| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| Other Sizes |
|
| 靶点 |
TTR (transthyretin) (EC50 = 2.7-3.2 μM)
Transthyretin (TTR) tetramer (binds with negative cooperativity to the two thyroxine-binding sites; \(K_{d1} \sim 2-3 \text{ nM}\), \(K_{d2} \sim 154-278 \text{ nM}\); EC\(_{50}\) ~2.7–3.2 µM for fibril inhibition under acidic conditions) [1] |
|---|---|
| 体外研究 (In Vitro) |
当 tacamimeis 与两个四聚体典型保守的极化蛋白结合位点以负耦合(Kd = ∼2 nM 和 ∼200 nM)结合时,TTR 是动力学稳定的 [1]。在 =4.4-4.5 72 小时后,tacramids (0-7.2 μM) 剂量依赖性地抑制 WT-TTR 淀粉样变性 [1]。
在酸性、促进纤维形成的条件下(pH 4.4–4.5,孵育72小时),氯苯唑酸能剂量依赖性地抑制野生型(WT)、V30M 和 V122I TTR 同源四聚体的淀粉样纤维形成,EC\(_{50}\) 值对应的氯苯唑酸与TTR摩尔比小于1。 氯苯唑酸能动力学稳定TTR四聚体,抵抗尿素介导的变性(6.5 M尿素,72小时),在2:1摩尔比下,四聚体解离率低于3%。 氯苯唑酸在人血浆中选择性地与TTR结合,结合化学计量比约为每个TTR四聚体结合0.81 ± 0.02个氯苯唑酸分子,表明其在血浆蛋白中的高选择性。 在尿素变性应激下,氯苯唑酸能稳定多种致病性TTR变体(V30M、Y69H、F64S、I84S、V122I、L111M)。[1] |
| 体内研究 (In Vivo) |
ATTR淀粉样变性是一种由转甲状腺素(TTR)淀粉样蛋白积聚引起的系统性、衰弱性和致命性疾病。RNA干扰(RNAi)是一种经过临床验证的技术,可能是治疗ATTR淀粉样变性的一种很有前途的方法。绝大多数TTR是TTR淀粉样蛋白的可溶性前体,在肝脏中表达和合成。RNAi技术实现了强大的肝脏基因沉默,其目标是降低全身TTR水平,并减轻肝脏TTR表达引起的ATTR的许多临床表现。为了验证这一假设,在遗传性ATTR淀粉样变性的小鼠模型中评估了TTR靶向siRNA。RNAi介导的肝TTR表达沉默抑制了TTR沉积,并促进了病理相关组织中现有TTR沉积的消退。此外,沉积回归的程度与RNAi介导的敲除水平相关。与TTR稳定剂tafamidis相比,RNAi介导的TTR敲低导致TTR沉积在更广泛的受影响组织中更大程度的消退。总之,本文提供的数据支持TTR降低背后的治疗假说,并强调了RNAi在治疗ATTR淀粉样变性患者中的潜力[2]。
在一项针对V30M TTR-FAP患者的tafamidis II/III期临床试验中,这种动力学稳定剂在18个月的治疗中显示出临床疗效。与安慰剂对照组相比,接受tafamidis治疗的患者神经系统恶化减少了52%,大小神经纤维功能分别保留了53%和80%,营养状况得到改善,这些结果与生活质量的提高有关。当与临床疗效数据相结合时,其中提供的tafamidis临床前数据提供了支持淀粉样蛋白假说的独特药理学证据,即降低淀粉样蛋白级联反应的效率可以阻止外周神经和自主神经系统的退化[1]。 在一项针对V30M TTR-FAP患者的II/III期临床试验中,与安慰剂相比,接受氯苯唑酸治疗18个月的患者神经功能恶化减少52%,大神经纤维和小神经纤维功能保留率分别为53%和80%,营养状况得到改善。[1] |
| 酶活实验 |
塔法米迪斯在其T4结合位点与TTR具有高亲和力结合。Tafamidis稳定较弱的TTR二聚体-二聚体界面。塔法米迪斯选择性地与人血浆中的TTR结合。塔法米迪斯稳定人血浆中的WT、V30M和V122I TTR。塔法米迪斯可稳定多种致病性TTR变体。<小时>
人血浆中TTR四聚体稳定性的免疫浊度测定。[1] TTR在人血浆中的尿素变性和化学交联如所述进行(参见文本和图6),除了通过免疫浊度对TTR进行定量外,进行了轻微的修改。将人血浆样品在冰上解冻,并通过离心除去不溶性物质。对于每种,去除4µL,并通过免疫浊度测定初始TTR浓度。对于每次稳定性测定,保留80µL等分的每份血浆样品,并加入1.6µL的5%二甲基亚砜(DMSO)或360µM的5%二甲亚砜中的太酰胺。在室温下孵育15分钟后,加入120µL尿素缓冲液(8M尿素、40mM磷酸钠、80mM KCl,pH 7.4),将样品混合并在室温下温育指定时间(通常为48小时)。所有样品均用3.2µL 25%戊二醛交联。4分钟后,用5.6µL 1.85 M NaBH4(在0.1 N NaOH中新鲜制备)猝灭反应并孵育5分钟。通过免疫浊度测定变性后TTR浓度(4µL)。根据制造商的说明使用Olympus OSR6175试剂和Prealbumin校准器ODR3029。为了评估两种检测方法之间的相关性,我们通过蛋白质印迹和免疫浊度平行分析了尿素处理和戊二醛交联后的血浆样品。在对照样品中,在尿素中3天后,通过免疫浊度检测到的TTR的量从22 mg/dL的初始值降低到3 mg/dL。在存在太酰胺的情况下,残留13 mg/dL的TTR;该水平与来自蛋白质印迹测定的结果非常一致(图S3A)。 使用等温滴定量热法(ITC)测定结合常数。将氯苯唑酸溶液滴定到含有WT-TTR(17 µM)的样品池中,温度25°C。测量热量变化并积分生成结合等温线,拟合负协同模型得到 \(K_{d1} = 3 \text{ nM}\) 和 \(K_{d2} = 278 \text{ nM}\)。[1] 在生理pH下进行亚基交换实验,通过分析未结合TTR四聚体比例随氯苯唑酸浓度的变化,间接测定四聚体解离速率并计算结合常数(\(K_{d1} = 2 \text{ nM}\),\(K_{d2} = 154 \text{ nM}\))。[1] |
| 动物实验 |
Evaluation of tafamidis in hTTR V30M HSF1± mice[2]
Tafamidis/meglumine (tafamidis) and its respective meglumine only control (meglumine) were prepared as previously described. Four hundred microliters of 2 mg/ml tafamidis (0.8 mg total) or its respective meglumine control were administered via subcutaneous injection to 15-month-old hTTR V30M HSF1± mice on days 0, 3, 5, 7, 10, 12, 14, 17, 19, 21, 24, 26, 28, 31, 33, 35 and 38. TTR tissue deposition was evaluated on day 52 as described earlier. To confirm tafamidis-mediated stabilization of serum TTR, serum TTR tetramer stability was analyzed on days -7, 9, 23 and 37 using a modified