-0208009对SNL大鼠突触可塑性的影响[1] 高尔基体染色用于检查ACC和杏仁核中树突和树突棘的形态变化(图8A)。树突棘总密度(图8B;ACC,F(2,72)=55.76;杏仁核,F(2,72)=37.72;所有p<0.001),蘑菇状数量(图8B;ACC,F(2,72)=28.13;杏仁核,F(2,72)=31.29;所有p<0.001)和薄状(图8B;ACC,F(2,72)=9.52;杏仁核,F(2,72)=21.76;与假手术大鼠相比,接受SNL手术的大鼠的脊柱密度显著增加,50 mg·kg-1 PCC028009治疗可以防止这些形态变化。 PCC/PCC-0208009对GL261皮下小鼠模型中Kyn/Trp的影响[3] 为了研究PCC在体内的生化机制,我们制备了携带GL261的小鼠模型。在小鼠以100mg/kg的剂量腹腔注射单剂量PCC后,在不同时间点测定了血浆和肿瘤中药效生物标志物Kyn/Trp和PCC的水平。如图3(a)所示,PCC在肿瘤和血浆中高度分布。与给药前(0小时)相比,给药后2至8小时,肿瘤和血浆样本中的Kyn/Trp比值均显著降低(P<0.05)(图3(b))。 PCC/PCC-0208009和TMZ联合治疗GL261皮下小鼠模型[3] 为了探讨PCC联合TMZ对体内肿瘤生长的抗肿瘤作用及其机制,制备了小鼠GL261皮下模型。小鼠用赋形剂、PCC、TMZ或PCC加TMZ治疗。测量动物的体重和肿瘤的体积和重量。通过流式细胞术分析肿瘤样本中的T细胞群,并用免疫组织化学方法检测IDO和Ki67的表达。 荷瘤小鼠体重[3] 如图3(c)和表1所示,与赋形剂组相比,在研究期间,PCC-0208009/PCC组对动物体重没有显著影响(P > 0.05). 从第12天和第16天到本研究结束,TMZ和PCC加TMZ组的小鼠体重与赋形剂组相比显著降低(P < 0.05). 与研究开始时相比,TMZ组和PCC加TMZ组的体重分别下降了12.56%和12.66%(P < 0.05). 然而,在PCC加TMZ组和TMZ组之间没有观察到体重下降(P > 0.05), 表明PCC不会增加TMZ的副作用。 肿瘤体积和肿瘤重量[3] 在PCC/PCC-0208009、TMZ和PCC+TMZ组中观察到肿瘤生长的抑制作用,PCC联合TMZ对肿瘤生长的影响比单独使用PCC或TMZ更强(图3(d))。研究结束时,PCC、TMZ和组合治疗组的平均肿瘤重量明显小于赋形剂组(P < 0.05), 肿瘤IR分别为42.59%、53.01%和70.83%(图3(e)和表1)。PCC组和TMZ组之间的肿瘤重量没有显著差异(P>0.05)。PCC加TMZ组的平均肿瘤重量小于PCC和TMZ两组(P < 0.05). GL261肿瘤中的T细胞亚型[3] 为了了解用PCC/PCC-0208009和TMZ治疗的动物的免疫变化,分析了肿瘤内的T细胞群。如图4(a)和(b)所示,与溶媒组相比,PCC组的CD3+、CD4+和CD8+T细胞百分比略有增加(P>0.05),而TMZ组的百分比显著降低(P<0.05)。在PCC+TMZ组中,CD3+细胞百分比显著高于溶媒组和TMZ组(P < 0.05), CD4+和CD8+的百分比高于溶媒组(P>0.05),显著高于TMZ组(P < 0.05). GL261肿瘤中IDO和Ki67的表达[3] 采用免疫组织化学检测GL261肿瘤中IDO和Ki67表达的变化。Ki67蛋白是增殖的细胞标志物。如图4(c)和(d)所示,Ki67在载体组中的表达水平很高。在PCC-0208009/PCC和TMZ组中观察到Ki67表达的显著降低(P > 0.05), 与赋形剂组相比,PCC加TMZ组的Ki67表达显著降低(P<0.05)。TMZ组和PCC组之间的Ki67的表达没有显著差异(P>0.05)。IDO的表达如图4(e)和(f)所示。载体组GL261肿瘤中观察到IDO的高表达水平,而PCC组的IDO表达显著降低(P < 0.05). PCC-0208009/PCC和TMZ联合治疗C6原位大鼠模型[3] 通过将肿瘤细胞植入SD大鼠的尾状核,制备了大鼠胶质瘤C6的同基因颅内原位模型。肿瘤接种日被指定为第1天。 动物存活率和体重[3] 动物存活曲线如图5(a)所示。与赋形剂组相比,PCC-0208009/PCC或TMZ组的动物存活率没有显著延长(P > 0.05). PCC加TMZ组的动物存活率明显延长,与赋形剂组(P<0.05)和PCC和TMZ组相比(P<0.05)。 如图5(b)所示,与赋形剂组相比,在研究期间,PCC-0208009/PCC组对大鼠体重没有显著影响(P > 0.05); 从第8天到本研究结束,从第8天至第21天,TMZ组和PCC加TMZ组的大鼠体重明显下降(P < 0.05). 然而,在PCC加TMZ组和TMZ组之间没有观察到体重的额外下降(P > 0.05), 表明PCC在该模型中没有增加TMZ的副作用。 C6肿瘤中的T细胞亚型[3] 为了了解PCC-0208009/PCC和PCC和TMZ联合治疗抗肿瘤作用的免疫机制,分析了肿瘤内的T细胞群。如图5(c)和(d)所示,与赋形剂组相比,PCC组的CD3+、CD4+和CD8+T细胞百分比增加,范围在40%至70%之间,TMZ组略有下降。在PCC+TMZ组中,CD3+、CD8+和CD4+T细胞的百分比与赋形剂和TMZ组相比显著增加了约两倍。 免疫组织化学法检测C6肿瘤中PCNA和IDO的表达[3] 免疫组织化学染色结果如图6所示。PCNA表达是胶质瘤的有用预后和诊断生物标志物。19 PCNA在脑组织中的表达非常低,在载体组的肿瘤中高度表达(图6(a))。与溶媒组相比,PCC-0208009/PCC、TMZ和PCC+TMZ组的PCNA显著降低(P < 0.05). 与PCC和TMZ组相比,PCC+TMZ组的PCNA显著降低(P < 0.05). 与赋形剂组相比,PCC组C6肿瘤中的IDO表达显著降低(P<0.05)(图6(b))。 |
| 酶活实验 |
IDO1活性测定[1]
通过LC-MS/MS系统分析脊髓和脑中Trp和Kyn的浓度。对大鼠(每组6只)实施安乐死,并在给药后解剖和收获L3-L4脊髓背角、海马、ACC和杏仁核组织,以测定IDO1活性。所有组织均用去离子水(40μL中含10mg组织)均质化,离心并收集上清液。使用PK研究中描述的方法确定每个组织中Kyn/Trp的比率。 |
| 细胞实验 |
蛋白质印迹分析[3]
