| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| Other Sizes |
|
| 靶点 |
5-HT1 receptor
Rizatriptan Benzoate (MK-462 Benzoate) is a selective agonist of 5-hydroxytryptamine 1B (5-HT₁B) and 1D (5-HT₁D) receptors. In radioligand binding assays, it exhibited high affinity for bovine caudate nucleus 5-HT₁B receptors (Ki = 1.6 nM) and human platelet 5-HT₁D receptors (Ki = 2.3 nM), with negligible affinity for 5-HT₁A (Ki > 1000 nM), 5-HT₂A (Ki > 1000 nM), and α₁-adrenergic receptors (Ki > 5000 nM) [1] - Rizatriptan Benzoate (MK-462 Benzoate) binds to human recombinant 5-HT₁F receptors (expressed in HEK 293 cells) with a Ki value of 15 nM, and shows no significant binding to dopamine D₂ (Ki > 10,000 nM) or histamine H₁ (Ki > 10,000 nM) receptors [2] |
|---|---|
| 体外研究 (In Vitro) |
Rizatriptan Benzoate(也称为 MK-462 Benzoate)是一种新型、有效、选择性的血清素 5-HT1B 和 5-HT1D 受体激动剂,可潜在用于治疗急性偏头痛发作。
在离体犬冠状动脉环中,Rizatriptan Benzoate (MK-462 Benzoate)(10-1000 nM)可浓度依赖性诱导收缩,IC₅₀为85 nM;1000 nM时的最大收缩幅度为60 mM KCl(去极化剂)诱导收缩的90%[1] - 在离体人基底动脉中,Rizatriptan Benzoate (MK-462 Benzoate)(100-1000 nM)可浓度依赖性收缩,1000 nM时最大收缩幅度为KCl诱导收缩的78%;在浓度高达1000 nM时,其对人隐静脉(外周血管)无收缩作用[1] - 在原代培养的大鼠皮层神经元中,用Rizatriptan Benzoate (MK-462 Benzoate)(1、5、10 μM)预处理24 h,可显著降低氧糖剥夺(OGD)诱导的乳酸脱氢酶(LDH)释放:10 μM剂量较仅OGD组使LDH释放减少58%。Western blot分析显示,10 μM剂量可使抗凋亡蛋白Bcl-2表达增加1.8倍,促凋亡蛋白Bax表达减少0.5倍[4] - 在小鼠小胶质细胞BV-2细胞中,Rizatriptan Benzoate (MK-462 Benzoate)(1、5 μM)预处理1 h,可抑制脂多糖(LPS,1 μg/mL)诱导的促炎细胞因子释放:5 μM剂量使TNF-α减少65%、IL-1β减少52%(ELISA检测),且不影响细胞活力(MTT法)[5] - 在离体大鼠三叉神经节神经元中,Rizatriptan Benzoate (MK-462 Benzoate)(100 nM)可抑制硝酸甘油(100 μM)诱导的降钙素基因相关肽(CGRP)释放,减少幅度为42%(放射免疫法RIA检测)[2] |
| 体内研究 (In Vivo) |
利扎曲普坦通过作用于血管周围三叉神经上的 5-HT(1D) 受体来阻断神经源性血管舒张,从而抑制麻醉豚鼠体内 CGRP 的释放。利扎曲普坦会引起麻醉豚鼠硬脑膜血管直径的短暂减小,并在 10 分钟内恢复到基线值。利扎曲普坦显着抑制三叉神经节高强度电刺激产生的硬脑膜血浆蛋白外渗。利扎曲普坦显着减少麻醉大鼠的电刺激硬脑膜血管舒张。利扎曲普坦苯甲酸盐显着降低正常组和模型组大鼠中脑SP mRNA水平,表明利扎曲普坦苯甲酸盐可以下调大鼠中脑SP基因表达。 Rizatriptan Benzoate 显着降低偏头痛大鼠模型中脑 PENK mRNA 表达,降低中脑甲硫脑啡肽和亮氨酸脑啡肽水平,从而减弱内源性疼痛调节系统的镇痛作用。[5]
这些研究调查了麻醉豚鼠神经源性硬脑膜血管舒张的药理学。在引入封闭的颅窗后,使用活体显微镜观察脑膜(硬脑膜)血管,并使用视频尺寸分析仪不断测量直径。在用降钙素基因相关肽(CGRP;1微克千克(-1),静脉注射)或硬脑膜局部电刺激(高达300微安)扩张硬脑膜血管之前,用内皮素-1(3微克千克(1),静脉内注射)收缩硬脑膜血管。在用CGRP受体拮抗剂CGRP((8-37))(0.3mg kg(-1),静脉注射)预处理的豚鼠中,电刺激的扩张器反应被抑制了85%,表明CGRP在该物种的神经源性硬脑膜血管舒张中起着重要作用。5-羟色胺(1B/1D)激动剂利扎曲普坦(100微克kg(-1))也阻断了神经源性硬脑膜血管舒张,估计血浆水平与患者抗偏头痛疗效所需的浓度相当Rizatriptan不能逆转CGRP诱发的硬脑膜扩张,表明其对位于支配硬脑膜血管的三叉神经感觉纤维上的突触前受体有作用。此外,选择性5-羟色胺(1D)激动剂PNU-142633(100微克千克(-1))也阻断了神经源性硬脑膜血管舒张,但5-羟色胺(1F)激动剂LY334370(3毫克千克(-1。这种机制可能是利扎曲普坦所例示的曲坦类抗偏头痛作用之一的基础,并表明豚鼠是研究神经源性硬脑膜血管舒张药理学的合适物种。1. 这些对麻醉大鼠的研究表明,使用活体显微镜观察,新型抗偏头痛药物利扎曲普坦显著减少了电刺激的硬脑膜血管舒张,但对外源性P物质或降钙素基因相关肽(CGRP)产生的硬脑膜血管直径的增加没有影响。里扎曲普坦还显著抑制了三叉神经节高强度电刺激产生的硬脑膜血浆蛋白外渗。我们认为利扎曲普坦抑制血管周围三叉神经释放感觉神经肽,以防止神经源性血管舒张和硬脑膜外渗。这些结合前抑制作用可能与利扎曲普坦的抗偏头痛作用有关。2. 本研究利用硝酸甘油诱导的偏头痛大鼠模型,通过实时定量聚合酶链反应检测苯甲酸Rizatriptan对中脑前脑啡肽和P物质基因表达的影响,并研究苯甲酸利扎曲普坦是否可以调节内源性疼痛调节系统。