| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 1mg |
|
||
| 2mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| Other Sizes |
|
| 靶点 |
mTOR (IC50 = 1.76 μM)
|
|---|---|
| 体外研究 (In Vitro) |
在缺乏 FKBP12 的情况下,Temsirolimus 有效抑制 mTOR 激酶活性,IC50 为 1.76 μM,与雷帕霉素相似,IC50 为 1.74 μM。纳摩尔浓度(10 nM 至 <5 μM)的替西罗莫司治疗通过 FKBP12 依赖性机制表现出适度且选择性的抗增殖活性,但在低微摩尔浓度(5-15 μM)下,它可以完全抑制多种肿瘤的增殖细胞通过以不依赖 FKBP12 的方式抑制 mTOR 信号传导。用微摩尔(20 μM)而非纳摩尔浓度的替西罗莫司治疗会导致总体蛋白质合成和多核糖体分解显着减少,同时翻译延伸因子 eEF2 和翻译起始因子 eIF2A 的磷酸化急剧上升.[1] Temsirolimus 以浓度依赖性方式抑制两种细胞的细胞生长和克隆存活,但在 PTEN 阳性 DU145 细胞中比在 PTEN 阴性 PC-3 细胞中更有效。它还抑制核糖体蛋白 S6 的磷酸化。 [2] 替西罗莫司 (100 ng/mL) 可有效抑制原代人淋巴细胞白血病 (ALL) 细胞的增殖并诱导细胞凋亡。[3]
|
| 体内研究 (In Vivo) |
在人类 ALL 的 NOD/SCID 异种移植模型中,每天 10 mg/kg 的替西罗莫司治疗可减少外周血原始细胞和脾肿大。 [3]与对照相比,Temsirolimus(腹膜内注射 20 mg/kg,5 天/周)显着减慢 DAOY 异种移植物的生长,1 周后延迟 160%,2 周后延迟 240%。单次高剂量替西罗莫司(100 mg/kg ip)治疗一周可使肿瘤体积减少 37%。替西罗莫司治疗 2 周后,雷帕霉素耐药 U251 异种移植物的生长也延迟了 148%。 [4] Temsirolimus 对 mTOR 的抑制可增强亨廷顿病小鼠模型四种不同行为任务的表现并减少聚集体形成。 [5] Temsirolimus 给药对 8226、OPM-2 和 U266 异种移植物的皮下生长产生显着的剂量依赖性抗肿瘤反应,8226 和 OPM-2 的 ED50 值分别为 20 mg/kg 和 2 mg/kg。这些反应与肿瘤细胞生长减少和血管生成抑制以及细胞凋亡增加和增殖抑制有关。 [6]
|
| 酶活实验 |
使用带有 Flag 标签的野生型人 mTOR (Flag-mTOR) DNA 构建体瞬时转染 HEK293 细胞。 48小时后,提取并纯化Flag-mTOR蛋白。纯化的Flag-mTOR体外激酶测定在96孔板中在不同浓度的Temsirolimus存在下进行,不含FKBP12,并使用解离增强镧系元素荧光免疫分析(DELFIA)方法以His6-S6K1为底物检测结果。首先在激酶测定缓冲液(10 mM Hepes (pH 7.4)、50 mM NaCl、50 mM β-甘油磷酸、10 mM MnCl2、0.5 mM DTT、0.25 μM 微囊藻毒素 LR 和 100 μg/mL BSA)中稀释酶。将 12 μL 稀释酶和 0.5 μL 替西罗莫司在每个孔中快速混合。通过添加 12.5 μL ATP 和含有 His6-S6K 的激酶测定缓冲液开始激酶反应,以创建 25 μL 的最终反应体积,其中包含 800 ng/mL FLAG-mTOR、100 μM ATP 和 1.25 μM His6-S6K。将反应板在室温下孵育 2 小时(1-6 小时呈线性)并轻轻摇动,然后添加 25 μL 终止缓冲液(20 mM Hepes (pH 7.4)、20 mM EDTA 和 20 mM EGTA)终止反应。 。使用铕-N1-ITC (Eu)(每个抗体 10.4 Eu)标记的单克隆抗 P(T389)-p70S6K 抗体用于室温下磷酸化 (Thr-389) His6-S6K 的 DELFIA 检测。将 45 μL 终止的激酶反应混合物转移至含有 55 μL PBS 的 MaxiSorp 板。将 Eu-P(T389)-S6K 抗体以 40 ng/mL 的浓度添加到 100 μL DELFIA 缓冲液中。在最小程度的搅拌下,抗体结合再持续一小时。然后使用含 0.05% Tween 20 (PBST) 的 PBS 吸出并清洁孔。在使用 PerkinElmer Victor 型读板器读取板之前,每个孔均接收 100 L DELFIA 增强溶液。
|
| 细胞实验 |
将替西罗莫司以一定浓度范围应用于细胞 72 小时。处理后使用 CellTiter AQ 检测试剂盒测量 MTS 染料转化率来评估活细胞密度。
在细胞培养研究中,替西罗莫司/CCI-779在常用的纳摩尔浓度下通常具有适度的选择性抗增殖活性。在这里,我们报道,在临床相关的低微摩尔浓度下,CCI-779完全抑制了广泛的肿瘤细胞的增殖。这种“高剂量”药物效应不需要FKBP12,并且与FKBP12不依赖的mTOR信号抑制相关。fkbp12 -雷帕霉素结合域(FRB)结合缺陷的雷帕霉素类似物未能引起纳米摩尔和微摩尔的生长抑制和mTOR信号传导,暗示FRB结合在这两种作用中。生化试验表明,CCI-779和雷帕霉素直接抑制mTOR激酶活性,IC(50)值分别为1.76 +/- 0.15和1.74 +/- 0.34微mol/L。有趣的是,抗CCI-779 mTOR突变体(mTOR- si)在体外对微摩尔CCI-779表现出11倍的抗性(IC(50), 20 +/- 3.4微mol/L),并且在暴露于微摩尔CCI-779的细胞中具有部分保护作用。用微摩尔浓度的CCI-779而不是纳摩尔浓度的CCI-779治疗癌细胞会导致整体蛋白质合成和多核糖体分解的显著下降。蛋白质合成的深度抑制伴随着翻译延伸因子eIF2和翻译起始因子eIF2 α磷酸化的快速增加。这些发现表明,高剂量CCI-779通过不依赖于fkbp12的机制抑制mTOR信号传导,从而导致深刻的翻译抑制。这种独特的高剂量药物效应可能与CCI-779及其他类似物在人类癌症患者中的抗肿瘤活性直接相关。[1] 研究人员研究了雷帕霉素类似物CCI-779,单独或联合化疗,作为人类前列腺癌细胞系PC-3和DU145增殖的抑制剂。通过免疫染色和/或Western blotting检测PTEN和phospho-Akt/PKB状态以及CCI-779对核糖体蛋白S6磷酸化的影响。磷酸化akt /PKB在PTEN突变型PC-3细胞和异种移植物中的表达高于PTEN野生型DU145细胞。CCI-779在两种细胞系中均能抑制S6的磷酸化。培养的细胞每周用米托蒽醌或多西紫杉醇治疗2个周期,疗程之间给予CCI-779或载体。CCI-779以剂量依赖的方式抑制两种细胞系的生长和克隆存活,但在化疗疗程之间给予CCI-779时影响最小。[2] 来自成年B淋巴细胞前体ALL患者的淋巴母细胞在骨髓基质上培养,并使用CCI-779(第二代MTI)治疗。与未处理的细胞相比,处理后的细胞增殖明显减少,凋亡细胞增加。我们还评估了CCI-779在NOD/SCID异种移植模型中的作用。我们在疾病建立后用CCI-779治疗了来自同一患者样本的68只小鼠。用CCI-779治疗的动物外周血母细胞减少,脾肿大。与之形成鲜明对比的是,未经治疗的动物继续表现出人类ALL的扩张。我们通过免疫印迹验证mTOR信号传导中间磷酸化- s6在人ALL中的抑制作用,发现暴露于CCI-779的异种移植人ALL中该靶点下调。我们的结论是,MTIs可以抑制成人ALL的生长,值得仔细研究作为治疗药物的治疗药物,以对抗目前的治疗方法通常无法治愈的疾病。[3] |
