| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 2mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| 5g |
|
||
| 10g |
|
||
| Other Sizes |

| 靶点 |
Progesterone receptor
|
|---|---|
| 体外研究 (In Vitro) |
在 T47D 细胞中,甲羟孕酮(10 nM,48 小时)通过 PI3K/Akt 信号通路刺激 Cyclin D1 的产生,从而促进细胞增殖 [1]。通过提高 HUVEC 中信号分子的表达,甲羟孕酮(100 nM,24 小时)增加了 HUVEC 上单核细胞标记物的数量,这可能是动脉粥样硬化的原因 [2]。
|
| 体内研究 (In Vivo) |
甲羟孕酮(27.7 μg/天,皮下注射)虽能增强血栓形成,但能抑制动脉血管血栓形成[3]。
MPA和MPA + e2治疗的动物表现出加重的血栓反应,表现为稳定闭塞的时间显著缩短。MPA的促血栓作用与ETP升高平行,而血小板活化不受影响。此外,MPA + E2减少了α -平滑肌肌动蛋白阳性细胞的数量,增加了斑块基质中的透明质酸。有趣的是,总斑块负担减少了MPA,但MPA + E2没有变化[3]。
结论和意义:长期服用MPA和MPA + E2可增加apoe缺陷小鼠动脉血栓形成,尽管MPA对动脉粥样硬化有抑制作用。凝血酶形成增加,平滑肌含量减少和非胶原斑块基质重塑可能参与促血栓作用。因此,MPA对动脉血栓形成和动脉粥样硬化的影响不同[3]。
甲羟孕酮醋酸酯(MPA)和MPA + e2治疗的动物表现出加重的血栓反应,表现为稳定闭塞的时间显著缩短。MPA的促血栓作用与ETP升高平行,而血小板活化不受影响。此外,MPA + E2减少了α -平滑肌肌动蛋白阳性细胞的数量,增加了斑块基质中的透明质酸。有趣的是,MPA降低了总斑块负担,但MPA + E2没有改变。 结论和意义:长期服用MPA和MPA + E2可增加apoe缺陷小鼠动脉血栓形成,尽管MPA对动脉粥样硬化有抑制作用。凝血酶形成增加,平滑肌含量减少和非胶原斑块基质重塑可能参与促血栓作用。因此,MPA对动脉血栓形成和动脉粥样硬化的影响是不同的。[4] |
| 酶活实验 |
醋酸甲羟孕酮(MPA)诱导乳腺癌细胞增殖的机制尚不清楚。本研究探讨了MPA影响孕激素受体(PR)阳性T47D人乳腺癌细胞中cyclin D1表达的机制。MPA (10 nM)处理48 h,细胞增殖率达到1.6倍。MPA诱导细胞周期蛋白D1表达(诱导率为3.3倍),选择性PR拮抗剂RU486阻断MPA诱导的细胞增殖和细胞周期蛋白D1表达(抑制率为23%)。MPA使转染PRB而不转染PRA的MCF-7细胞中cyclin D1的蛋白水平(诱导率为2.2倍)和启动子活性(诱导率为2.7倍)均升高。虽然MPA转录激活了cyclin D1的表达,但cyclin D1启动子没有孕激素应答元件相关序列。我们进一步研究了cyclin D1表达调控的机制。由于cyclin D1启动子包含三个假定的核因子- kappab (NFkappaB)结合基序,并且NFkappaB是Akt的底物,因此我们研究了磷脂酰肌醇3-激酶(PI3K)/Akt/NFkappaB级联对cyclin D1对MPA的反应的影响。MPA诱导Akt瞬时磷酸化(5 min诱导2.7倍),PI3K抑制剂(wortmannin)处理可减弱MPA诱导的cyclin D1表达上调(抑制40%)和细胞增殖(抑制40%)。MPA还诱导了NFkappaBalpha抑制剂(IkappaBalpha)的磷酸化(诱导率为2.3倍),而wortmannin处理可减弱MPA诱导的IkappaBalpha磷酸化(抑制率为60%)。用IkappaBalpha磷酸化抑制剂(BAY 11-7085)或特异性NFkappaB核易位抑制剂(SN-50)处理可以减弱mpa诱导的cyclin D1表达上调(分别抑制80%和50%)和细胞增殖(分别抑制55%和34%)。由于MPA诱导Akt的短暂磷酸化,且cyclin D1启动子不含孕酮响应元件相关序列,因此MPA通过PRB通过PI3K/Akt/NFkappaB级联上调cyclin D1表达诱导细胞增殖可能是非基因组机制[1]。
本文首次利用秀丽隐杆线虫(Cunninghamella elegans)、玫瑰毛霉(Trichothecium roseum)和铅毛霉(Mucor plumbeus)研究了甲氧孕酮(1)的真菌转化。得到的代谢物如下:6β,20-dihydroxymedroxyprogesterone(2), 12个β-hydroxymedroxyprogesterone(3), 6β,11β-dihydroxymedroxyprogesterone(4), 16β-hydroxymedroxyprogesterone(5), 11α,17-dihydroxy-6α-methylpregn-4-ene-3, 20-dione (6), 11-oxo-medroxyprogesterone(7) 6α-methyl-17α-hydroxypregn-1, 4-diene-3, 20-dione(8)和6β-hydroxymedroxyprogesterone(9), 15β-hydroxymedroxyprogesterone(10), 6α-methyl-17α,11β-dihydroxy-5α-pregnan-3, 20-dione(11), 11个β-hydroxymedroxyprogesterone(12)和11α,20-dihydroxymedroxyprogesterone(13)。在所有微生物转化产物中,新分离的生物转化产物13对SH-SY5Y细胞的增殖活性最强。化合物12、5、6、9、11和3对SH-SY5Y肿瘤细胞系也显示出一定程度的活性(活性由高到低)。从未报道过的生物转化产物2显示出对乙酰胆碱酯酶最有效的抑制活性。进行分子模拟研究是为了了解观察到的实验活动,也为了获得更多关于生物转化产物与酶之间的结合模式和相互作用的信息。[4] |
| 细胞实验 |
细胞增殖测定[1]
细胞类型: T47D 测试浓度: 10 nM 孵育时间: 24 小时、48小时、72小时 实验结果:48小时时细胞数量增加。 蛋白质印迹分析 [1] 细胞类型: T47D 测试浓度: 10 nM 孵育时间: 4小时 实验结果:诱导Cyclin D1蛋白表达。 RT-PCR[2] 细胞类型: HUVEC 测试浓度: 100 nM 孵育时间: 24小时 实验结果:粘附分子的mRNA和蛋白表达增加。 在HUVECs中,通过实时PCR检测粘附分子mRNA水平。免疫细胞化学和酶联免疫吸附测定蛋白表达。为了模拟单核细胞粘附内皮细胞,我们使用了一个流动室系统来评估孕激素对U937单核细胞粘附HUVEC单层的影响。我们还研究了小干扰rna对粘附分子的抑制作用。[2] |