结果表明,苯甲酸利扎曲普坦显著降低了前脑啡肽和P物质的mRNA表达。苯甲酸利扎曲普坦可能抑制内源性疼痛调节系统的镇痛作用。3. 通过免疫组织化学染色,对清醒大鼠上矢状窦周围硬脑膜电刺激后大脑中Fos的表达进行了系统研究。Fos样免疫反应神经元主要分布在上颈脊髓、三叉神经脊髓尾侧核、中缝大核、中脑导水管周围灰质、下丘脑腹内侧核和丘脑中。经腹腔注射苯甲酸Rizatriptan预处理后,三叉神经脊束核尾侧和中缝大核中Fos样免疫反应神经元的数量减少,中脑导水管周围灰质中Fos类免疫反应神经元数量增加,下丘脑腹内侧核和丘脑中侧核保持不变。这些结果提供了形态学证据,表明上述细胞核参与了三叉神经血管性头痛的发展和维持。[4] 在硝酸甘油诱导的大鼠偏头痛模型中(10 mg/kg,腹腔注射),于硝酸甘油给药前30 min口服Rizatriptan Benzoate (MK-462 Benzoate)(1、3、10 mg/kg),可剂量依赖性减少甩头行为:10 mg/kg剂量在2 h内使甩头频率减少72%,ED₅₀为2.8 mg/kg。同时,该剂量可将异常Grooming行为评分(0-3分)从硝酸甘油组的2.7降至0.8(2 h时)[3] - 在大鼠大脑中动脉阻塞(MCAO)模型中(阻塞2 h+再灌注24 h),于再灌注后1 h静脉注射Rizatriptan Benzoate (MK-462 Benzoate)(3、10 mg/kg),可剂量依赖性减少脑梗死体积:10 mg/kg剂量使梗死体积减少58%(TTC染色),并将神经功能评分(0-5分)从MCAO组的3.8降至1.2[4] - 在小鼠热板疼痛模型中(55±0.5°C),腹腔注射Rizatriptan Benzoate (MK-462 Benzoate)(0.5、1、2 mg/kg)可延长热痛阈潜伏期:2 mg/kg剂量在给药30 min时使潜伏期从溶媒组的5.2 s延长至10.1 s,作用持续4 h[5] - 在犬三叉神经刺激模型中(50 Hz,0.2 ms脉冲,0.1 mA),于刺激前10 min静脉注射Rizatriptan Benzoate (MK-462 Benzoate)(0.1、0.3 mg/kg),可减轻神经源性炎症:0.3 mg/kg剂量在刺激后30 min使结膜充血评分(0-4分)从刺激组的4.0降至1.0[1] |
| 酶活实验 |
SYBR绿色实时定量PCR[3]
20微升反应包括10μL SYBR Premix Ex Taq™、0.4μL上游和下游引物(10μM)、0.4μL ROX参考染料、2.0μL cDNA和6.8μL dH2O。通过定量PCR处理不同浓度的质粒标准样品(1.2×103−1.2×109)拷贝/μL。每个样本均一式三份。反应条件如下:94°C预变性2分钟,94°C变性30秒,62°C退火30秒,72°C延伸30秒,共40个循环。在每个周期的退火结束时测量荧光信号,在PCR扩增过程中定义测量临界点,即与荧光信号进入背景水平以上指数增长阶段的拐点相对应的阈值周期值。以95°C持续15秒、60°C持续20秒和95°C连续15秒的模式进行熔解曲线分析。 5-HT₁B受体结合实验(牛尾状核):将牛尾状核在冰浴的50 mM Tris-HCl缓冲液(pH7.4,含4 mM CaCl₂)中匀浆,48,000 × g离心15 min。重悬膜沉淀后,取50 μg膜蛋白与[³H]-舒马曲坦(0.5 nM,选择性5-HT₁B/1D配体)及不同浓度的Rizatriptan Benzoate (MK-462 Benzoate)(10⁻¹²-10⁻⁶ M)在25°C孵育60 min。非特异性结合定义为在10 μM未标记舒马曲坦存在下的结合。反应通过预浸泡于0.1%聚乙烯亚胺的GF/B滤膜过滤终止,滤膜用冰浴缓冲液洗涤3次。采用液体闪烁光谱法计数放射性,利用Cheng-Prusoff方程计算Ki值[1] - 5-HT₁D受体结合实验(人血小板):洗涤人血小板后,在上述Tris-HCl缓冲液中匀浆,48,000 × g离心15 min。取100 μg膜蛋白与[³H]-LSD(0.3 nM)及Rizatriptan Benzoate(10⁻¹²-10⁻⁶ M)在25°C孵育60 min。非特异性结合用10 μM Metergoline确定,过滤和放射性计数步骤同上[1] - 5-HT₁F受体结合实验(人重组HEK 293细胞):将稳定表达人5-HT₁F受体的HEK 293细胞在冰浴的25 mM HEPES缓冲液(pH7.4,含10 mM MgCl₂)中匀浆,50,000 × g离心15 min。取75 μg膜蛋白与[³H]-5-HT(1 nM)及Rizatriptan Benzoate(10⁻¹¹-10⁻⁶ M)在25°C孵育90 min。非特异性结合用10 μM未标记5-HT定义,过滤后计数放射性[2] |
| 细胞实验 |
原代大鼠皮层神经元OGD实验:从新生Sprague-Dawley大鼠(1-3日龄)分离皮层神经元,用0.25%胰蛋白酶消化15 min,以1×10⁵个细胞/孔接种于多聚-L-赖氨酸包被的96孔板。用含10%胎牛血清(FBS)的DMEM培养基培养7天。OGD处理前,用Rizatriptan Benzoate (MK-462 Benzoate)(1、5、10 μM)预处理细胞24 h。OGD通过更换为无糖Earle's平衡盐溶液(EBSS)并置于95%N₂/5%CO₂培养箱中4 h诱导。OGD后,用正常培养基再孵育24 h。收集上清液检测LDH活性,细胞活力计算为(实验组LDH-正常组LDH)/(OGD组LDH-正常组LDH)×100%[4]
- BV-2细胞因子释放实验:将小鼠小胶质细胞BV-2以5×10⁴个细胞/孔接种于24孔板,用含10%FBS的DMEM培养至80%汇合。用Rizatriptan Benzoate (MK-462 Benzoate)(1、5 μM)预处理细胞1 h,再用LPS(1 μg/mL)刺激24 h。收集培养上清液,采用夹心ELISA试剂盒检测TNF-α和IL-1β浓度,按试剂盒说明书操作,在450 nm处读取吸光度[5] - 皮层神经元凋亡蛋白Western blot实验:OGD/再灌注后,用含蛋白酶抑制剂的RIPA缓冲液裂解皮层神经元。取30 μg总蛋白进行12%SDS-PAGE电泳,转移至PVDF膜,4°C下用Bax、Bcl-2及β-actin(内参)一抗孵育过夜。膜与HRP标记的二抗室温孵育1 h,ECL试剂显色,ImageJ软件定量条带灰度值[4] |
