| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 1mg |
|
||
| 2mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| Other Sizes |
|
| 靶点 |
Guanylate cyclase C
|
|---|---|
| 体外研究 (In Vitro) |
Linaclotide 以浓度依赖性方式在体外抑制 [125I]-STa 与野生型小鼠肠粘膜的结合。相反,GC-C 无效小鼠的[125I]-STa 与这些膜的结合显着减少。在体外空肠液中孵育 30 分钟后,利那洛肽完全降解[1]。利那洛肽作用于管腔膜上的鸟苷酸环化酶-C受体,增加肠道内氯化物和碳酸氢盐的分泌,抑制钠离子的吸收,从而增加管腔内水分的分泌,改善排便;该药物被最低限度地吸收到体循环中[2]。
|
| 体内研究 (In Vivo) |
药代动力学分析显示口服生物利用度非常低(0.10%)。在肠道分泌和运输模型中,利那洛肽在野生型小鼠中表现出显着的药理作用,但在 GC-C 缺失小鼠中则不然:诱导手术结扎的空肠环中液体分泌增加,伴随着环状鸟苷-3',5 水平的分泌升高-单磷酸盐和加速胃肠道转运[1]。利那洛肽显着增加每周自发排便和完全自发排便 (CSBM),同时减少慢性便秘患者的腹痛[2]。
|
| 酶活实验 |
肠粘膜结合试验[1]
STa(p)被放射性碘化(2.200 Ci/mmol),并按照Thompson等人1985年的描述进行纯化。在产生的两种单碘化形式的STa中,分离、纯化了第四种酪氨酸标记的STa,并将其用作本研究中的示踪剂。结合反应在50µl反应中进行,该反应含有0.1 M pH 5.0的乙酸钠、0.2%的BSA、肠粘膜蛋白(50µg)、53000 cpm[125I]-STa(11 fmol,217 pM)和0.3 nM至1.0µM的利那洛肽竞争对手。在37°C下孵育30分钟后,通过真空过滤将反应应用于Whatman GF/C玻璃纤维过滤器(用1%聚乙烯吡咯烷酮预处理)。然后用冰冷的PBS缓冲液冲洗过滤器,并在闪烁计数器中测量捕获的[125I]-STa放射性配体。特异性结合是通过从总结合中减去在过量未标记的利那洛肽存在下结合的[125I]-STa来确定的。使用GraphPad Prism生成竞争性放射性配体结合曲线。结合数据的非线性回归分析用于计算导致50%放射性配体结合的竞争对手浓度(IC50)。由于这些测定中使用的[125I]-STa浓度为217 pM,与其解离常数相比非常小,因此计算出的IC50和Ki值实际上是相同的。结果表示为平均值±平均值标准误差(SEM)。 利那洛肽在肠液中的代谢[1] 为了收集小肠液样本,两只小鼠禁食过夜,但可以随意使用过滤后的自来水。对麻醉(异氟烷)小鼠进行剖腹手术,并将其小肠取出。在形成1至3厘米长的环之前,用3毫升20毫摩尔Tris-HCl缓冲液(pH 7.5)冲洗选定用于结扎的空肠区域,然后注射0.2毫升赋形剂(含10毫摩尔葡萄糖、10毫摩尔HEPES、pH 7.0的克雷布斯-林格溶液)(KRGH)。缝合腹壁和皮肤,让动物恢复30分钟。恢复后,处死小鼠,切除环,取出液体并储存在-20°C下Linaclotide(0.1 mg/ml)在37°C下在0.010 ml肠液或0.010 ml磷酸盐缓冲盐水(PBS)(对照)中孵育不同时间。通过加入0.015 ml PBS和一体积冰冷的12%三氯乙酸(TCA)停止反应,涡旋并在4°C下以16000×g离心5分钟Linaclotide降解通过LC-MS/MS进行分析,使用MassLynx 4.0 SP4版软件进行分子量预测和数据分析。 |
| 动物实验 |
Mice: Three groups (n=3) of female CD-1 mice receive linaclotide (8 mg/kg) intravenously (i.v.), and two groups (n=3) receive linaclotide (8 mg/kg) by gavage (p.o.) in order to assess oral bioavailability. After allowing blood to clot for five minutes, serum is collected and kept at -80°C until sample preparation and LC-MS/MS analysis[1]. The blood is then centrifuged at 13,000×g for three minutes.