细胞类型: HeLa 细胞 测试浓度: 0、50、100、200 nM 孵育时间:48小时 实验结果:PCC剂量依赖性地抑制IFN-γ诱导的IDO蛋白表达,在100和200 nM时表现出显着差异( P<0.05)。 RT-PCR [3] 细胞类型: HeLa 细胞 测试浓度: 0、50、100、200 nM 孵育持续时间:48小时 实验结果:PCC以剂量依赖性方式抑制IFN-γ的IDO mRNA表达,这在以下时间表现出显着差异:所有剂量与IFN-γ组相比。 PCC/PCC-0208009对HeLa细胞存活和增殖的影响[3] HeLa细胞以6×103个细胞/孔的速度接种到96孔板中。培养10-12小时后,用含有100 ng/mL干扰素-γ(IFN-γ)或PCC-0208009的新鲜培养基替换培养基,在25、50、100或200 nM浓度下添加或不添加100 ng/mL IFN-γ,并使用含有0.1%DMSO的培养基作为载体处理。在添加药物后72小时,观察细胞存活率和增殖情况。在存活率测定中,使用CountStar IC1000自动细胞计数器洗涤、胰蛋白酶处理和计数贴壁细胞,并通过0.1%台盼蓝排除法确认计数细胞的存活率,该排除率表示为活细胞的百分比。在增殖试验中,使用3-[4,5-二甲基噻唑-2-基]-2,5-二苯基溴化四唑(MTT)法检测细胞。对照细胞的细胞增殖率表示为100%,并计算其他组的相对细胞增殖率。 PCC/PCC-0208009对HeLa细胞IDO活性的抑制作用[3] HeLa细胞以6×103个细胞/孔的速度接种在96孔板中。培养10-12小时后,仅用新鲜培养基或含有100 ng/mL IFN-γ的培养基替换培养基。除载体组外,其他组均由IFN-γ诱导24小时。然后,仅用新鲜培养基、含有100 ng/mL IFN-γ的培养基或含有100 nMPCC-0208009的培养基替换培养基。在添加药物后0.5、1、2、5、10、24、48和72小时,收集细胞上清液,通过液相色谱-串联质谱(LC-MS/MS)测定l-犬尿氨酸(Kyn)和色氨酸(Trp)。 PCC/PCC-0208009对HeLa细胞IDO表达的影响[3] HeLa细胞以2×105个细胞/孔的速度接种在6孔板中。培养10-12h后用新鲜培养基替换培养基,分别在50、100和200 nM下为100 ng/mL IFN-γ或100 ng/mL IFN-γ加PCC-0208009。孵育48小时后,收获细胞。分别通过Western blot和定量实时聚合酶链式反应(qRT-PCR)检测IDO在蛋白质和mRNA水平的表达。 |
| 动物实验 |
Animal/Disease Models: Adult male Sprague Dawley rats (180 g-200 g) [1]
Doses: 50 mg/kg Route of Administration: Single po (oral gavage) Experimental Results: The highest concentrations of PCC-0208009 in plasma and brain were observed at 60 min after administration. Animal/Disease Models: Adult male SD (Sprague-Dawley) rats bearing spinal nerve ligation (SNL)[1] Doses: 12.5 mg/kg, 25 mg/kg, 50 mg/kg Route of Administration: po (oral gavage); once Experimental Results: demonstrated the behavioral tests and the timelines. Formalin-induced inflammatory pain model [1] Formalin test was carried out in mice according to a modified protocol in a transparent test chamber (23 cm × 13 cm × 14 cm; length × width × height). Sham (0.5% CMC-Na, p.o.), vehicle (0.5% CMC-Na, p.o.), pregabalin (60 mg·kg−1, p.o.) or PCC-0208009 (25, 50, 100 mg·kg−1, p.o.) were administered 60 min before formalin injection in a volume of 10 mL·kg−1 body weight (n = 14 mice per group) and then mice were acclimatized in the test cage for 10 min prior to formalin injection. 20 μL of 2.5% formalin (36.5–38% formaldehyde solution diluted in 0.9% saline) was injected to the right hind paw subcutaneously (s.c.) (sham mice were injected with 20 μL 0.9% saline) and pain-like nocifensive behaviors were monitored as 5 min bins for a total duration of 60 min. A mirror placed behind the observation chamber allowed the unhindered observation of the formalin-injected paw. The cumulative licking, shaking and lifting time (s) of the injected paw were counted as described. Behavioral response during 0–5 min post-formalin was considered Phase I and that during 15 min-45 min post-formalin injection was considered Phase II. Animal model of neuropathic pain [1] A model of neuropathic pain was induced by the ligation of L5 spinal nerve as described previously. Briefly, rats were anesthetized with sodium pentobarbital (50 mg·kg−1, i.p.). Thereafter, a 