| 动物实验 |
In preliminary experiments it was found that, following introduction of the cranial window, the dural blood vessels typically were observed to be maximally dilated, so that electrical stimulation of the cranial window produced little if any increase in diameter. It was therefore necessary to preconstrict the dural vessels with intravenously administered endothelin-1 (ET-1, 3 μg kg−1) which produced an approximate 50% reduction in dural blood vessel diameter (unpublished observations). Following administration of endothelin-1 (3 μg kg−1, i.v.) dural vasodilation was reliably evoked approximately 3 min later by intravenous rat-αCGRP (1 μg kg−1) or electrical stimulation of the cranial window (250–300 μA, 5-Hz, 1 ms for 10 s) and expressed as percentage increase in dural blood vessel diameter±s.e.mean from baseline. Rizatriptan benzoate (0.01–1 mg kg−1), PNU142,633 (0.01–1 mg kg−1) or LY334370 (3 mg kg−1) were administered intravenously 12 min before administration of ET-1 whereas human-αCGRP(8–37) (0.3 mg kg−1) was given 2 min prior to ET-1. Statistical comparisons between drug and vehicle treated rats were made by t-tests (BMDP statistical software) and P<0.05 was considered significant. [1]
Migraine model establishment and interventions [3] Rizatriptan benzoate control and treatment groups were intragastrically perfused with rizatriptan benzoate, 1 mg/kg per day (according to the adult daily dose), and normal control and model groups were perfused with normal saline 2 mL per day. After 7 days, nitroglycerin (10 mg/kg) was subcutaneously injected into the buttocks of the rizatriptan benzoate treatment and model groups to induce migraine. Normal saline (2 mL/kg) was injected into the normal control and rizatriptan benzoate control groups. Rat Migraine Model (Nitroglycerin-Induced): Male Sprague-Dawley rats (200-220 g) were randomly divided into 4 groups (n=8/group): Vehicle (0.5% methylcellulose, p.o.), Rizatriptan Benzoate 1 mg/kg (p.o.), 3 mg/kg (p.o.), 10 mg/kg (p.o.). Thirty minutes after drug administration, rats received nitroglycerin (10 mg/kg, i.p.) to induce migraine-like symptoms. Rats were placed in a transparent observation cage, and head-scratching frequency was recorded every 10 min for 2 h. Grooming behavior was scored at 2 h (0 = normal, 3 = severe abnormal grooming) [3] - Rat MCAO Model: Male Sprague-Dawley rats (280-320 g) were anesthetized with isoflurane. The middle cerebral artery (MCA) was occluded using a nylon monofilament (0.26 mm diameter) inserted via the external carotid artery. After 2 h of occlusion, the filament was withdrawn to allow reperfusion. One hour after reperfusion, rats received Rizatriptan Benzoate (MK-462 Benzoate) (3, 