Oral bioavailability of Linaclotide in mice [1] To determine oral bioavailability, three groups (n = 3) of female CD-1 mice received Linaclotide (8 mg/kg) intravenously (i.v.), while two groups (n = 3) received Linaclotide (8 mg/kg) by gavage (p.o.). Blood was allowed to clot for 5 min, centrifuged at 13,000 × g for 3 min, and the serum was collected and stored at − 80 °C until sample preparation and analysis by LC–MS/MS. The concentration of linaclotide was determined based on a standard concentration curve of linaclotide generated using a set of standards prepared in mouse serum (lower limit of quantitation was 1.0 ng/ml). Data were collected using Waters MassLynx version 4.0 software. Linaclotide serum concentrations were plotted as a function of time using GraphPad Prism 5.0 software. Pharmacokinetic parameters for oral and intravenous administration were calculated using WinNonlin version 5.2. If no analyte was detected, the concentration was set to zero for calculations of the AUC and oral bioavailability. Intestinal fluid secretion assay [1] Intestinal loops in wt and GC-C null mice (n = 5–7/group) were surgically ligated after the mice had been placed under isofluorane anesthesia and laparotomy was performed to exteriorize the small intestine. The small intestines were flushed with Krebs–Ringer buffer (K–R, 10 mM glucose, 10 mM HEPES) pH 7.0 (KRGH) and a loop of approximately 3 cm in length was created halfway between the stomach and the cecum. Loops were injected with either 100 µl Linaclotide (5 µg) or 100 µl vehicle (KRGH), and the animals were allowed to recover for 90 min prior to euthanasia. The loops were then excised and the length and weight of each loop was recorded both prior to and after collection of the intestinal fluid content. Fluid secretion was calculated and expressed as the weight to length ratio (W/L), a commonly used surrogate to measure intestinal secretion. Gastrointestinal transit in mice [1] Male and female wt and GC-C null mice (n = 9/group) were fasted overnight, having access to water ad libitum. The mice received oral doses (200 µl) of either Linaclotide (100 µg/kg) or vehicle (20 mM Tris–HCl, pH 7.5) 10 min prior to a dose of 10% activated carbon/10% gum arabic powder suspension (200 µl in water) administered by gavage. After 5 min, the animals were euthanized and their intestines ranging from the stomach to the cecum were removed. Gastrointestinal transit is expressed as the percentage of the total length of the small intestine traveled by the charcoal front. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Linaclotide is minimally absorbed with negligible systemic availability following oral administration; however, systemic exposure is not of importance for the maximal effects of linaclotide, as the ligand-binding domain of the GC-C target is located on the luminal surface of intestinal epithelial cells. There is no available information regarding the area under the curve (AUC) and peak plasma concentrations (Cmax) as the concentrations of linaclotide and its active metabolite in plasma are below the limit of quantitation. Following once-daily administration of 290 mcg linaclotide for seven days, the average active peptide recovery in the stool samples of fed and fasted healthy subjects was 3% and 5%, respectively. The recovered active peptide constituted the active metabolite. Given that linaclotide plasma concentrations following recommended oral doses are not measurable, linaclotide is not expected to be distributed to tissues to any clinically relevant extent. No information is available. Given that linaclotide plasma concentrations following therapeutic oral doses are not measurable, linaclotide is expected to be minimally distributed to tissues. Active peptide recovery in the stool samples of fed and fasted subjects following the daily administration of 290 mcg of Linzess for seven days averaged