2 cm long incision was made at the level of the posterior iliac crest to access the right lumbar spinal nerves under the cold-light. L5 spinal nerve was identified and carefully dissected free from the adjacent L4 spinal nerve and then tightly ligated distal to the dorsal root ganglia using 6–0 silk suture. The SNL operation was completed by closing the muscles and skin with a 3–0 and 2–0 silk suture in layers. Daily intramuscular injection of 0.4 mL penicillin was administered post-surgically for three days to prevent infection. In the sham surgery, the L5 nerve was not ligated. Rats were allowed to recover for 7 days before behavioral testing. Experiment design in SNL rats [1] The timelines and experimental designs of the behavioral tests were shown in Fig. 1E. The experiments from 1 to 4 were all for SNL rats, and each group in experiments was 12 rats but were not the same animals. Experiment 1: to evaluate the antinociceptive effects of an acute dose of PCC-0208009 on neuropathic pain, six groups of rats (n = 12 per group) with the following treatments were used: sham (0.5% CMC-Na, p.o.), vehicle (0.5% CMC-Na, p.o.), pregabalin (30 mg·kg−1, p.o.) and PCC0208009 (12.5, 25 and 50 mg·kg−1, p.o.). Mechanical allodynia and thermal hyperalgesia were measured before and 30, 60 and 90 min after the drug administration on day 10 post-SNL surgery (POD10) and POD 11, respectively. Experiment 2: to measure the antinociceptive effects of PCC-0208009 on spontaneous pain, conditioned place preference (CPP) was performed during POD10 to POD17 and six groups of rats (n = 12 per group) with the following treatments were used: sham (0.5% CMC-Na, p.o.), vehicle (0.5% CMC-Na, p.o.), pregabalin (30 mg·kg−1, p.o.) and PCC0208009 (12.5, 25 and 50 mg·kg−1, p.o.). Experiment 3: to measure the effects of repeated administration of PCC-0208009 on the neuropathic pain and motor function, six groups of rats (n = 12 per group) with the following treatments were used: sham (0.5% CMC-Na, p.o.), vehicle (0.5% CMC-Na, p.o.), pregabalin (30 mg·kg−1, p.o.) and PCC0208009 (12.5, 25 and 50 mg·kg−1, p.o.). Drugs were administered p.o. twice daily for 21 consecutive days. Mechanical allodynia was measured 60 min after drug administration on POD17 and POD24, and thermal hyperalgesia was measured 60 min after drug administration on POD18 and POD25. Rota-rod and open field tests were performed 60 min after drug administration on POD26-POD28 and POD29, respectively. Besides, the ACC and amygdala tissues for immunofluorescence assay were collected on POD14. The spinal cord dorsal horn, hippocampus, ACC and amygdala tissues for IDO1 activity assay as well as the ACC and amygdala tissues for IL-6, IL-1β enzyme linked immunosorbent assay (ELISA), Golgi-cox stain, western blotting and reverse transcription-polymerase chain reaction (RT-PCR) were collected on POD30 (sham n = 6; vehicle, n = 6; PCC0208009 50 mg·kg−1, n = 6). Experiment 4: to measure the effects of repeated administration of PCC-0208009 on anxiety-like and cognition-related behaviors, seven groups of rats (n = 12 per group) with the following treatments were used: sham (0.5% CMC-Na, p.o.), vehicle (0.5% CMC-Na, p.o.), diazepam (3 mg·kg−1), risperidone (1 mg·kg−1) and PCC0208009 (12.5, 25 and 50 mg·kg−1). Drugs were administered p.o. twice daily for 19 consecutive days. Novel object recognition (NOR) test was evaluated 60 min postdose on POD14 and POD15, Morris water maze (MWM) test was performed 60 min postdose on POD21 and POD25, and elevated zero maze test (EOM) was performed 60 min postdose on POD28. Pentobarbital-induced loss of righting reflex in normal mice [1] Mice (n = 12 per group) were acclimated to the environment in a transparent test chamber (23 cm × 13 cm × 14 cm; length × width × height) for at least 2 h and randomly assigned into six groups: vehicle (0.5% CMC-Na, p.o.), diazepam (3 mg·kg−1, p.o.), pregabalin (60 mg·kg−1, p.o.) and PCC-0208009 (25, 50, 100 mg·kg−1, p.o.) before testing. Forty-five min before pentobarbital sodium (28 mg·kg−1, i.p.) injection, mice received the respective drug administrations. Immediately after pentobarbital administration, the loss of righting reflex was tested for 30 min. The number of mice with the loss of righting reflex for at least 1 min within the 30 min test period was recorded. Sleep latency was defined as the time between pentobarbital injection and the time that loss of righting reflex was observed, and sleep duration was defined as the time between the onset of loss of righting reflex and the time that mice regained righting reflex. Locomotor activity in normal rats [1] Rats (n = 12 per group) were transferred to the test room at least 2 h before the test and were randomly assigned into five groups: vehicle (0.5% CMC-Na, p.o.), pregabalin (30 mg·kg−1, p.o.) and PCC-0208009 (12.5, 25, 50 mg·kg−1, p.o.). Fifty-five minutes after the respective drug administrations, rats were placed into test boxes (50 cm × 50 cm × 50 cm; length × width × height) and the locomotor activity was recorded and analyzed for 10 min by TopScan monitoring system. Effects on the pharmacodynamic biomarker Kyn/Trp [3] When the tumor volumes reached approximately 300–400 mm3, the mice were intragastrically (i.g.) administered a single dose of PCC-0208009/PCC at 100 mg/kg. At 0, 2, 4, and 8 h after administration, plasma and tumor were collected for the detection of Trp, Kyn, and PCC, with five animals per time point. Trp, Kyn, and PCC were all measured by LC-MS/MS. Anti-tumor effects of PCC-0208009/PCC in combination with TMZ [3] When the tumors reached approximately 100 mm3, the mice were randomized into four groups: Vehicle, PCC-0208009/PCC, TMZ, and PCC plus TMZ; each group contained 10 mice. PCC was i.g. administered at 100 mg/kg