| 动物实验 |
Animal/Disease Models: ApoE-/- mouse model [3]
Doses: 27.7 μg/day Route of Administration: sc Experimental Results: diminished atherosclerotic plaque and increased thrombosis. Apolipoprotein E (ApoE)-/- mice were bilaterally ovariectomized and treated with placebo, MPA (27.7 microg day(-1)) and MPA + 17-beta-oestradiol (E2; 1.1 microg day(-1)) for 90 days, on a Western-type diet. Thrombotic response was measured in a photothrombosis model, platelet activation by fluorescence activated cell sorting (FACS) analysis (CD62P) and thrombin generation by the endogenous thrombin potential (ETP). Furthermore, aortic plaque burden and aortic root plaque composition were determined.[3] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
No specific investigation on the absolute bioavailability of medroxyprogesterone (MPA) in humans has been conducted. MPA is rapidly absorbed from the gastrointestinal tract, and maximum MPA concentrations are obtained between 2 to 4 hours after oral administration. Administration of medroxyprogesterone acetate with food increases the bioavailability of MPA. A 10 mg dose of medroxyprogesterone acetate, taken immediately before or after a meal, increased MPA Cmax (50 to 70%) and AUC (18 to 33%). The half-life of MPA was not changed with food. Medroxyprogesterone is approximately 90% protein bound, primarily to albumin; no MPA binding occurs with sex hormone binding globulin. Most MPA metabolites are excreted in the urine as glucuronide conjugates with only minor amounts excreted as sulfates. For more Absorption, Distribution and Excretion (Complete) data for MEDROXYPROGESTERONE (10 total), please visit the HSDB record page. Metabolism / Metabolites Following oral dosing, MPA is extensively metabolized in the liver via hydroxylation, with subsequent conjugation and elimination in the urine. ...MPA is almost exclusively eliminated via hepatic metabolism. In 14 patients with advanced liver disease, MPA disposition was significantly altered (reduced elimination). In patients with fatty liver, the mean percent dose excreted in the 24-hour urine as intact MPA after a 10 mg or 100 mg dose was 7.3% and 6.4%, respectively. Biological Half-Life Elimination half-life of oral preparation is 32 to 44 hr. /Acetate/ |
| 参考文献 |
|
| 其他信息 |
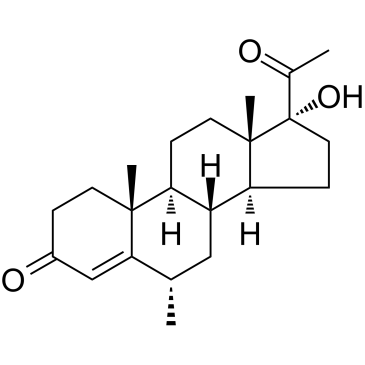
Medroxyprogesterone is a 3-oxo Delta(4)-steroid that is pregn-4-ene-3,20-dione substituted by an alpha-hydroxy group at position 17 and a methyl group at position 6. It has a role as a contraceptive drug, a progestin and a synthetic oral contraceptive. It is a 20-oxo steroid, a 3-oxo-Delta(4) steroid, a 17alpha-hydroxy steroid and a tertiary alpha-hydroxy ketone.