about 5% (fasted) and about 3% (fed) and virtually all as the active metabolite. Linzess is minimally absorbed with low systemic availability following oral administration. Concentrations of linaclotide and its active metabolite in plasma are below the limit of quantitation after oral doses of 145 ug or 290 ug were administered. Therefore, standard pharmacokinetic parameters such as area under the curve (AUC), maximum concentration (Cmax), and half-life cannot be calculated. It is not known whether linaclotide is distributed into human milk. For more Absorption, Distribution and Excretion (Complete) data for Linaclotide (8 total), please visit the HSDB record page. Metabolism / Metabolites Linaclotide is metabolized in the small intestine, where it loses its C-terminal tyrosine moiety to form a principal active metabolite, MM-419447. The disulfide bonds of linaclotide and MM-419447 are reduced in the intestinal lumen, followed by proteolysis and degradation to form smaller peptides and naturally occurring amino acids which are absorbed through the intestine. In rats _in vitro_, linaclotide was resistant to enzymatic hydrolysis by pepsin, trypsin, aminopeptidase or chymotrypsin. The metabolism of linaclotide was investigated in a set of experiments, predominantly in rodents. Linaclotide is metabolised in the intestine by immediate break down of the disulfide bridges which prone linaclotide to further digestion by the enzymes present in the gastrointestinal environment. Several breakdown products containing 3-13 amino acids have been identified. Only one metabolite, MM-419447, was shown to be pharmacodynamic active. Linaclotide is metabolized within the gastrointestinal tract to its principal, active metabolite by loss of the terminal tyrosine moiety. Both linaclotide and the metabolite are proteolytically degraded within the intestinal lumen to smaller peptides and naturally occurring amino acids. ... We examined the metabolic stability of linaclotide in conditions that mimic the gastrointestinal tract and characterized the metabolite MM-419447 (CCEYCCNPACTGC), which contributes to the pharmacologic effects of linaclotide. Systemic exposure to these active peptides is low in rats and humans, and the low systemic and portal vein concentrations of linaclotide and MM-419447 observed in the rat confirmed both peptides are minimally absorbed after oral administration. Linaclotide is stable in the acidic environment of the stomach and is converted to MM-419447 in the small intestine. The disulfide bonds of both peptides are reduced in the small intestine, where they are subsequently proteolyzed and degraded. After oral administration of linaclotide, <1% of the dose was excreted as active peptide in rat feces and a mean of 3-5% in human feces; in both cases MM-419447 was the predominant peptide recovered. MM-419447 exhibits high-affinity binding in vitro to T84 cells, resulting in a significant, concentration-dependent accumulation of intracellular cyclic guanosine-3',5'-monophosphate (cGMP). In rat models of gastrointestinal function, orally dosed MM-419447 significantly increased fluid secretion into small intestinal loops, increased intraluminal cGMP, and caused a dose-dependent acceleration in gastrointestinal transit. These results demonstrate the importance of the active metabolite in contributing to linaclotide's pharmacology. Biological Half-Life There is no available information regarding the half-life as the concentrations of linaclotide and its active metabolite in plasma are below the limit of quantitation. Two male and two female monkeys were intravenously dosed for seven consecutive days with 15 mg/kg/day linaclotide. ... /The/ mean half life was approximately 1.5 hr on day 1 and 7 for both genders. Absorption of linaclotide into the systemic circulation is minimal. In a study by Busby et al.,11 patients were given 290 μg of linaclotide once