10 mg/kg, i.v., dissolved in normal saline, volume 10 mL/kg) or vehicle (normal saline). Twenty-four hours later, rats were euthanized, and brains were sectioned into 2-mm slices. Slices were stained with 2% TTC at 37°C for 20 min, and infarct volume was measured using ImageJ. Neurological function was scored blindly (0 = normal, 5 = death) [4] - Mouse Hot-Plate Assay: Female ICR mice (20-22 g) were acclimated to the hot-plate apparatus (55±0.5°C) for 3 days. Basal nociceptive latency (time to paw withdrawal) was measured (cut-off time 30 s). Mice were randomly divided into 4 groups (n=10/group): Vehicle (normal saline, i.p.), Rizatriptan Benzoate 0.5 mg/kg (i.p.), 1 mg/kg (i.p.), 2 mg/kg (i.p.). Latency was measured at 30, 60, 120, and 240 min post-administration [5] - Canine Trigeminal Stimulation Model: Male beagles (10-12 kg) were anesthetized with pentobarbital. The trigeminal ganglion was exposed surgically, and electrical stimulation (50 Hz, 0.2 ms pulse width, 0.1 mA) was applied for 10 min. Ten minutes before stimulation, Rizatriptan Benzoate (MK-462 Benzoate) (0.1, 0.3 mg/kg, i.v., dissolved in normal saline) or vehicle was administered. Conjunctival hyperemia was scored blindly at 30 min post-stimulation (0 = no hyperemia, 4 = severe hyperemia) [1] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Rizatriptan is readily absorbed (approximately 90%) following oral administration; however, the mean oral absolute bioavailability of the rizatriptan tablet is about 45%, owing to extensive first-pass metabolism. The Tmax is approximately one to 1.5 hours. The presence of a migraine headache did not appear to affect the absorption or pharmacokinetics of rizatriptan. Food has no significant effect on the bioavailability of rizatriptan but delays the time to reach peak concentration by an hour. In clinical trials, rizatriptan was administered without regard to food. The bioavailability and Cmax of rizatriptan were similar following the administration of rizatriptan tablets and rizatriptan orally disintegrating tablets. Still, the absorption rate is somewhat slower with orally disintegrating tablets, with Tmax delayed by up to 0.7 hours. The AUC of rizatriptan is approximately 30% higher in females than males. No accumulation occurred on multiple dosing. Following oral administration of a single 10 mg of 14 C-rizatriptan, the total radioactivity of the administered dose recovered over 120 hours in urine and feces was 82% and 12%, respectively. Following oral administration of 14C-rizatriptan, rizatriptan accounted for about 17% of circulating plasma radioactivity. Approximately 14% of an oral dose is excreted in urine as unchanged rizatriptan, while 51% is excreted as indole acetic acid metabolite, indicating