Medroxyprogesterone is a Progestin. Medroxyprogesterone is a synthetic derivative of progesterone administered as an acetate salt (medroxyprogesterone acetate) with antiestrogenic activity. As a do all progestins, medroxyprogesterone binds to and activates nuclear receptors which subsequently bind to and activate target genes for transcription. As an antiestrogen, this agent may inhibit the growth-stimulating effects of estrogen on estrogen-sensitive tumor cells. (NCI04) A synthetic progestational hormone used in veterinary practice as an estrus regulator. Mechanism of Action Medroxyprogesterone shares the pharmacologic actions of the progestins. In women with adequate endogenous estrogen, medroxyprogesterone transforms a proliferative endometrium into a secretory one. Medroxyprogesterone has been shown to have slight androgenic activity in animals. Anabolic effects have also been reported, but the drug apparently lacks appreciable estrogenic activity in humans. In animals, the drug exhibits pronounced adrenocorticoid activity, but a clinically important effect has not been observed in humans. Medroxyprogesterone inhibits the secretion of pituitary gonadotropins following usual IM or subcutaneous dosages (eg, 150 or 104 mg every 3 months), thus preventing follicular maturation and ovulation and resulting in endometrial thinning; these effects result in contraceptive activity. Available evidence indicates that these effects do not occur following oral administration of usual dosages (ie, 5-10 mg daily as single daily doses) of the drug. High doses of medroxyprogesterone inhibit pituitary secretion of luteinizing hormone (LH) and follicle-stimulating hormone (FSH), and will prevent cyclic gonadotropin surges that occur during the normal menstrual cycle. It has been suggested that the drug acts at the hypothalamus since it does not suppress the release of LH and FSH following administration of gonadotropin-releasing hormone and since basal concentrations of LH and FSH remain within the low normal range when the drug is used as a contraceptive. Although the mechanism of action has not been determined, medroxyprogesterone has antineoplastic activity against some cancers (eg, endometrial carcinoma, renal carcinoma). Progestins elicit, to varying degrees, all the pharmacologic responses usually produced by progesterone: induction of secretory changes in the endometrium, increase in basal body temperature (thermogenic action), production of histologic changes in vaginal epithelium, relaxation of uterine smooth muscle, stimulation of mammary alveolar tissue growth, pituitary inhibition, and production of withdrawal bleeding in the presence of estrogen. /Progestins/ Following binding to cytoplasmic receptor protein, steroid is transported to nucleus, and complex is bound there in reactions analogous to those described... for estrogens. However, there is no apparent need for receptor alteration, as with estrogen receptor. /Progesterone/ Although medroxyprogesterone acetate (MPA) is used as an injectable contraceptive, in hormone replacement therapy (HRT) and in treatment of certain cancers, the steroid receptors and their target genes involved in the actions of MPA are not well understood. /Investigators/ show that MPA, like dexamethasone (dex), significantly represses tumour necrosis factor (TNF)-stimulated interleukin-6 (IL-6) protein production in mouse fibroblast (L929sA) cells. In addition, MPA repressed IL-6 and IL-8 promoter-reporter constructs at the transcriptional level, via interference with nuclear factor kappaB (NFkappaB) and activator protein-1 (AP-1). Furthermore, like dex, MPA does not affect NFkappaB DNA-binding activity. /The authors/ also observed significant transactivation by MPA of a glucocorticoid