| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| Other Sizes |
|
| 靶点 |
FKBP12; calcineurin; macrocyclic lactone
|
||
|---|---|---|---|
| 体外研究 (In Vitro) |
NO合酶的激活、IL-2基因转录、细胞脱粒和细胞凋亡属于钙依赖性过程,可被他克莫司一水合物(FK506一水合物、富士霉素一水合物、FR900506一水合物)抑制。通过与激素受体复合物内的 FKBP 结合并抑制降解,他克莫司还可以增强黄体酮和糖皮质激素的作用。该药物可能会以类似于 CsA 的方式增加 TGFβ-1 基因表达。他克莫司可抑制 T 细胞受体连接后的 T 细胞生长[1]。用低剂量他克莫司(FK506,10 μg/L)处理MH3924A细胞并不会对其增殖能力产生太大影响(P=0.135)。用浓度增加的他克莫司 (100-1,000 μg/L) 处理可显着增加 (P<0.01) MH3924A 细胞的增殖。 AMD3100治疗在任何剂量(10、50或100μg/L)下似乎都不影响MH3924A细胞的增殖(P>0.05)。然而,不同剂量的AMD3100与100 μg/L他克莫司联用时,MH3924A细胞的体外增殖能力增强(P<0.01)[3]。
|
||
| 体内研究 (In Vivo) |
在第 10 天至第 16 或第 23 天给予右旋糖酐硫酸钠 (DSS) 治疗的小鼠服用他克莫司,以研究对结肠炎进展和维持的治疗效果。与正常动物相比,接受 DSS 处理的对照组在第 17 天和第 24 天时表现出结肠长度大幅缩短和结肠重量增加。此外,对照组每单位长度的结肠重量是正常动物的两倍以上组的。虽然与对照组相比,接受 DSS 治疗的大鼠中,7 或 14 天的他克莫司治疗显着抑制了每单位长度结肠重量的增加,但这种治疗实际上并未恢复结肠缩短。此外,如抑制百分比(59% vs. 28%)所示,他克莫司对每单位长度结肠重量增加的抑制作用在 14 天的治疗中比 7 天的治疗更明显[4]。
|
||
| 酶活实验 |
他克莫司 (FK506) 抑制钙依赖性事件,例如 IL-2 基因转录、NO 合酶激活、细胞脱颗粒和细胞凋亡。他克莫司还通过与激素受体复合物中包含的 FKBP 结合,防止降解,从而增强糖皮质激素和黄体酮的作用。该药物可以以与 CsA 类似的方式增强 TGFβ-1 基因的表达。他克莫司抑制 T 细胞受体连接后的 T 细胞增殖。低浓度他克莫司(FK506,10 μg/L)处理对MH3924A细胞的增殖没有显着影响(P=0.135)。高浓度他克莫司(100-1,000 μg/L)处理后,MH3924A细胞增殖显着增强(P<0.01)。但不同浓度的AMD3100与100 μg/L他克莫司合用时,MH3924A细胞体外增殖能力增强(P<0.01)。
|
||
| 细胞实验 |
他克莫司,原名FK506,是一种具有免疫抑制特性的大环内酯类抗生素。尽管在结构上与环孢菌素A(CsA)无关,但其作用方式相似。它主要通过损伤靶细胞中的基因表达来发挥作用。他克莫司与亲免疫蛋白FK506结合蛋白(FKBP)结合。这种复合物抑制钙调神经磷酸酶。该药物抑制钙依赖性事件,如白细胞介素-2基因转录、一氧化氮合酶激活、细胞脱颗粒和凋亡。他克莫司还通过与激素受体复合物中含有的FKBP结合来增强糖皮质激素和黄体酮的作用,防止降解。该试剂可以以类似于CsA所证明的方式增强转化生长因子β-1基因的表达。他克莫司抑制了T细胞受体连接后的T细胞增殖。与2型T辅助细胞相比,1型T辅助电池似乎优先受到抑制。T细胞介导的细胞毒性受损。抑制这些功能所必需的T细胞衍生生长因子间接影响B细胞生长和抗体产生。抗原呈递似乎得以避免。他克莫司影响的分子事件仍在继续被发现[1]。
|
||
| 动物实验 |
|
||
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Absorption of tacrolimus from the gastrointestinal tract after oral administration is incomplete and variable. The absolute bioavailability in adult kidney transplant patients is 17±10%; in adults liver transplant patients is 22±6%; in healthy subjects is 18±5%. The absolute bioavailability in pediatric liver transplant patients was 31±24%. Tacrolimus maximum blood concentrations (Cmax) and area under the curve (AUC) appeared to increase in a dose-proportional fashion in 18 fasted healthy volunteers receiving a single oral dose of 3, 7, and 10 mg. When given without food, the rate and extent of absorption were the greatest. The time of the meal also affected bioavailability. When given immediately after a meal, mean Cmax was reduced 71%, and mean AUC was reduced 39%, relative to the fasted condition. When administered 1.5 hours following the meal, mean Cmax was reduced 63%, and mean AUC was reduced 39%, relative to the fasted condition. In man, less than 1% of the dose administered is excreted unchanged in urine. When administered IV, fecal elimination accounted for 92.6±30.7%, urinary elimination accounted for 2.3±1.1%. 2.6 ± 2.1 L/kg [pediatric liver transplant patients] 1.07 ± 0.20 L/kg [patients with renal impairment, 0.02 mg/kg/4 hr dose, IV] 3.1 ± 1.6 L/kg [Mild Hepatic Impairment, 0.02 mg/kg/4 hr dose, IV] 3.7 ± 4.7 L/kg [Mild Hepatic Impairment, 7.7 mg dose, PO] 3.9 ± 1.0 L/kg [Severe hepatic impairment, 0.02 mg/kg/4 hr dose, IV] 3.1 ± 3.4 L/kg [Severe hepatic impairment, 8 mg dose, PO] 0.040 L/hr/kg [healthy subjects, IV] 0.172 ± 0.088 L/hr/kg [healthy subjects, oral] 0.083 L/hr/kg [adult kidney transplant patients, IV] 0.053 L/hr/kg [adult liver transplant patients, IV] 0.051 L/hr/kg [adult heart transplant patients, IV] 0.138 ± 0.071 L/hr/kg [pediatric liver transplant patients] 0.12 ± 0.04 (range 0.06-0.17) L/hr/kg [pediatric kidney transplant patients] 0.038 ± 0.014 L/hr/kg [patients with renal impairment, 0.02 mg/kg/4 hr dose, IV] 0.042 ± 0.02 L/hr/kg [Mild Hepatic Impairment, 0.02 mg/kg/4 hr dose, IV] 0.034 ± 0.019 L/hr/kg [Mild Hepatic Impairment, 7.7 mg dose, PO] 0.017 ± 0.013 L/hr/kg [Severe hepatic impairment, 0.02 mg/kg/4 hr dose, IV] 0.016 ± 0.011 L/hr/kg [Severe hepatic impairment, 8 mg dose, PO] The aim