| 动物实验 |
Cells are implanted in matrigel for the creation of xenografts; matrigel is stored at −20°C and thawed on ice at 4°C for 3 hours prior to use. After being gently resuspended in 1 mL of PBS, the cells are incubated for 5 minutes on ice. Cells are transferred to the tube containing 1 mL of matrigel using a prechilled pipette, and the cell concentration is adjusted to 3×107/mL. Using a 25-gauge needle, the cells (3×106 in 0.1 mL) are injected s.c. into the mice's flanks. When xenografts grew to a size of about 5 mm in diameter, animals are assorted randomLy into groups of 10 mice. The following experiments are conducted: Mice bearing PC-3 tumors are treated with CCI-779 (1, 5, 10, and 20 mg per kg per day), or vehicle solution for 3 or 5 days per week for 3 weeks. Mice bearing DU145 tumors are only treated with CCI-779 (20 mg per kg per day) or vehicle solution for 3 weeks. Mice bearing PC-3 tumors receive the following treatments: (a) control, vehicle solution for CCI-779; (b) chemotherapy alone, mitoxantrone 1.5 mg/kg or docetaxel 10 mg/kg is injected i.p. weekly for 3 doses; (c) CCI-779 alone, 5 or 10 mg/kg is injected i.p. daily, three times a week for 3 weeks; (4) chemotherapy followed by CCI-779.
|
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Infused intravenous over 30 - 60 minutes. Cmax is typically observed at the end of infusion Excreted predominantly in feces (76%), 4.6% of drug and metabolites recovered in urine. 17% of drug was not recovered by either route following a 14-day sample collection. 172 L in whole blood of cancer patients; both temsirolimus and sirolimus are extensive distributed partitioned into formed blood elements 16.2 L/h (22%) Following administration of a single 25 mg dose of temsirolimus in patients with cancer, mean temsirolimus Cmax in whole blood was 585 ng/mL (coefficient of variation, CV =14%), and mean AUC in blood was 1627 ng.hr/mL (CV=26%). Typically Cmax occurred at the end of infusion. Over the dose range of 1 mg to 25 mg, temsirolimus exposure increased in a less than dose proportional manner while sirolimus exposure increased proportionally with dose. Following a single 25 mg intravenous dose in patients with cancer, sirolimus AUC was 2.7-fold that of temsirolimus AUC, due principally to the longer half-life of sirolimus. Following a single 25 mg intravenous dose, mean steady-state volume of distribution of temsirolimus in whole blood of patients with cancer was 172 liters. Both temsirolimus and sirolimus are extensively partitioned into formed blood elements. Following a single 25 mg dose of temsirolimus in patients