daily for seven days, and then plasma samples were drawn. No quantifiable concentrations of linaclotide or its primary metabolite, MM-419447, were found. This finding mirrored other absorption data from clinical trials. When linaclotide was administered at a one-time dose of 2897 μg, quantifiable concentrations of linaclotide were found in 2 of 18 participants, but the primary metabolite was undetectable. In a Phase III trial in patients with IBS-C or CC receiving linaclotide (290 or 145 μg, respectively), only 2 of 465 patients had detectable plasma linaclotide concentrations; the linaclotide concentrations were under 0.5 ng/mL, and no patient had quantifiable levels of the primary metabolite. Distribution of linaclotide is minimal because of the drug’s local action on the gut and minimal absorption into the systemic circulation.[2] Linaclotide was shown to be relatively stable in gastric fluid. It was not metabolized during three hours of in vitro incubation with trypsin, pepsin, aminopeptidase, or chymotrypsin. Its 13-amino acid active metabolite, MM-419447, was produced by incubating linaclotide with carboxypeptidase A. Linaclotide was almost completely converted to MM-419447 by carboxypeptidase A after six hours of digestion. In animal studies, linaclotide was metabolized more quickly in the duodenum and jejunal loops than in the ileal loop. In order for linaclotide and its metabolite to be completely degraded (and thus lose their pharmacologic activity), the peptides undergo disulfide bond reduction in the intestine, which then makes them susceptible to proteolytic digestion, by which the peptides are broken down into smaller peptides and amino acids and recycled by the body.[2] In a Phase I open-label, two-period, crossover food-effect study in healthy volunteers, stool samples were gathered after oral administration of 290 μg of linaclotide once daily for seven days and then again after a single dose of 2897 μg.12 Almost all of the active peptide recovered in the feces was in the form of the primary metabolite, MM-419447. Recovery of active peptide ranged from 0 to 20% (mean, 3–5%) of the administered linaclotide dose. Only after the 2897-μg dose was given with a meal was the parent compound found (in 3 of 9 participants at a median of 0.4% of the administered linaclotide dose).[2] |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
IDENTIFICATION AND USE: Linaclotide is a white to off-white powder. Linaclotide is used in adults in adults for the treatment of irritable bowel syndrome with constipation. It is also used in adults for the treatment of chronic idiopathic constipation. HUMAN EXPOSURE AND TOXICITY: There is limited experience with overdose of linaclotide. During the clinical development program of linaclotide, single doses of 2897 ug were administered to 22 healthy volunteers; the safety profile in these subjects was consistent with that in the overall linaclotide-treated population, with diarrhea being the most commonly reported adverse reaction. Linaclotide is contraindicated in infants and children younger than 6 years of age and should be avoided in children and adolescents 6-17 years of age. While safety and effectiveness has not been established in pediatric patients less than 18 years of age, linaclotide caused deaths in young juvenile mice when administered in single, clinically relevant, adult oral doses. Linaclotide was not genotoxic in the in vitro chromosomal aberration assay in cultured human peripheral blood lymphocytes. ANIMAL STUDIES: In rats, there was no detectable systemic exposure to linaclotide at single oral dose levels of up to 5.0 mg/kg. There were no linaclotide-related effects observed on survival, body weight, food consumption, clinical observations, or macroscopic evaluations. Cynomolgus monkeys were administered a single oral dose of linaclotide at dose levels of 0.5, 1.5, 3.0, and 5.0 mg/kg. The