response element (GRE)-driven promoter-reporter construct in both L929sA and COS-1 cells. The MPA-induced nuclear translocation of the glucocorticoid receptor (GR), as well as the antagonistic effects of RU486, strongly suggest that the actions of MPA in these cells are mediated at least in part via the GR. /Investigators/ assessed the transcriptional effects of MPA as compared with those of progesterone and dihydrotestosterone (DHT) in human breast cancer cells. A new progesterone receptor-negative, androgen receptor-positive human breast cancer cell line, designated Y-AR, was engineered and characterized. Transcription assays using a synthetic promoter/reporter construct, as well as endogenous gene expression profiling comparing progesterone, MPA and DHT, were performed in cells either lacking or containing progesterone receptor and/or androgen receptor. In progesterone receptor-positive cells, MPA was found to be an effective progestin through both progesterone receptor isoforms in transient transcription assays. Interestingly, DHT signaled through progesterone receptor type B. Expression profiling of endogenous progesterone receptor-regulated genes comparing progesterone and MPA suggested that although MPA may be a somewhat more potent progestin than progesterone, it is qualitatively similar to progesterone. To address effects of MPA through androgen receptor, expression profiling was performed comparing progesterone, MPA and DHT using Y-AR cells. These studies showed extensive gene regulatory overlap between DHT and MPA through androgen receptor and none with progesterone. Interestingly, there was no difference between pharmacological MPA and physiological MPA, suggesting that high-dose therapeutic MPA may be superfluous. /This/ comparison of the gene regulatory profiles of MPA and progesterone suggests that, for physiologic hormone replacement therapy, the actions of MPA do not mimic those of endogenous progesterone alone. ... It is possible that the increased breast cancer risk and/or the therapeutic efficacy of MPA in cancer treatment is in part mediated by androgen receptor. |
| 分子式 |
C22H32O3
|
|---|---|
| 分子量 |
344.48
|
| 精确质量 |
344.235
|
| 元素分析 |
C, 76.70; H, 9.36; O, 13.93
|
| CAS号 |
520-85-4
|
| 相关CAS号 |
Medroxyprogesterone;520-85-4;Medroxyprogesterone-d3;162462-69-3;Medroxyprogesterone-d7; 71-58-9 (acetate)
|
| PubChem CID |
10631
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
1.1±0.1 g/cm3
|
| 沸点 |
488.0±45.0 °C at 760 mmHg
|
| 熔点 |
220-223.5ºC
|
| 闪点 |
263.0±25.2 °C
|
| 蒸汽压 |
0.0±2.8 mmHg at 25°C
|
| 折射率 |
1.554
|
| LogP |
3.38
|
| tPSA |
54.37
|
| 氢键供体(HBD)数目 |
1
|
| 氢键受体(HBA)数目 |
3
|
| 可旋转键数目(RBC) |
1
|
| 重原子数目 |
25
|
| 分子复杂度/Complexity |
664
|
| 定义原子立体中心数目 |
7
|
| SMILES |
CC([C@@]1(O)CC[C@@]2([H])[C@]3([H])C[C@H](C)C4=CC(CC[C@]4(C)[C@@]3([H])CC[C@]12C)=O)=O
|
| InChi Key |
FRQMUZJSZHZSGN-HBNHAYAOSA-N
|
| InChi Code |
InChI=1S/C22H32O3/c1-13-11-16-17(20(3)8-5-15(24)12-19(13)20)6-9-21(4)18(16)7-10-22(21,25)14(2)23/h12-13,16-18,25H,5-11H2,1-4H3/t13-,16+,17-,18-,20+,21-,22-/m0/s1
|
| 化学名 |
Pregn-4-ene-3,20-dione, 17-hydroxy-6-alpha-methyl-
|
| 别名 |
Medroxyprogesterone; NSC 27408; Medroxyprogesteron; Medroxiprogesteronum; Medroxiprogesterona; Medroxyprogesteronum; Medrossiprogesterone; 17-Hydroxy-6alpha-methylprogesterone; NSC-27408; NSC27408;
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ~50 mg/mL (~145.14 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (7.26 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL 澄清 DMSO 储备液加入900 μL 玉米油中,混合均匀。 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.9029 mL | 14.5146 mL | 29.0293 mL | |
| 5 mM | 0.5806 mL | 2.9029 mL | 5.8059 mL | |
| 10 mM | 0.2903 mL | 1.4515 mL | 2.9029 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。