twice daily, TMZ was i.g. administered at 100 mg/kg once every 2 days, and the vehicle group was i.g. administered 1% SCMC twice daily. The dosing volume was 0.1 mL/10 g. During the study, the body weight of animals and tumor volumes were measured once every 3 or 5 days. At the end of the study, tumors were collected and quickly weighed. The mean tumor weight (MTW) in each group was obtained. The inhibition rate (IR in %) was calculated by the following formula: IR (%) = [(MTWvehicle − MTWtreatment)/MTWvehicle] × 100. Five tumors were randomly selected for flow cytometry analysis, and three tumors were randomly selected for immunohistochemical detection. Animal survival study [3] According to the body weight, animals were randomly divided into four groups: Vehicle, PCC-0208009/PCC, TMZ, and PCC plus TMZ. Each group contained 10 animals. PCC was i.g. administered at 50 mg/kg twice daily, TMZ was i.g. administered at 50 mg/kg once every 2 days, and the vehicle group was i.g. administered with 1% SCMC twice daily, from day 5 to day 35. The dosing volume was 0.2 mL/100 g. During the study, the body weight was measured twice every week and the survival times of rats were recorded and analyzed. Animals were kept in the study until the rats were dead or dying. |
| 药代性质 (ADME/PK) |
The PK/PD profile of PCC-0208009 after a single oral administration in rats [1]
In order to assess the mean plasma or brain concentration-time profiles and the inhibition of IDO1 enzyme activity to produce Kyn from Trp in rats, PK/PD testing was conducted in rats. PCC0208009 was detected at 60, 120 and 240 min after drug administration in plasma and brain samples, and the highest concentrations of PCC0208009 in plasma (Fig. 1B) and brain (Fig. 1C) were observed at 60 min after administration. Concomitantly, the Kyn/Trp ratio decreased at 60, 120 and 240 min postdose, with the minimum level in the plasma and the brain seen at 60 min post-dose (Fig. 1D). Distribution of PCC-0208009/PCC in rat brain [3] At 15 days after tumor inoculation, the rats were i.g. administered a single dose of PCC-0208009/PCC at 50 mg/kg, and the cerebrum and cerebellum were harvested for the detection of PCC content. The PCC contents in the cerebrum and cerebellum were 122.3 and 113.7 nM/g at 0.5 h, 70.6 and 63.5 nM/g at 2.5 h, 32.8 and 34.3 nM/g at 6.5 h, respectively. These results indicated that PCC could cross the blood-brain barrier and distribute into the brain. Pharmacokinetic (PK) and pharmacodynamic (PD) studies [1] The PCC-0208009 concentration and the Kyn/Trp ratio in the plasma and brain of rats were measured. Healthy Sprague-Dawley rats were given a single oral dose of PCC-0208009 at 50 mg·kg−1. Plasma and brain samples were collected at 60, 120 and 240 min post-drug administration. Brain samples were homogenized in purified water (weight to volume ratio of 4:1). The concentrations of