monkeys that were administered a single oral dose of linaclotide (1.5 mg/kg or greater) exhibited changes in stool consistency (non-formed and/or liquid feces), qualitatively reduced food consumption, and/or abdominal distention. There were no significant changes in individual body weight data for these animals. A monkey dosed orally for five consecutive days at 1.5 mg/kg/day exhibited non-formed and liquid feces over the course of the dosing period, with mild abdominal distention occurring on the fourth dosing day. These results demonstrated that linaclotide was well tolerated by Cynomolgus monkeys following a single oral dose at dose levels up to 5.0 mg/kg. However, deaths in juvenile mice were seen when linaclotide was administered in clinically relevant adult doses. In neonatal mice, linaclotide caused deaths at 10 ug/kg/day after oral administration of 1 or 2 daily doses on post-natal day 7. These deaths were due to rapid and severe dehydration. Supplemental subcutaneous fluid administration prevented death after linaclotide administration in neonatal mice. In studies conducted without supplemental fluid administration, tolerability to linaclotide increases with age in juvenile mice. In 2-week-old mice, linaclotide was well tolerated at a dose of 50 ug/kg/day, but deaths occurred after a single oral dose of 100 ug/kg. In 3-week-old mice, linaclotide was well tolerated at 100 ug/kg/day, but deaths occurred after a single oral dose of 600 ug/kg. Linaclotide was well tolerated and did not cause death in 4-week-old juvenile mice at a dose of 1,000 ug/kg/day for 7 days and in 6-week-old juvenile mice at a dose of 20,000 ug/kg/day for 28 days. The potential for linaclotide to cause teratogenic effects was studied in rats, rabbits and mice. Oral administration of up to 100 mg/kg/day in rats and 40 mg/kg/day in rabbits produced no maternal toxicity and no effects on embryo-fetal development. In mice, oral dose levels of at least 40 mg/kg/day produced severe maternal toxicity including death, reduction of gravid uterine and fetal weights, and effects on fetal morphology. Oral doses of 5 mg/kg/day did not produce maternal toxicity or any adverse effects on embryo-fetal development in mice. Linaclotide had no effect on fertility or reproductive function in male and female rats at oral doses of up to 100,000 ug/kg/day. Linaclotide was not genotoxic in an in vitro bacterial reverse mutation (Ames) assay. Hepatotoxicity In clinical trials, linaclotide therapy was not associated with significant changes in serum enzyme levels or episodes of clinically apparent liver injury. Minor transient ALT elevations arose in Likelihood score: E (unlikely cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Linaclotide is minimally absorbed from the gastrointestinal tract and the drug and its active metabolite are not measurable in milk following administration of doses up to 290 mcg daily. Linaclotide appears to be acceptable in nursing mothers and no special precautions are required. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding No information is available. The safey of linaclotide has been demonstrated in several clinical studies. The most commonly reported adverse event is mild-to-moderate diarrhea (Table 3); other commonly reported events are flatulence and abdominal pain. In a 12-week trial, patients receiving linaclotide had comparable types and rates of adverse events. Rates of discontinuation were higher in the linaclotide group (4.7% in patients receiving 145 μg and 3.8% in those receiving 290 μg) than among placebo users (0.5%), which was attributed to treatment-associated diarrhea. A larger portion of the linaclotide group (1.5% versus 0.2% for placebo users) had diarrhea that was graded as severe by an investigator. No clinically significant between-group differences in hematology or blood chemistry values, urinalysis or electrocardiogram (ECG) findings, or vital signs were found. During the previously summarized 26-week trial, safety findings mirrored those in the 12-week trial. Diarrhea was more likely in the linaclotide group versus the placebo group, and the discontinuation rate was also higher in the linaclotide group. Of the patients who reported diarrhea while receiving linaclotide, 7.7% had mild, 10.0% had moderate, and 2.0% had severe diarrhea. Most patients reported treatment-emergent diarrhea within the first 4 weeks of therapy. No differences in vital signs, hematology or blood chemistry values, or ECG parameters were reported.[2] |
| 参考文献 |
|
| 其他信息 |
Therapeutic Uses
Linzess (linaclotide) is indicated in adults for the treatment of irritable bowel syndrome with constipation (IBS-C). /Included in US product label/ Linzess is indicated in adults for the treatment of chronic idiopathic constipation (CIC). /Included in US product label/ Drug Warnings /BOXED WARNING/ WARNING: PEDIATRIC RISK. Linzess is contraindicated in pediatric patients up to 6 years of age; in nonclinical studies, administration of a single, clinically relevant adult oral dose of linaclotide caused deaths due to dehydration in young juvenile mice. Avoid use of Linzess in pediatric patients 6 through 17 years of age. The safety and efficacy of Linzess has not been established in pediatric patients under 18 years of age. Linaclotide is contraindicated in infants and children younger than 6 years of age and should be avoided in children and adolescents 6-17 years of age. Safety and efficacy of linaclotide in pediatric patients have not been established, and the drug has caused deaths in toxicology studies in juvenile mice 1-3 weeks of age (approximately equivalent to infants younger than 2 years of age). The deaths in young juvenile mice occurred following 1 or 2 doses of linaclotide 10 ug/kg administered once daily beginning on postnatal day 7, single oral doses of 100 ug/kg on day 14, and single oral doses of 600 ug/kg on day 21. Although no deaths occurred in juvenile mice 6 weeks of age (approximately equivalent to adolescents 12-17 years of age) receiving linaclotide 20,000 ug/kg daily for 28 days, use of the drug in children and adolescents 6-17 years of age should be avoided because of the deaths reported in younger mice and the lack of safety and efficacy data in pediatric patients.1 No data are available for mice between 3 and 6 weeks of age. Severe diarrhea was reported in clinical trials in 2% of patients receiving linaclotide for treatment of either irritable bowel syndrome (IBS) with constipation or chronic idiopathic constipation. If severe diarrhea occurs, treatment with the drug should be interrupted or discontinued. It is not known whether linaclotide is distributed into human milk. Although plasma concentrations of linaclotide and its active metabolite are not measurable following oral administration at recommended dosages, caution is advised when linaclotide is administered to nursing women. For more Drug Warnings (Complete) data for Linaclotide (10 total), please visit the HSDB record page. Pharmacodynamics Linaclotide is a laxative with visceral analgesic and secretory activities. In animal studies and clinical trials, linaclotide improved constipation and gastrointestinal symptoms in patients with irritable bowel syndrome with predominant constipation and chronic idiopathic constipation. In animal models, linaclotide has been shown to both accelerate gastrointestinal transit and reduce intestinal pain. In an animal model of visceral pain, linaclotide reduced abdominal muscle contraction and decreased the activity of pain-sensing nerves. Taking linaclotide with a high-fat meal results in looser stools and a higher stool frequency than taking it in the fasted state. Linaclotide binds to its target, guanylate cyclase-C (GC-C), with high affinity and selectivity. Linaclotide and its active