substantial first-pass metabolism. The mean volume of distribution is approximately 140 L in male subjects and 110 L in female subjects. An early study involving healthy subject reported plasma clearance of 1042 mL/min in males and 821 mL/min in females; however, this difference in clearance rates is not thought to be clinically relevant. Metabolism / Metabolites Rizatriptan primarily undergoes oxidative deamination mediated by monoamine oxidase-A (MAO-A) to form triazolomethyl-indole-3-acetic acid, which is not pharmacologically active. N-monodesmethyl-rizatriptan is a minor metabolite with a pharmacological activity comparable to the parent compound's. Plasma concentrations of N-monodesmethyl-rizatriptan are approximately 14% of those of the parent compound, which is eliminated at a similar rate. Other pharmacologically inactive minor metabolites include the N-oxide, the 6-hydroxy compound, and the sulfate conjugate of the 6-hydroxy metabolite. Rizatriptan is metabolized by monoamine oxidase A isoenzyme (MAO-A) to an inactive indole acetic acid metabolite. In addition, several other inactive metabolites are formed. An active metabolite, N-monodesmethyl-rizatriptan, with pharmacological activity similar to that of the parent compound has been identified in small concentrations (14%) in the plasma. Route of Elimination: Approximately 14% of an oral dose is excreted in urine as unchanged rizatriptan while 51% is excreted as indole acetic acid metabolite, indicating substantial first pass metabolism. Half Life: 2-3 hours Biological Half-Life The plasma half-life of rizatriptan in males and females ranges from two to three hours. In male Sprague-Dawley rats, oral administration of Rizatriptan Benzoate (MK-462 Benzoate) (2 mg/kg) resulted in a peak plasma concentration (Cmax) of 89 ng/mL, time to Cmax (Tmax) of 0.8 h, and terminal half-life (t₁/₂) of 2.1 h. Absolute oral bioavailability was 63%. Intravenous (i.v.) administration (1 mg/kg) showed a plasma clearance of 15.2 mL/min/kg and volume of distribution at steady state (Vss) of 1.9 L/kg. Within 72 h, 78% of the dose was excreted in urine (35% as parent drug, 43% as inactive metabolites) [1] - In male beagles, oral administration of Rizatriptan Benzoate (MK-462 Benzoate) (1 mg/kg) had a Cmax of 52 ng/mL, Tmax of 1.0 h, and t₁/₂ of 2.8 h, with an oral bioavailability of 58%. Intravenous administration (0.5 mg/kg) showed a clearance of 12.8 mL/min/kg and Vss of 2.3 L/kg [1] - In healthy human volunteers (n=6), oral administration of Rizatriptan Benzoate (MK-462 Benzoate) (5 mg) resulted in a Cmax of 18 ng/mL, Tmax of 1.2 h, and t₁/₂ of 2.5 h. Absolute oral bioavailability was 60%. Plasma protein binding rate (measured via ultrafiltration) was 14% over a concentration range of 10-1000 ng/mL. The drug is primarily metabolized via hepatic CYP3A4-mediated N-demethylation, producing inactive metabolites [2] |