PCC0208009 in the plasma and brain were determined using a validated high-performance LC-MS/MS method, analyzed by an Agilent 1100 series HPLC system and a TSQ Quantum Access tandem mass spectrometer equipped with electrospray ionization (ESI) source. Samples (5 μL) were pretreated by a liquid–liquid extraction with 3 mL of tert-butyl methyl ether-dichloromethane (3/2, v/v). The mobile phase used acetonitrile-water (80:20, v/v) containing 0.02 mM ammonium acetate and was kept at a flow rate of 0.2 mL·min−1. A symmetry C18 column (150 mm × 2.1 mm i.d., 3.5 μm, Waters, USA, SN: 0124362291265) was used for the HPLC system. The following parameters were applied: spray voltage of 4 kV; sheath gas and auxiliary gas pressures of 30 and 5 psi, respectively; capillary temperature of 350℃; and argon gas pressure of 1.5 milli-Torr. The collision induced dissociation voltage was 18 V for all samples. The transitions (precursor to product) monitored were m/z 436.1 → 253.9. The quantities of Kyn and Trp were determined according to methods previously established in the laboratory Distribution of PCC-0208009/PCC in the rat brain [3] After tumor inoculation for 15 days, rats were i.g. administered a single dose of PCC at 50 mg/kg. At 0.5, 2.5, and 6.5 h after dosing, the cerebrum and cerebellum were harvested for detection of PCC content using LC-MS/MS. |
| 参考文献 |
|
| 其他信息 |
Background and purpose: Indoleamine 2, 3-dioxygenase 1 (IDO1) has been linked to neuropathic pain and IDO1 inhibitors have been shown to reduce pain in animals. Some studies have indicated that IDO1 expression increased after neuropathic pain in hippocampus and spinal cord, whether these changes existing in anterior cingulate cortex (ACC) and amygdala remains obscure and how IDO1 inhibition leads to analgesia is largely unknown. Here, we evaluated the antinociceptive effect of PCC0208009, an indirect IDO1 inhibitor, on neuropathic pain and examined the related neurobiological mechanisms.
Experimental approach: The effects of PCC0208009 on pain, cognition and anxiogenic behaviors were evaluated in a rat model of neuropathic pain. Motor disorder, sedation and somnolence were also assessed. Biochemical techniques were used to measure IDO1-mediated signaling changes in ACC and amygdala.
Key results: In rats receiving spinal nerve ligation (SNL), IDO1 expression level was increased in ACC and amygdala. PCC0208009 attenuated pain-related behaviors in the formalin test and SNL model and increased cognition and anxiogenic behaviors in SNL rats at doses that did not affect locomotor activity and sleeping. PCC0208009 inhibited IDO1 expression in ACC and amygdala by inhibiting the IL-6-JAK2/STAT3-IDO1-GCN2-IL-6 pathway. In addition, PCC0208009 reversed synaptic plasticity at the functional and structural levels by suppressing NMDA2B receptor and CDK5/MAP2 or CDK5/Tau pathway in ACC and amygdala.