of this study was to assess tacrolimus levels in breast milk and neonatal exposure during breastfeeding. An observational cohort study was performed in two tertiary referral high-risk obstetric medicine clinics. Fourteen women taking tacrolimus during pregnancy and lactation, and their 15 infants, 11 of whom were exclusively breast-fed, were assessed. Tacrolimus levels were analyzed by liquid chromatography-tandem mass spectrometry. Samples from mothers and cord blood were collected at delivery and from mothers, infants, and breast milk postnatally where possible. All infants with serial sampling had a decline in tacrolimus level, which was approximately 15% per day (ratio of geometric mean concentrations 0.85; 95% confidence interval, 0.82-0.88; P<0.001). Breast-fed infants did not have higher tacrolimus levels compared with bottle-fed infants (median 1.3 ug/L [range, 0.0-4.0] versus 1.0 ug/L (range, 0.0-2.3), respectively; P=0.91). Maximum estimated absorption from breast milk is 0.23% of maternal dose (weight-adjusted). Ingestion of tacrolimus by infants via breast milk is negligible. Breastfeeding does not appear to slow the decline of infant tacrolimus levels from higher levels present at birth. Maternal and umbilical cord (venous and arterial) samples were obtained at delivery from eight solid organ allograft recipients to measure tacrolimus and metabolite bound and unbound concentrations in blood and plasma. Tacrolimus pharmacokinetics in breast milk were assessed in one subject. Mean (+ or - SD) tacrolimus concentrations at the time of delivery in umbilical cord venous blood (6.6 + or - 1.8 ng ml(-1)) were 71 + or - 18% (range 45-99%) of maternal concentrations (9.0 + or - 3.4 ng ml(-1)). The mean umbilical cord venous plasma (0.09 + or - 0.04 ng ml(-1)) and unbound drug concentrations (0.003 + or - 0.001 ng ml(-1)) were approximately one fifth of the respective maternal concentrations. Arterial umbilical cord blood concentrations of tacrolimus were 100 + or - 12% of umbilical venous concentrations. In addition, infant exposure to tacrolimus through the breast milk was less than 0.3% of the mother's weight-adjusted dose. Differences between maternal and umbilical cord tacrolimus concentrations may be explained in part by placental P-gp function, greater red blood cell partitioning and higher haematocrit levels in venous cord blood. Ten colostrum samples were obtained from six women in the immediate postpartum period (0-3 days) with a mean drug concentration of 0.79 ng/mL (range 0.3-1.9 ng/mL). The median milk:maternal plasma ratio was 0.5. The plasma protein binding of tacrolimus is approximately 99% and is independent of concentration over a range of 5-50 ng/mL. Tacrolimus is bound mainly to albumin and alpha-1-acid glycoprotein, and has a high level of association with erythrocytes. The distribution of tacrolimus between whole blood and plasma depends on several factors, such as hematocrit, temperature at the time of plasma separation, drug concentration, and plasma protein concentration. In a US study, the ratio of whole blood concentration to plasma concentration averaged 35 (range 12 to 67). There was no evidence based on blood concentrations that tacrolimus accumulates systemically upon intermittent topical application for periods of up to 1 year. As with other topical calcineurin inhibitors, it is not known whether tacrolimus is distributed into the lymphatic system. For more Absorption, Distribution and Excretion (Complete) data for Tacrolimus (9 total), please visit the HSDB record page. Metabolism / Metabolites The metabolism of tacrolimus is predominantly mediated by CYP3A4 and secondarily by CYP3A5. Tacrolimus is metabolized into 8 metabolites: 13-demethyl tacrolimus, 31-demethyl tacrolimus, 15-demethyl tacrolimus, 12-hydroxy tacrolimus, 15,31-didemethyl tacrolimus, 13,31-didemethyl tacrolimus, 13,15-didemethyl tacrolimus, and a final metabolite involving O-demethylation and the formation of