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation Breastmilk levels of rizatriptan are low and the half-life in milk is relatively short. Amounts ingested by the infant are small and unlikely to affect the nursing infant. Painful, burning nipples and breast pain have been reported after doses of sumatriptan and other triptans. This has occasionally been accompanied by a decrease in milk production. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk A review of four European adverse reaction databases found 26 reported cases of, painful, burning nipples, painful breasts, breast engorgement and/or painful milk ejection in women who took a triptan while nursing. Pain was sometimes intense and occasionally led to decreased milk production. Pain generally subsided with time as the drug was eliminated. The authors proposed that triptans may cause vasoconstriction of the arteries in the breast, nipples, and the arteries surrounding the alveoli and milk ducts, causing a painful sensation and a painful milk ejection reflex. Protein Binding Rizatriptan is minimally bound (14%) to plasma proteins. In acute toxicity studies in male Sprague-Dawley rats, the LD₅₀ of Rizatriptan Benzoate (MK-462 Benzoate) was >200 mg/kg (i.p.) and >500 mg/kg (p.o.). No mortality, ataxia, or convulsions were observed within 72 h of administration [1] - In a 28-day repeated oral toxicity study in male Sprague-Dawley rats (doses: 10, 30, 100 mg/kg/day), the 100 mg/kg group showed a slight reduction in body weight gain (8% lower than vehicle controls), but no significant changes in serum alanine transaminase (ALT) or aspartate transaminase (AST). Serum creatinine and urea (renal function markers) were within normal ranges. No histopathological abnormalities were found in the liver, kidney, or brain. The no-observed-adverse-effect level (NOAEL) was 30 mg/kg/day [3] - In vitro hepatotoxicity testing using human hepatocytes showed no significant increase in LDH release or decrease in cell viability (MTT assay) after 24 h exposure to Rizatriptan Benzoate (MK-462 Benzoate) at concentrations up to 100 μM [2] - No significant drug-drug interactions were observed when Rizatriptan Benzoate (MK-462 Benzoate) (10 mg/kg, p.o.) was co-administered with phenelzine (a monoamine oxidase inhibitor, 5 mg/kg, p.o.) in rats (no abnormal blood pressure or heart rate changes). Co-administration with propranolol (a β-blocker, 10 mg/kg, p.o.) did not alter the pharmacokinetic parameters of Rizatriptan Benzoate (Cmax and t₁/₂ changed by <10%) [1] |
| 参考文献 | |
| 其他信息 |
Rizatriptan benzoate is a member of tryptamines.