with cancer, temsirolimus mean (CV) systemic clearance was 16.2 (22%) L/hr. It is not known whether temsirolimus is excreted into human milk... Following IV administration of a single radiolabeled dose of temsirolimus, approximately 78% of the total radioactivity is recovered in feces and 4.6% in urine within 14 days. Metabolism / Metabolites Primarily metabolized by cytochrome P450 3A4 in the human liver. Sirolimus, an equally potent metabolite, is the primary metabolite in humans following IV infusion. Other metabolic pathways observed in in vitro temsirolimus metabolism studies include hydroxylation, reduction and demethylation. Sirolimus, an active metabolite of temsirolimus, is the principal metabolite in humans following intravenous treatment. The remainder of the metabolites account for less than 10% of radioactivity in the plasma. Temsirolimus is metabolized by hydrolysis to sirolimus, the principal active metabolite. Both temsirolimus and sirolimus also are metabolized by cytochrome P-450 (CYP) isoenzyme 3A4. Although temsirolimus is metabolized to sirolimus, temsirolimus itself exhibits antitumor activity and is not considered a prodrug. The in vitro metabolism of temsirolimus, (rapamycin-42-[2,2-bis-(hydroxymethyl)]-propionate), an antineoplastic agent, was studied using human liver microsomes as well as recombinant human cytochrome P450s, namely CYP3A4, 1A2, 2A6, 2C8, 2C9, 2C19, and 2E1. Fifteen metabolites were detected by liquid chromatography (LC)-tandem mass spectrometry (MS/MS or MS/MS/MS). CYP3A4 was identified as the main enzyme responsible for the metabolism of the compound. Incubation of temsirolimus with recombinant CYP3A4 produced most of the metabolites detected from incubation with human liver microsomes, which was used for large-scale preparation of the metabolites. By silica gel chromatography followed by semipreparative reverse-phase high-performance liquid chromatography, individual metabolites were separated and purified for structural elucidation and bioactivity studies. The minor metabolites (peaks 1-7) were identified as hydroxylated or desmethylated macrolide ring-opened temsirolimus derivatives by both positive and negative mass spectrometry (MS) and MS/MS spectroscopic methods. Because these compounds were unstable and only present in trace amounts, no further investigations were conducted. Six major metabolites were identified as 36-hydroxyl temsirolimus (M8), 35-hydroxyl temsirolimus (M9), 11-hydroxyl temsirolimus with an opened hemiketal ring (M10 and M11), N- oxide temsirolimus (M12), and 32-O-desmethyl temsirolimus (M13) using combined LC-MS, MS/MS, MS/MS/MS, and NMR techniques. Compared with the parent compound, these metabolites showed dramatically decreased activity against LNCaP cellular proliferation. Biological Half-Life Temsirolimus exhibits a bi-exponential decline in whole blood concentrations and the mean half-lives of temsirolimus and sirolimus were 17.3 hr and 54.6 hr, respectively. Temsirolimus exhibits a bi-exponential decline in whole blood concentrations and the mean half-lives of temsirolimus and sirolimus were 17.3 hr and 54.6 hr, respectively. |