a fused ring. The major metabolite identified in incubations with human liver microsomes is 13-demethyl tacrolimus. In in vitro studies, a 31-demethyl metabolite has been reported to have the same activity as tacrolimus. Tacrolimus is extensively metabolized by the mixed-function oxidase system, primarily the cytochrome P-450 system (CYP3A). A metabolic pathway leading to the formation of 8 possible metabolites has been proposed. Demethylation and hydroxylation were identified as the primary mechanisms of biotransformation in vitro. The major metabolite identified in incubations with human liver microsomes is 13-demethyl tacrolimus. In in vitro studies, a 31-demethyl metabolite has been reported to have the same activity as tacrolimus. Fk_506 has known human metabolites that include 13-O-Desmethyltacrolimus and 15-O-Desmethyltacrolimus. Biological Half-Life The elimination half life in adult healthy volunteers, kidney transplant patients, liver transplants patients, and heart transplant patients are approximately 35, 19, 12, 24 hours, respectively. The elimination half life in pediatric liver transplant patients was 11.5±3.8 hours, in pediatric kidney transplant patients was 10.2±5.0 (range 3.4-25) hours. In a mass balance study of IV administered radiolabeled tacrolimus to 6 healthy volunteers, ... the elimination half-life based on radioactivity was 48.1+ or - 15.9 hours whereas it was 43.5 + or- 11.6 hours based on tacrolimus concentrations. ... When administered PO, the elimination half-life based on radioactivity was 31.9 + or- 10.5 hours whereas it was 48.4 + or - 12.3 hours based on tacrolimus concentrations ... . ... A case of tacrolimus toxicity in a non-transplant patient /is presented/. ... /The/ patient's tacrolimus dose was 2.1 mg/kg/day for 4 days (therapeutic 0.03 to 0.05 mg/kg/day). Her tacrolimus elimination half-life was 16.5 hours, compared to a mean half-life in healthy volunteers of 34.2 +/- 7.7 hours. ... |
||
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation Limited data indicate that amounts of systemically administered tacrolimus are low in breastmilk and probably do not adversely affect the breastfed infant. United States and European experts and guidelines consider tacrolimus to be probably safe to use during breastfeeding. Exclusively breastfed infants should be monitored if this drug is used during lactation, possibly including measurement of serum levels to rule out toxicity if there is a concern. Topical tacrolimus presents a low risk to the nursing infant because it is poorly absorbed after topical application and peak blood concentrations are less than 2 mcg/L in most patients. Ensure that the infant's skin does not come into direct contact with the areas of skin that have been treated. Current guidelines allow topical tacrolimus to be applied to the nipples just after nursing, with the nipples cleaned gently before nursing. Only water-miscible cream or gel products should be applied to the breast or nipple because ointments may expose the infant to high levels of mineral paraffins via licking, so pimecrolimus cream may be preferable to tacrolimus ointment for nipple application. ◉ Effects in Breastfed Infants One infant was exclusively breastfed during maternal tacrolimus therapy throughout gestation to at least 2.5 months of age at which time the infant was developing normally physically and neurologically. An ultrasound examination of the infant's thymus was normal. The National Transplantation Pregnancy Registry reported data gathered from 1991 to 2011 on mothers who breastfed their infants following organ transplantation. A total of 68 mothers with transplants (mostly kidney or liver) used tacrolimus while breastfeeding a total of 83 infants. Duration of nursing ranged from 1 week to 1.5 years and follow-up of the children ranged from weeks to 16 years. There were no reports of problems in any of the infants or children. As of December 2013, a total of 92 mothers