Rizatriptan Benzoate is the benzoate salt form of rizatriptan, a member of the triptan class agents with anti-migraine property. Rizatriptan benzoate selectively binds to and activates serotonin (5-HT) 1B receptors expressed in intracranial arteries, and to 5-HT 1D receptors located on peripheral trigeminal sensory nerve terminals in the meninges and central terminals in brain stem sensory nuclei. Receptor binding results in constriction of cranial vessels and inhibition of nociceptive transmission, thereby providing relief of migraine headaches. Rizatriptan benzoate may also relief migraine headaches by inhibition of pro-inflammatory neuropeptide release. See also: Rizatriptan (has active moiety). The present studies have demonstrated that electrical stimulation of the dura mater evokes neurogenic vasodilation of preconstricted dural blood vessels in anaesthetized guinea-pigs and that the dilation is mediated by CGRP release from trigeminal fibres. In addition neurogenic, but not CGRP-evoked dural vasodilation, was also blocked by rizatriptan at clinically relevant doses via an action on presynaptic 5-HT1D receptors, since neurogenic dural vasodilation was also blocked by the 5-HT1D agonist PNU142,633 but not by the 5-HT1F agonist LY334370. The present studies suggest that the guinea-pig may be an appropriate species in which to investigate the pharmacology of neurogenic dural vasodilation providing data that can be extrapolated to man.[1] Opioid peptides and opioid receptor agonists exert strong analgesic effects by inhibiting neuronal pain-evoked discharges and activating the pain modulatory descending inhibitory system. Enkephalin is classified into two forms according to its structure: met-enkephalin and leu-enkephalin. They are derived from a single precursor, namely, PENK. The results of the present study revealed no significant difference in midbrain PENK expression levels between model and normal control groups, indicating that migraine does not directly influence midbrain PENK expression. However, the effects of migraine on opioid peptide expression require further study. Rizatriptan benzoate significantly reduced midbrain PENK mRNA expression, decreasing the levels of midbrain met-enkephalin and leu-enkephalin, and thereby weakening the analgesic effects of the endogenous pain modulatory system. In addition, SP has been shown to stimulate enkephalin release from the periaqueductal gray. In the present study, rizatriptan benzoate reduced SP and PENK mRNA expression in the midbrain. However, whether there is a correlation between these two reductions remains to be fully investigated. In conclusion, rizatriptan benzoate decreased expression of the mRNAs for SP and PENK in the midbrain, possibly inhibiting the analgesic effects of the endogenous pain modulatory system.