Conclusion and implications: These results support the role of IDO1-mediated molecular mechanisms in neuropathic pain and suggest that the IDO1 inhibitor PCC0208009 demonstrates selective pain suppression and could be a useful pharmacological therapy for neuropathic pain. [1]
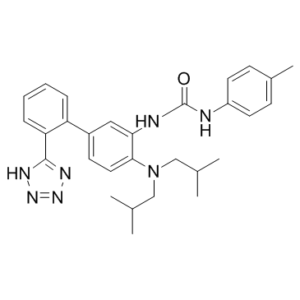
A novel series of o-phenylenediamine-based inhibitors of indoleamine 2,3-dioxygenase (IDO) has been identified. IDO is a heme-containing enzyme, overexpressed in the tumor microenvironment of many cancers, which can contribute to the suppression of the host immune system. Synthetic modifications to a previously described diarylether series resulted in an additional degree of molecular diversity which was exploited to afford compounds that demonstrated significant potency in the HeLa human cervical cancer IDO1 assay. [2] Indoleamine 2,3-dioxygenase (IDO), which is highly expressed in human glioblastoma and involved in tumor immune escape and resistance to chemotherapy, is clinically correlated with tumor progression and poor clinical outcomes, and is a promising therapeutic target for glioblastoma. IDO inhibitors are marginally efficacious as single-agents; therefore, combination with other therapies holds promise for cancer therapy. The aim of this study was to investigate the anti-tumor effects and mechanisms of the IDO inhibitor PCC0208009 in combination with temozolomide. The effects of PCC0208009 on IDO activity inhibition, and mRNA and protein expression in HeLa cells were observed. In the mouse glioma GL261 heterotopic model, the effects of PCC0208009 on l-kynurenine/tryptophan (Kyn/Trp), tumor growth, flow cytometry for T cells within tumors, and immunohistochemistry for IDO and Ki67 were examined. In the rat glioma C6 orthotopic model, animal survival, flow cytometry for T cells within tumors, and immunohistochemistry for proliferating cell nuclear antigen (PCNA) and IDO were examined. The results show that PCC0208009 is a highly effective IDO inhibitor, not only directly inhibiting IDO activity but also participating in the gene regulation of IDO expression at the transcription and translation levels. PCC0208009 significantly enhanced the anti-tumor effects of temozolomide in GL261 and C6 models, by increasing the percentages of CD3+, CD4+, and CD8+ T cells within tumors and suppressing tumor proliferation. These findings indicate that PCC0208009 can potentiate the anti-tumor efficacy of temozolomide and suggest that combination of IDO inhibitor-based immunotherapy with chemotherapy is a potential strategy for brain tumor treatment. [3] |
| 分子式 |
C29H35N7O
|
|
|---|---|---|
| 分子量 |
497.6345
|
|
| 精确质量 |
497.29
|
|
| 元素分析 |
C, 69.99; H, 7.09; N, 19.70; O, 3.21
|
|
| CAS号 |
1668565-74-9
|
|
| 相关CAS号 |
|
|
| PubChem CID |
90718185
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| LogP |
6.5
|
|
| tPSA |
98.8
|
|
| 氢键供体(HBD)数目 |
3
|
|
| 氢键受体(HBA)数目 |
5
|
|
| 可旋转键数目(RBC) |
9
|
|
| 重原子数目 |
37
|
|
| 分子复杂度/Complexity |
686
|
|
| 定义原子立体中心数目 |
0
|
|
| SMILES |
O=C(N([H])C1C([H])=C([H])C(C([H])([H])[H])=C([H])C=1[H])N([H])C1C([H])=C(C2=C([H])C([H])=C([H])C([H])=C2C2N=NN([H])N=2)C([H])=C([H])C=1N(C([H])([H])C([H])(C([H])([H])[H])C([H])([H])[H])C([H])([H])C([H])(C([H])([H])[H])C([H])([H])[H]
|
|
| InChi Key |
CJNMMPAEIYFQIJ-UHFFFAOYSA-N
|
|
| InChi Code |
InChI=1S/C29H35N7O/c1-19(2)17-36(18-20(3)4)27-15-12-22(24-8-6-7-9-25(24)28-32-34-35-33-28)16-26(27)31-29(37)30-23-13-10-21(5)11-14-23/h6-16,19-20H,17-18H2,1-5H3,(H2,30,31,37)(H,32,33,34,35)
|
|
| 化学名 |
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 2.5 mg/mL (5.02 mM) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 悬浮液;超声助溶。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (5.02 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL 澄清 DMSO 储备液加入到 900 μL 玉米油中并混合均匀。 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.0095 mL | 10.0476 mL | 20.0953 mL | |
| 5 mM | 0.4019 mL | 2.0095 mL | 4.0191 mL | |
| 10 mM | 0.2010 mL | 1.0048 mL | 2.0095 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。