had breastfed 125 infants for as long as 26 months with no apparent adverse effects in infants. The breastfed infants of six women who took tacrolimus during pregnancy for organ transplantation were breastfed (4 exclusive, 2 partial) for 45 to 180 days and followed for periods of 2 to 30 months. The mothers' mean daily tacrolimus dosage during breastfeeding was 9.6 mg daily (range 4.5 to 15 mg daily). Four mothers were also taking azathioprine 100 to 150 mg daily, one was taking diltiazem, and one was taking prednisolone 15 mg and aspirin 75 mg daily. None of the infants had any clear tacrolimus-related side effects, although one had transient thrombocytosis that resolved despite continued breastfeeding. Developmental milestones were normal and no pattern of infections was noted. Two mothers with systemic lupus erythematosus were reported who took tacrolimus 3 mg daily during pregnancy and lactation as well as prednisolone 30 or 40 mg daily. Three years after birth, both children were healthy. The durations of lactation were not stated. In a case series of women who had liver transplants over a 25-year period, one woman breastfed (extent not stated) her infant while taking tacrolimus. No neonatal complications were noted. A mother with a liver transplant was maintained on belatacept 10 mg/kg monthly, slow-release tacrolimus (Envarsus and Veloxis) 2 mg daily, azathioprine 25 mg daily, and prednisone 2.5 mg daily. She breastfed her infant for a year (extent not stated). The infant’s growth and cognitive milestones were normal. An Australian case series reported 3 women with heart transplants who had a total of 5 infants, all of whom were breastfed (extent not stated) during maternal tacrolimus therapy. Daily dosages ranged from 3 to 13 mg daily. No adverse infant effects were reported up to the times of discharge. A woman with rheumatoid arthritis refractory to etanercept took sarilumab 200 mg every two weeks during pregnancy until 37 weeks of gestation. She was also taking prednisolone 10 mg and tacrolimus 3 mg daily. She delivered a healthy infant at 38 weeks of gestation and breastfed her infant. Prednisolone was continued postpartum, tacrolimus was restarted at 7 days postpartum, and sarilumab was restarted at 28 days postpartum. The mother continued to breastfeed until 6 months postpartum. The infant was vaccinated with multiple live vaccines after reaching six months old, including the Bacille-Calmette-Guerin vaccine, with no adverse effects. A woman with a heart transplant took tacrolimus alone throughout pregnancy and postpartum while breastfeeding her infant (extent not stated) for one year. The child had normal weight gain, normal motor development, and no signs of metabolic disorders or significant infections. The age of the infant at evaluation was not stated. ◉ Effects on Lactation and Breastmilk A study in renal transplant patients who were on a tacrolimus-based immunosuppression regimen found that women’s median serum prolactin levels were 14.4 mcg/L compared with women who were not taking tacrolimus (17.6 mcg/L). The difference was statistically significant. Median serum testosterone levels (0.121 vs 0.137 mcg/L) and serum cortisol levels (82.5 vs 105 mg/L) were also significantly lower in the tacrolimus group. The reduced prolactin may be caused by inhibition of the transcription of the human prolactin gene. Not all studies have found a reduction in serum prolactin with tacrolimus. The prolactin level in a mother with established lactation may not affect her ability to breastfeed. |
||
| 参考文献 |
|
||
| 其他信息 |
Tacrolimus hydrate is a hydrate that is the monohydrate form of tacrolimus. It has a role as an immunosuppressive agent. It contains a tacrolimus (anhydrous).