version of a previously described TTR tetramer stability assay. See Supplementary Figure 2 for more detail on assay conditions and tetramer detection and quantitation. To quantify the extent of stabilization, % TTR tetramer stabilization was calculated using the following equation as previously described. To compare the efficacy of the tetramer stabilization approach to that of RNAi-mediated TTR knockdown, we evaluated tafamidis in the hTTR V30M HSF1± model and quantified the impact of TTR tetramer stabilization on the regression of preexisting TTR deposits. To compensate for differences in dose frequency and route of administration, mice were administered excess tafamidis (>100× on mg/kg basis) to enable sufficient TTR tetramer stabilization. Although administration of tafamidis resulted in a significant and clinically relevant degree of serum TTR tetramer stabilization, only moderate TTR deposit regression was observed in the sciatic nerve and dorsal root ganglion; consistent regression was not observed in other tissues examined. It should be noted that the study duration was chosen to allow a more direct comparison with siTTR1 (Figure 3) and, as such, it is possible that longer term administration of tafamidis may have resulted in greater deposit regression in the hTTR V30M HSF1± model. However, in these conditions, TTR lowering seems to be more effective. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Tafamidis reaches a Cmax of 1430.93ng/mL with a Tmax of 1.75h fasted and 4h fed. The AUC of tafamidis is 47,864.31ng\h/mL. A 20mg oral dose of tafamidis is approximately 59% recovered in the feces, largely as unchanged drug. Approximately 22% of a 20mg oral dose is recovered in the urine, mostly as the glucuronide metabolite. The apparent volume of distribution at steady state is 18.5L. The oral clearance of tafamidis is 0.263L/h. The apparent total clearance is 0.44L/h. Metabolism / Metabolites Tafamidis is largely not subject to first pass or oxidative metabolism, being 90% unchanged after in in vitro experiments. Preclinical data suggest tafamidis is mainly metabolized through glucuronidation and excreted in bile. Biological Half-Life The half life of tafamidis is 49h. Tafamidis is orally bioavailable and selectively binds TTR in blood without significant binding to other plasma proteins.[1] The plasma half-life of TTR is approximately 24 hours, and tafamidis stabilizes TTR over this period as shown in subunit exchange experiments.[1] |
| 毒性/毒理 (Toxicokinetics/TK) |
Protein Binding
Tafamidis 99.9% protein bound in plasma, mostly to transthyretin. Tafamidis was well tolerated in clinical trials with no clinically relevant effects on thyroid function or laboratory measures, despite binding to thyroxine-binding sites on TTR.[1] |
| 参考文献 | |
| 其他信息 |
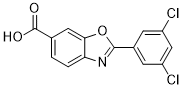
Tafamidis is a member of the class of 1,3-benzoxazoles that is 1,3-benzoxazole-6-carboxylic acid in which the hydrogen at position 2 is replaced by a 3,5-dichlorophenyl group. Used (as its meglumine salt) for the amelioration of transthyretin-related hereditary amyloidosis. It has a role as a central nervous system drug. It is a member of 1,3-benzoxazoles, a monocarboxylic acid and a dichlorobenzene. It is a conjugate acid of a tafamidis(1-).