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
Serum aminotransferase elevations occur in 30% to 40% and alkaline phosphatase in 60% to 70% of patients receiving temsirolimus, but the abnormalities are usually mild, asymptomatic and self-limiting, rarely requiring dose modification or discontinuation. Elevations of liver enzymes above 5 times the upper limit of normal occur in only 1% to 3% of patients. Since approval and wide spread clinical use, there have been no case reports of clinically apparent liver injury attributed to temsirolimus use. Temsirolimus, like sirolimus, is immunosuppressive, and reactivation of hepatitis B is considered a possible complication of therapy. Yet despite more than 10 years of clinical use, there have been no reports of reactivation of hepatitis B attributed to temsirolimus therapy. Thus, acute liver injury with jaundice due to temsirolimus is probably quite rare, if it occurs at all. Hypersensitivity reactions to temsirolimus infusions are not uncommon (for which reason premedication with an antihistamine is recommended) and instances of Stevens Johnson syndrome have been reported. Likelihood score: E* (unproven but suspected rare cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Temsirolimus is a prodrug of sirolimus. Because no information is available on the use of temsirolimus or sirolimus during breastfeeding, an alternate drug may be preferred, especially while nursing a newborn or preterm infant. The manufacturer recommends that breastfeeding be discontinued during temsirolimus therapy and for 3 weeks following the last dose. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding 87% bound to plasma proteins in vitro at a concentration of 100 ng/ml Interactions CYP3A4 inhibitors: Potential pharmacokinetic interaction (increased plasma concentrations of the principal active metabolite sirolimus). Concomitant use with a potent CYP3A4 inhibitors should be avoided; if no alternative is available, consideration should be given to temsirolimus dosage adjustment. CYP3A4 inducers: Potential pharmacokinetic interaction (decreased plasma concentrations of the principal active metabolite sirolimus). Concomitant use with potent CYP3A4 inducers should be avoided; if no alternative is available, consideration should be given to temsirolimus dosage adjustment. Angioedema-type reactions observed during concomitant therapy with angiotensin-converting enzyme (ACE) inhibitors. Caution is advised. Increased risk of intracerebral bleeding in patients receiving concomitant therapy. Caution is advised. For more Interactions (Complete) data for Temsirolimus (17 total), please visit the HSDB record page. |
| 参考文献 |
|
| 其他信息 |
Therapeutic Uses