metabolite act locally on the luminal surface of the intestinal epithelium. As linaclotide is stable under a highly acidic pH environment, it acts in a pH-independent manner. Aims Linaclotide is an orally administered 14-amino acid peptide being developed for the treatment of constipation-predominant irritable bowel syndrome (IBS-C) and chronic constipation. We determined the stability of linaclotide in the intestine, measured the oral bioavailability, and investigated whether the pharmacodynamic effects elicited in rodent models of gastrointestinal function are mechanistically linked to the activation of intestinal guanylate cyclase C (GC-C). Main methods Linaclotide binding to intestinal mucosal membranes was assessed in competitive binding assays. Stability and oral bioavailability of linaclotide were measured in small intestinal fluid and serum, respectively, and models of gastrointestinal function were conducted using wild type (wt) and GC-C null mice. Key findings Linaclotide inhibited in vitro [125I]-STa binding to intestinal mucosal membranes from wt mice in a concentration-dependent manner. In contrast, [125I]-STa binding to these membranes from GC-C null mice was significantly decreased. After incubation in vitro in jejunal fluid for 30 min, linaclotide was completely degraded. Pharmacokinetic analysis showed very low oral bioavailability (0.10%). In intestinal secretion and transit models, linaclotide exhibited significant pharmacological effects in wt, but not in GC-C null mice: induction of increased fluid secretion into surgically ligated jejunal loops was accompanied by the secretion of elevated levels of cyclic guanosine-3′,5′-monophosphate and accelerated gastrointestinal transit. Significance Linaclotide is a potent and selective GC-C agonist that elicits pharmacological effects locally in the gastrointestinal tract. This pharmacological profile suggests that orally administered linaclotide may be capable of improving the abdominal symptoms and bowel habits of patients suffering from IBS-C and chronic constipation.[1] Purpose: The pharmacology, pharmaco-kinetics, and clinical efficacy and safety of linaclotide in the management of chronic constipation (CC) and constipation-predominant irritable bowel syndrome (IBS-C) are reviewed. Summary: Linaclotide (Linzess, Forest Pharmaceuticals) is a 14-amino acid peptide indicated for the treatment of adults with CC and IBS-C. Linaclotide acts on guanylate cyclase-C receptors on the luminal membrane to increase chloride and bicarbonate secretions into the intestine and inhibit the absorption of sodium ions, thus increasing the secretion of water into the lumen and improving defecation; the drug is minimally absorbed into the systemic circulation. Linaclotide is approved by the Food and Drug Administration (FDA) for oral once-daily administration at doses of 145 μg for CC and 290 μg for IBS-C. In placebo-controlled Phase III clinical trials, linaclotide significantly increased weekly spontaneous bowel movements and complete spontaneous bowel movements (CSBMs) while reducing abdominal pain in patients with CC. In patients with IBS-C, linaclotide was demonstrated to be effective in meeting FDA-recommended endpoints such as reductions of at least 30% from baseline in abdominal pain scores and CSBM frequency. The most common adverse effect of linaclotide is diarrhea, which was reported in 16-20% of clinical trial participants. Conclusion: Linaclotide is an important advance in the treatment of CC and IBS-C, with a novel mechanism of action resulting in accelerated intestinal transit. In clinical trials, linaclotide demonstrated efficacy relative to placebo for treatment of both CC and IBS-C. Linaclotide's adverse effects are generally mild and confined to the gastrointestinal tract. |
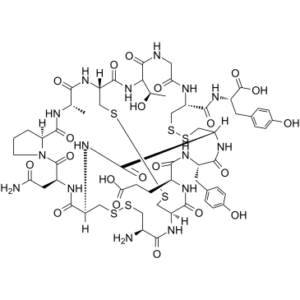
| 分子式 |
C59H79N15O21S6
|
|---|---|
| 分子量 |
1526.74000
|
| 精确质量 |
1525.389