A macrolide isolated from the culture broth of a strain of Streptomyces tsukubaensis that has strong immunosuppressive activity in vivo and prevents the activation of T-lymphocytes in response to antigenic or mitogenic stimulation in vitro. See also: Tacrolimus (annotation moved to). Therapeutic Uses Immunosuppressive Agents Prograf is indicated for the prophylaxis of organ rejection in patients receiving allogeneic kidney transplants. It is recommended that Prograf be used concomitantly with azathioprine or mycophenolate mofetil (MMF) and adrenal corticosteroids. /Included in US product label/ Prograf is indicated for the prophylaxis of organ rejection in patients receiving allogeneic liver transplants. It is recommended that Prograf be used concomitantly with adrenal corticosteroids. Therapeutic drug monitoring is recommended for all patients receiving Prograf. /Included in US product label/ Prograf is indicated for the prophylaxis of organ rejection in patients receiving allogeneic heart transplants. It is recommended that Prograf be used concomitantly with azathioprine or mycophenolate mofetil (MMF) and adrenal corticosteroids. /Included in US product label/ For more Therapeutic Uses (Complete) data for Tacrolimus (13 total), please visit the HSDB record page. Drug Warnings /BOXED WARNING/ MALIGNANCIES AND SERIOUS INFECTIONS. Increased risk of development of lymphoma and other malignancies, particularly of the skin, due to immunosuppression. Increased susceptibility to bacterial, viral, fungal, and protozoal infections, including opportunistic infections. Only physicians experienced in immunosuppressive therapy and management of organ transplant patients should prescribe Prograf. Patients receiving the drug should be managed in facilities equipped and staffed with adequate laboratory and supportive medical resources. The physician responsible for maintenance therapy should have complete information requisite for the follow-up of the patient. /BOXED WARNING/ WARNING: Long-term Safety of Topical Calcineurin Inhibitors Has Not Been Established Although a causal relationship has not been established, rare cases of malignancy (e.g., skin and lymphoma) have been reported in patients treated with topical calcineurin inhibitors, including Protopic Ointment. Therefore: Continuous long-term use of topical calcineurin inhibitors, including Protopic Ointment, in any age group should be avoided, and application limited to areas of involvement with atopic dermatitis; Protopic Ointment is not indicated for use in children less than 2 years of age; Only 0.03% Protopic Ointment is indicated for use in children 2-15 years of age. Topical tacrolimus therapy should be avoided for malignant or premalignant skin conditions (e.g., cutaneous T-cell lymphoma (CTCL)), which may appear clinically similar to dermatitis. Because of a potential increased risk for skin cancer, patients /using topical tacrolimus/ should be advised to limit exposure to sunlight or other UV light by wearing protective clothing and using a broad-spectrum sunscreen with a high protection factor. For more Drug Warnings (Complete) data for Tacrolimus (42 total), please visit the HSDB record page. Pharmacodynamics Tacrolimus acts by reducing peptidyl-prolyl isomerase activity by binding to the immunophilin FKBP-12 (FK506 binding protein) creating a new complex. This inhibits both T-lymphocyte signal transduction and IL-2 transcription. Tacrolimus has similar activity to cyclosporine but rates of rejection are lower with tacrolimus. Tacrolimus has also been shown to be effective in the topical treatment of eczema, particularly atopic eczema. It suppresses inflammation in a similar way to steroids, but is not as powerful. An important dermatological advantage of tacrolimus is that it can be used directly on the face; topical steroids cannot be used on the face, as they thin the skin dramatically there. On other parts of the body, topical steroid are generally a better treatment. Cyclosporin A and FK506 inhibit T- and B-cell activation and other processes essential to an effective immune response. In T lymphocytes these drugs disrupt an unknown step in the transmission of signals from the T-cell