Temsirolimus is indicated for the treatment of advanced renal cell carcinoma. /Included in US product label/ Drug Warnings Anaphylaxis, dyspnea, flushing, and chest pain have been reported. Temsirolimus should be used with caution in patients with known hypersensitivity to the drug or its metabolites (eg, sirolimus), polysorbate 80, or any other ingredient in the formulation. Pretreatment with an antihistamine prior to each dose of temsirolimus is recommended to prevent hypersensitivity reactions. Temsirolimus should be used with caution in patients with known hypersensitivity to antihistamines or with conditions requiring avoidance of antihistamines. The safety and pharmacokinetics of temsirolimus were evaluated in a dose escalation phase 1 study in 110 patients with normal or varying degrees of hepatic impairment. Patients with baseline bilirubin >1.5 x ULN experienced greater toxicity than patients with baseline bilirubin /= grade 3 adverse reactions and deaths, including deaths due to progressive disease, were greater in patients with baseline bilirubin >1.5 x ULN. temsirolimus is contraindicated in patients with bilirubin >1.5 x ULN due to increased risk of death. Use caution when treating patients with mild hepatic impairment. Concentrations of temsirolimus and its metabolite sirolimus were increased in patients with elevated AST or bilirubin levels. If temsirolimus must be given in patients with mild hepatic impairment (bilirubin >1 - 1.5 x ULN or AST >ULN but bilirubin No clinical studies were conducted with temsirolimus in patients with decreased renal function. Less than 5% of total radioactivity was excreted in the urine following a 25 mg intravenous dose of (14)C-labeled temsirolimus in healthy subjects. Renal impairment is not expected to markedly influence drug exposure, and no dosage adjustment of temsirolimus is recommended in patients with renal impairment. For more Drug Warnings (Complete) data for Temsirolimus (29 total), please visit the HSDB record page. |
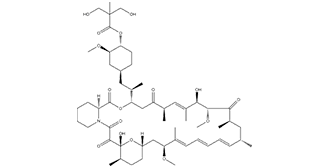
| 分子式 |
C56H87NO16
|
|---|---|
| 分子量 |
1030.29
|
| 精确质量 |
1029.602
|
| 元素分析 |
C, 65.28; H, 8.51; N, 1.36; O, 24.85
|
| CAS号 |
162635-04-3
|
| 相关CAS号 |
162635-04-3
|
| PubChem CID |
6918289
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
1.2±0.1 g/cm3
|
| 沸点 |
1048.4±75.0 °C at 760 mmHg
|
| 熔点 |
99-101ºC
|
| 闪点 |
587.8±37.1 °C
|
| 蒸汽压 |
0.0±0.6 mmHg at 25°C
|
| 折射率 |
1.554
|
| LogP |
2.96
|
| tPSA |
241.96
|
| 氢键供体(HBD)数目 |
4
|
| 氢键受体(HBA)数目 |
16
|
| 可旋转键数目(RBC) |
11
|
| 重原子数目 |
73
|
| 分子复杂度/Complexity |
2010
|
| 定义原子立体中心数目 |
15
|
| SMILES |
O(C([H])([H])[H])[C@@]1([H])[C@@]([H])(C([H])([H])C([H])([H])[C@@]([H])(C([H])([H])[C@@]([H])(C([H])([H])[H])[C@]2([H])C([H])([H])C([C@@]([H])(C([H])=C(C([H])([H])[H])[C@]([H])([C@]([H])(C([C@]([H])(C([H])([H])[H])C([H])([H])[C@]([H])(C([H])([H])[H])C([H])=C([H])C([H])=C([H])C([H])=C(C([H])([H])[H])[C@]([H])(C([H])([H])[C@]3([H])C([H])([H])C([H])([H])[C@@]([H])(C([H])([H])[H])[C@@](C(C(N4C([H])([H])C([H])([H])C([H])([H])C([H])([H])[C@@]4([H])C(=O)O2)=O)=O)(O[H])O3)OC([H])([H])[H])=O)OC([H])([H])[H])O[H])C([H])([H])[H])=O)C1([H])[H])OC(C(C([H])([H])[H])(C([H])([H])O[H])C([H])([H])O[H])=O |c:35,66,70,t:62|