|
| 元素分析 |
C, 46.41; H, 5.22; N, 13.76; O, 22.01; S, 12.60
|
| CAS号 |
851199-59-2
|
| 相关CAS号 |
851199-60-5 (acetate); 851199-59-2
|
| PubChem CID |
16158208
|
| 序列 |
H-Cys(1)-Cys(2)-Glu-Tyr-Cys(3)-Cys(1)-Asn-Pro-Ala-Cys(2)-Thr-Gly-Cys(3)-Tyr-OH
L-cysteinyl-L-cysteinyl-L-alpha-glutamyl-L-tyrosyl-L-cysteinyl-L-cysteinyl-L-asparagyl-L-prolyl-L-alanyl-L-cysteinyl-L-threonyl-glycyl-L-cysteinyl-L-tyrosine (1->6),(2->10),(5->13)-tris(disulfide) |
| 短序列 |
CCEYCCNPACTGCY
H-C(1)C(2)EYC(3)C(1)NPAC(2)TGC(3)Y-OH |
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
1.6±0.1 g/cm3
|
| 沸点 |
2045.0±65.0 °C at 760 mmHg
|
| 闪点 |
1190.5±34.3 °C
|
| 蒸汽压 |
0.0±0.3 mmHg at 25°C
|
| 折射率 |
1.712
|
| LogP |
-5.84
|
| tPSA |
725.71
|
| 氢键供体(HBD)数目 |
19
|
| 氢键受体(HBA)数目 |
28
|
| 可旋转键数目(RBC) |
13
|
| 重原子数目 |
101
|
| 分子复杂度/Complexity |
3030
|
| 定义原子立体中心数目 |
14
|
| SMILES |
O=C1[C@H](CC(=O)N)NC(=O)[C@@H]2CSSC[C@@H](C(N[C@@H]3C(N[C@H](C(N[C@H](C(N[C@H](C(N2)=O)CSSC[C@@H](C(=O)N[C@H](C(=O)O)CC2C=CC(O)=CC=2)NC(=O)CNC(=O)[C@H]([C@H](O)C)NC(=O)[C@H](CSSC3)NC(=O)[C@H](C)NC(=O)[C@@H]2CCCN12)=O)CC1C=CC(O)=CC=1)=O)CCC(=O)O)=O)=O)N
|
| InChi Key |
KXGCNMMJRFDFNR-WDRJZQOASA-N
|
| InChi Code |
InChI=1S/C59H79N15O21S6/c1-26-47(82)69-41-25-101-99-22-38-52(87)65-33(13-14-45(80)81)49(84)66-34(16-28-5-9-30(76)10-6-28)50(85)71-40(54(89)72-39(23-97-96-20-32(60)48(83)70-38)53(88)67-35(18-43(61)78)58(93)74-15-3-4-42(74)56(91)63-26)24-100-98-21-37(64-44(79)19-62-57(92)46(27(2)75)73-55(41)90)51(86)68-36(59(94)95)17-29-7-11-31(77)12-8-29/h5-12,26-27,32-42,46,75-77H,3-4,13-25,60H2,1-2H3,(H2,61,78)(H,62,92)(H,63,91)(H,64,79)(H,65,87)(H,66,84)(H,67,88)(H,68,86)(H,69,82)(H,70,83)(H,71,85)(H,72,89)(H,73,90)(H,80,81)(H,94,95)/t26-,27+,32-,33-,34-,35-,36-,37-,38-,39-,40-,41-,42-,46-/m0/s1
|
| 化学名 |
(2S)-2-[[(1R,4S,7S,13S,16R,21R,24R,27S,30S,33R,38R,44S)-21-amino-13-(2-amino-2-oxoethyl)-27-(2-carboxyethyl)-44-[(1R)-1-hydroxyethyl]-30-[(4-hydroxyphenyl)methyl]-4-methyl-3,6,12,15,22,25,28,31,40,43,46,51-dodecaoxo-18,19,35,36,48,49-hexathia-2,5,11,14,23,26,29,32,39,42,45,52-dodecazatetracyclo[22.22.4.216,33.07,11]dopentacontane-38-carbonyl]amino]-3-(4-hydroxyphenyl)propanoic acid
|
| 别名 |
MM 416775; Linaclotide; Linzess; 851199-59-2; Constella; UNII-N0TXR0XR5X; Linaclotida; HSDB 8224; Linaclotide [USAN:INN]; MM416775; MD-1100 acetate; MM-416775; Linzess; Linaclotide acetate; Linzess Constela
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO: ~50 mg/mL (~32.8 mM)
H2O: ~16.7 mg/mL (~10.9 mM) |
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (1.64 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (1.64 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (1.64 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: 4.17 mg/mL (2.73 mM) in PBS (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶 (<60°C). 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 0.6550 mL | 3.2750 mL | 6.5499 mL | |
| 5 mM | 0.1310 mL | 0.6550 mL | 1.3100 mL | |
| 10 mM | 0.0655 mL | 0.3275 mL | 0.6550 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT03796884 | Active Recruiting |
Drug: Linaclotide Other: Placebo |
Colorectal Adenoma Stage 0 Colorectal Cancer AJCC v8 |
Sidney Kimmel Cancer Center at Thomas Jefferson University |
October 30, 2019 | Phase 2 |
| NCT03119584 | Active Recruiting |
Drug: linaclotide or placebo | Chronic Constipation Diabete Mellitus |
Texas Tech University Health Sciences Center, El Paso |
September 1, 2015 | Phase 4 |
| NCT05652205 | Recruiting | Drug: Linaclotide Drug: Placebo for Linaclotide |
Chronic Idiopathic Constipation (CIC) Functional Constipation (FC) |
AbbVie | December 29, 2022 | Phase 3 |
| NCT06091735 | Recruiting | Drug: OSS Drug: OSS+Linzess Drug: PEG-Interferon Alfa |
Bowel Preparation | Jinling Hospital, China | August 1, 2023 | Not Applicable |
| NCT05760313 | Recruiting | Drug: Linaclotide Drug: Placebo |
Functional Constipation | AbbVie | April 27, 2023 | Phase 2 |