Tafamidis and tafamidis meglumine (FX-1006A) are benzoxazole derivatives developed by FoldRX. Tafamidis is structurally similar to diflusinal. Tafamidis was granted an EMA market authorisation on 16 November 2011 and FDA approval on 3 May 2019. See also: Tafamidis Meglumine (has salt form). Drug Indication Tafamidis is indicated to treat cardiomyopathy of wild type or hereditary transthyretin-mediated amyloidosis in adults. FDA Label Mechanism of Action Genetic mutations or natural misfolding of transthyretin destabalizes transthyretin tetramers, leading to their dissociation and aggregation in tissues, and disrupting the normal function of these tissues. Tafamidis binds to transthyretin tetramers at the thyroxin binding sites, stabilizing the tetramer, reducing the availability of monomers for amyloidogenesis. Pharmacodynamics Tafamidis stabilizes transthyretin tetramers, reducing the amount of monomers available for amyloidogenesis. It has a long duration of action as it is given once daily, and a wide therapeutic window. Tafamidis is a benzoxazole derivative (2-(3,5-dichloro-phenyl)-benzoxazole-6-carboxylic acid) developed as an orally available TTR kinetic stabilizer to inhibit tetramer dissociation, the rate-limiting step in TTR amyloidogenesis. It mimics the protective effect of the T119M mutation, which slows tetramer dissociation and prevents disease in compound heterozygotes. The crystal structure of tafamidis bound to TTR (1.3 Å resolution) shows it occupies the thyroxine-binding sites, with hydrophobic interactions from dichloro-substituents and water-mediated H-bonds via its carboxylate group, stabilizing the dimer-dimer interface.[1] |
| 分子式 |
C14H7CL2NO3
|
|---|---|
| 分子量 |
308.1163
|
| 精确质量 |
306.98
|
| 元素分析 |
C, 54.58; H, 2.29; Cl, 23.01; N, 4.55; O, 15.58
|
| CAS号 |
594839-88-0
|
| 相关CAS号 |
Tafamidis meglumine;951395-08-7;Tafamidis-d3
|
| PubChem CID |
11001318
|
| 外观&性状 |
Typically exists as white to off-white solids at room temperature
|
| 密度 |
1.5±0.1 g/cm3
|
| 沸点 |
486.7±40.0 °C at 760 mmHg
|
| 闪点 |
248.1±27.3 °C
|
| 蒸汽压 |
0.0±1.3 mmHg at 25°C
|
| 折射率 |
1.677
|
| LogP |
5.29
|
| tPSA |
63.33
|
| 氢键供体(HBD)数目 |
1
|
| 氢键受体(HBA)数目 |
4
|
| 可旋转键数目(RBC) |
2
|
| 重原子数目 |
20
|
| 分子复杂度/Complexity |
371
|
| 定义原子立体中心数目 |
0
|
| SMILES |
ClC1C([H])=C(C([H])=C(C=1[H])C1=NC2C([H])=C([H])C(C(=O)O[H])=C([H])C=2O1)Cl
|
| InChi Key |
TXEIIPDJKFWEEC-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C14H7Cl2NO3/c15-9-3-8(4-10(16)6-9)13-17-11-2-1-7(14(18)19)5-12(11)20-13/h1-6H,(H,18,19)
|
| 化学名 |
2-(3,5-dichlorophenyl)benzo[d]oxazole-6-carboxylic acid
|
| 别名 |
Fx-1006, PF06291826; Fx1006, PF-06291826; Fx 1006, Fx-1006A; PF 06291826; Tafamidis; Vyndaqel; TAFAMIDIS; 594839-88-0; Vyndamax; FX-1006; 2-(3,5-Dichlorophenyl)-1,3-Benzoxazole-6-Carboxylic Acid; 2-(3,5-Dichlorophenyl)-6-benzoxazole carboxylic acid; tafamidisum; 8FG9H9D31J;
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ~37.5 mg/mL (~121.71 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 2.5 mg/mL (8.11 mM) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 悬浮液;超声助溶。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: 2.5 mg/mL (8.11 mM) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 悬浊液; 超声助溶。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (8.11 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 3.2455 mL | 16.2274 mL | 32.4549 mL | |
| 5 mM | 0.6491 mL | 3.2455 mL | 6.4910 mL | |
| 10 mM | 0.3245 mL | 1.6227 mL | 3.2455 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。