antigen receptor to cytokine genes that coordinate the immune response. The putative intracellular receptors for FK506 and cyclosporin are cis-trans prolyl isomerases. Binding of the drug inhibits isomerase activity, but studies with other prolyl isomerase inhibitors and analysis of cyclosporin-resistant mutants in yeast suggest that the effects of the drug result from the formation of an inhibitory complex between the drug and isomerase, and not from inhibition of isomerase activity. A transcription factor, NF-AT, which is essential for early T-cell gene activation, seems to be a specific target of cyclosporin A and FK506 action because transcription directed by this protein is blocked in T cells treated with these drugs, with little or no effect on other transcription factors such as AP-1 and NF-kappa B. Here we demonstrate that NF-AT is formed when a signal from the antigen receptor induces a pre-existing cytoplasmic subunit to translocate to the nucleus and combine with a newly synthesized nuclear subunit of NF-AT. FK506 and cyclosporin A block translocation of the cytoplasmic component without affecting synthesis of the nuclear subunit. [1] Antigen recognition by the T-cell receptor (TCR) initiates events including lymphokine gene transcription, particularly interleukin-2, that lead to T-cell activation. The immunosuppressive drugs, cyclosporin A (CsA) and FK-506, prevent T-cell proliferation by inhibiting a Ca(2+)-dependent event required for induction of interleukin-2 transcription. Complexes of FK-506 or CsA and their respective intracellular binding proteins inhibit the calmodulin-dependent protein phosphatase, calcineurin, in vitro. The pharmacological relevance of this observation to immunosuppression or drug toxicity is undetermined. Calcineurin, although present in lymphocytes, has not been implicated in TCR-mediated activation of lymphokine genes or in transcriptional regulation in general. Here we report that transfection of a calcineurin catalytic subunit increases the 50% inhibitory concentration (IC50) of the immunosuppressants FK-506 and CsA, and that a mutant subunit acts in synergy with phorbol ester alone to activate the interleukin-2 promoter in a drug-sensitive manner. These results implicate calcineurin as a component of the TCR signal transduction pathway by demonstrating its role in the drug-sensitive activation of the interleukin-2 promoter.[2] The immunosuppressive agents cyclosporin A (CsA) and FK 506 bind to distinct families of intracellular proteins (immunophilins) termed cyclophilins and FK 506-binding proteins (FKBPs). Recently, it has been shown that, in vitro, the complexes of CsA-cyclophilin and FK 506-FKBP-12 bind to and inhibit the activity of calcineurin, a calcium-dependent serine/threonine phosphatase. We have investigated the effects of drug treatment on phosphatase activity in T lymphocytes. Calcineurin is expressed in T cells, and its activity can be measured in cell lysates. Both CsA and FK 506 specifically inhibit cellular calcineurin at drug concentrations that inhibit interleukin 2 production in activated T cells. Rapamycin, which binds to FKBPs but exhibits different biological activities than FK 506, has no effect on calcineurin activity. Furthermore, excess concentrations of rapamycin prevent the effects of FK 506, apparently by displacing FK 506 from FKBPs. These results show that calcineurin is a target of drug-immunophilin complexes in vivo and establish a physiological role for calcineurin in T-cell activation.[3] |
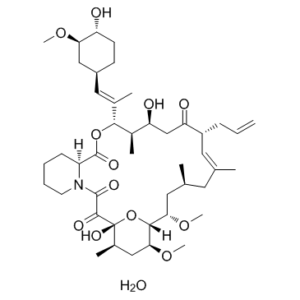
| 分子式 |
C44H71NO13
|
|
|---|---|---|
| 分子量 |
822.05
|
|
| 精确质量 |
821.492
|
|
| 元素分析 |
C, 64.29; H, 8.71; N, 1.70; O, 25.30
|
|
| CAS号 |
109581-93-3
|
|
| 相关CAS号 |
Tacrolimus;104987-11-3
|
|
| PubChem CID |
5282315
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 沸点 |
871.7ºC at 760 mmHg
|
|
| 熔点 |
127-129°
|
|
| 闪点 |
481ºC
|
|
| 蒸汽压 |
1.73E-35mmHg at 25°C
|
|
| 来源 |
fungus Streptomyces tsukubaensis.