|
| InChi Key |
CBPNZQVSJQDFBE-FUXHJELOSA-N
|
| InChi Code |
InChI=1S/C56H87NO16/c1-33-17-13-12-14-18-34(2)45(68-9)29-41-22-20-39(7)56(67,73-41)51(63)52(64)57-24-16-15-19-42(57)53(65)71-46(30-43(60)35(3)26-38(6)49(62)50(70-11)48(61)37(5)25-33)36(4)27-40-21-23-44(47(28-40)69-10)72-54(66)55(8,31-58)32-59/h12-14,17-18,26,33,35-37,39-42,44-47,49-50,58-59,62,67H,15-16,19-25,27-32H2,1-11H3/b14-12+,17-13+,34-18+,38-26+/t33-,35-,36-,37-,39-,40+,41+,42+,44-,45+,46+,47-,49-,50+,56-/m1/s1
|
| 化学名 |
[(1R,2R,4S)-4-[(2R)-2-[(1R,9S,12S,15R,16E,18R,19R,21R,23S,24E,26E,28E,30S,32S,35R)-1,18-dihydroxy-19,30-dimethoxy-15,17,21,23,29,35-hexamethyl-2,3,10,14,20-pentaoxo-11,36-dioxa-4-azatricyclo[30.3.1.04,9]hexatriaconta-16,24,26,28-tetraen-12-yl]propyl]-2-methoxycyclohexyl] 3-hydroxy-2-(hydroxymethyl)-2-methylpropanoate
|
| 别名 |
CCI-779; CCI779; Temsirolimus; Torisel; 162635-04-3; 624KN6GM2T; DTXSID2040945; UNII-624KN6GM2T; WAY-CCI 779; CCI 779; NSC 683864; NSC683864; NSC-683864; Temsirolimus; 624KN6GM2T; DTXSID2040945; UNII-624KN6GM2T; WAY-CCI 779; Brand name: Torisel
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: (1). 本产品在运输和储存过程中需避光。 (2). 请将本产品存放在密封且受保护的环境中(例如氮气保护),避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO: ~75 mg/mL (~72.8 mM)
Water: <1 mg/mL Ethanol: ~75 mg/mL (~72.8 mM) |
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 5 mg/mL (4.85 mM) (饱和度未知) in 10% EtOH + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,将 100 μL 50.0 mg/mL 澄清乙醇储备液加入到 400 μL PEG300 中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 5 mg/mL (4.85 mM) (饱和度未知) in 10% EtOH + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 50.0 mg/mL 澄清 EtOH 储备液添加到 900 μL 玉米油中并充分混合。 View More
配方 3 中的溶解度: ≥ 2.08 mg/mL (2.02 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: ≥ 2.08 mg/mL (2.02 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将100 μL 20.8 mg/mL 澄清 DMSO 储备液加入900 μL 玉米油中,混合均匀。 配方 5 中的溶解度: 30% PEG400+0.5% Tween80+5% propylene glycol:10mg/mL 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 0.9706 mL | 4.8530 mL | 9.7060 mL | |
| 5 mM | 0.1941 mL | 0.9706 mL | 1.9412 mL | |
| 10 mM | 0.0971 mL | 0.4853 mL | 0.9706 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Temsirolimus in Combination with Metformin in Patients with Advanced Cancers
CTID: NCT01529593
Phase: Phase 1 Status: Active, not recruiting
Date: 2024-11-07
Minimal toxicity of CCI-779 (Temsirolimus) in NOD/SCID mice.Blood.2004 Dec 15;104(13):4181-7. |
Antitumor effect of CCI-779.Blood.2004 Dec 15;104(13):4181-7. |
Antitumor effects of CCI-779.Blood.2004 Dec 15;104(13):4181-7. |
Antiangiogenic effects of CCI-779.Blood.2004 Dec 15;104(13):4181-7. |
CCI-779 induces myeloma cell apoptosis.
CCI-779''''s effects on p70S6kinase phosphorylation and cell-cycle regulatory proteins in vivo.Blood.2004 Dec 15;104(13):4181-7. |
|