[3] Rizatriptan Benzoate (MK-462 Benzoate) is a second-generation triptan drug developed for the acute treatment of migraine. Compared to first-generation triptans (e.g., sumatriptan), it has higher oral bioavailability (60-63% vs. ~14% for sumatriptan) and faster onset of action (Tmax ~1 h vs. ~2 h for sumatriptan) [1] - The mechanism of action of Rizatriptan Benzoate (MK-462 Benzoate) involves two key effects: 1) Agonism of 5-HT₁B receptors on cerebral blood vessels, constricting abnormally dilated vessels associated with migraine; 2) Agonism of 5-HT₁D receptors on trigeminal nerve terminals, inhibiting the release of pro-inflammatory neuropeptides (e.g., CGRP) and reducing neurogenic inflammation [1] - Preclinical studies in migraine models (e.g., nitroglycerin-induced rat model) showed that the effective oral dose range of Rizatriptan Benzoate (MK-462 Benzoate) (1-10 mg/kg) is consistent with the clinical recommended dose (5-10 mg for humans), supporting its translational potential [3] - Beyond migraine treatment, Rizatriptan Benzoate (MK-462 Benzoate) exhibited neuroprotective effects in a rat MCAO model (cerebral ischemia), likely via inhibiting neuronal apoptosis (upregulating Bcl-2 and downregulating Bax), suggesting potential for expanding its therapeutic indications [4] - In vitro studies showed Rizatriptan Benzoate (MK-462 Benzoate) inhibits microglial activation and pro-inflammatory cytokine release, indicating an additional anti-inflammatory mechanism that may contribute to relieving migraine-related pain [5] |
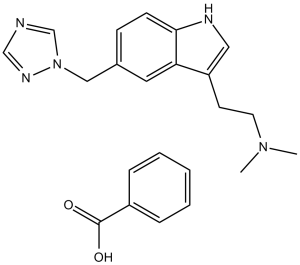
| 分子式 |
C22H25N5O2
|
|
|---|---|---|
| 分子量 |
391.47
|
|
| 精确质量 |
391.2
|
|
| 元素分析 |
C, 67.50; H, 6.44; N, 17.89; O, 8.17
|
|
| CAS号 |
145202-66-0
|
|
| 相关CAS号 |
Rizatriptan-d6 benzoate; 1216984-85-8; 144034-80-0; 159776-67-7 (sulfate)
|
|
| PubChem CID |
77997
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 密度 |
1.21g/cm3
|
|
| 沸点 |
504.8ºC at 760mmHg
|
|
| 熔点 |
178-180°C
|
|
| 闪点 |
259.1ºC
|
|
| 蒸汽压 |
2.58E-10mmHg at 25°C
|
|
| 折射率 |
1.645
|
|
| LogP |
3.296
|
|
| tPSA |
87.04
|
|
| 氢键供体(HBD)数目 |
2
|
|
| 氢键受体(HBA)数目 |
5
|
|
| 可旋转键数目(RBC) |
6
|
|
| 重原子数目 |
29
|
|
| 分子复杂度/Complexity |
412
|
|
| 定义原子立体中心数目 |
0
|
|
| SMILES |
O([H])C(C1C([H])=C([H])C([H])=C([H])C=1[H])=O.N1([H])C([H])=C(C([H])([H])C([H])([H])N(C([H])([H])[H])C([H])([H])[H])C2C([H])=C(C([H])([H])N3C([H])=NC([H])=N3)C([H])=C([H])C1=2
|
|
| InChi Key |
JPRXYLQNJJVCMZ-UHFFFAOYSA-N
|
|
| InChi Code |
InChI=1S/C15H19N5.C7H6O2/c1-19(2)6-5-13-8-17-15-4-3-12(7-14(13)15)9-20-11-16-10-18-20;8-7(9)6-4-2-1-3-5-6/h3-4,7-8,10-11,17H,5-6,9H2,1-2H3;1-5H,(H,8,9)
|
|
| 化学名 |
benzoic acid;N,N-dimethyl-2-[5-(1,2,4-triazol-1-ylmethyl)-1H-indol-3-yl]ethanamine
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (6.39 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (6.39 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (6.39 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: 50 mg/mL (127.72 mM) in PBS (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶. 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.5545 mL | 12.7724 mL | 25.5447 mL | |
| 5 mM | 0.5109 mL | 2.5545 mL | 5.1089 mL | |
| 10 mM | 0.2554 mL | 1.2772 mL | 2.5545 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
A Study of the efficacy and safety of Rizatriptan 10 mg PRD in the treatment of acute migraine in patients with non satisfactory response to previous pharmacologic treatment
CTID: null
Phase: Phase 4 Status: Ongoing
Date: 2007-06-22
 |
|---|
 |