|
|
| LogP |
4.512
|
|
| tPSA |
187.59
|
|
| 氢键供体(HBD)数目 |
4
|
|
| 氢键受体(HBA)数目 |
13
|
|
| 可旋转键数目(RBC) |
7
|
|
| 重原子数目 |
58
|
|
| 分子复杂度/Complexity |
1480
|
|
| 定义原子立体中心数目 |
14
|
|
| SMILES |
O1[C@]2(C(C(N3C([H])([H])C([H])([H])C([H])([H])C([H])([H])[C@@]3([H])C(=O)O[C@]([H])(/C(/C([H])([H])[H])=C(\[H])/[C@]3([H])C([H])([H])C([H])([H])[C@]([H])([C@@]([H])(C3([H])[H])OC([H])([H])[H])O[H])[C@]([H])(C([H])([H])[H])[C@]([H])(C([H])([H])C([C@]([H])(C([H])([H])C([H])=C([H])[H])C([H])=C(C([H])([H])[H])C([H])([H])[C@]([H])(C([H])([H])[H])C([H])([H])[C@@]([H])([C@]1([H])[C@]([H])(C([H])([H])[C@@]2([H])C([H])([H])[H])OC([H])([H])[H])OC([H])([H])[H])=O)O[H])=O)=O)O[H].O([H])[H] |c:78|
|
|
| InChi Key |
NWJQLQGQZSIBAF-MLAUYUEBSA-N
|
|
| InChi Code |
InChI=1S/C44H69NO12.H2O/c1-10-13-31-19-25(2)18-26(3)20-37(54-8)40-38(55-9)22-28(5)44(52,57-40)41(49)42(50)45-17-12-11-14-32(45)43(51)56-39(29(6)34(47)24-35(31)48)27(4)21-30-15-16-33(46)36(23-30)53-7;/h10,19,21,26,28-34,36-40,46-47,52H,1,11-18,20,22-24H2,2-9H3;1H2/b25-19+,27-21+;/t26-,28+,29+,30-,31+,32-,33+,34-,36+,37-,38-,39+,40+,44+;/m0./s1
|
|
| 化学名 |
(1R,9S,12S,13R,14S,17R,18E,21S,23S,24R,25S,27R)-1,14-dihydroxy-12-[(E)-1-[(1R,3R,4R)-4-hydroxy-3-methoxycyclohexyl]prop-1-en-2-yl]-23,25-dimethoxy-13,19,21,27-tetramethyl-17-prop-2-enyl-11,28-dioxa-4-azatricyclo[22.3.1.04,9]octacos-18-ene-2,3,10,16-tetrone;hydrate
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 本产品在运输和储存过程中需避光。 |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (3.04 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (3.04 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL 澄清 DMSO 储备液加入到 900 μL 玉米油中并混合均匀。 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.2165 mL | 6.0824 mL | 12.1647 mL | |
| 5 mM | 0.2433 mL | 1.2165 mL | 2.4329 mL | |
| 10 mM | 0.1216 mL | 0.6082 mL | 1.2165 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。