| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 1mg |
|
||
| 2mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| Other Sizes |
|
| 靶点 |
Mer (IC50 = 0.74 nM); FLT3 (IC50 = 0.8 nM); Axl (IC50 = 14 nM); Tyro3 (IC50 = 17 nM)
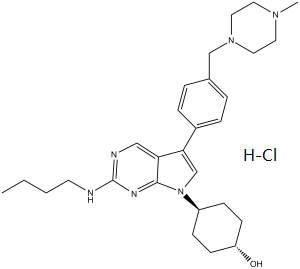
The targets of UNC-2025 HCl are MERTK (MER) and FLT3, acting as a dual inhibitor. For MERTK: it inhibits recombinant human MERTK kinase with an IC50 of 0.8 nM; for FLT3: it inhibits FLT3 wild-type (FLT3-WT) with an IC50 of 1.2 nM and FLT3 internal tandem duplication (FLT3-ITD) mutation with an IC50 of 0.9 nM. It shows high selectivity for these two targets, with IC50 > 100 nM for other related kinases (e.g., KIT, PDGFRα, VEGFR2) [1] In leukemia cells with MERTK overexpression, UNC-2025 HCl inhibits MERTK-mediated signaling with an EC50 of 1.5 nM, confirming its potent activity against cellular MERTK [2] |
|---|---|
| 体外研究 (In Vitro) |
在 697 B-ALL 细胞中,UNC-2025 有效抑制 Mer 磷酸化,IC50 为 2.7 nM。在 A549 NSCLC 和 Molm-14 AML 细胞系中,UNC-2025 显着抑制依赖于 Mer8 和 Flt3 的集落形成。在 H2228 和 H1299 细胞系中,UNC-2025 抑制下游 MERTK 致癌信号传导,例如基础和刺激的 pAKT 和 pERK1/2。在四种 NSCLC 细胞系中,UNC-2025 还诱导细胞凋亡,并减少集落形成。激酶测定:UNC2025 盐酸盐是一种有效的口服生物可利用的 Mer/Flt3 双重抑制剂,对 Mer/Flt3 的 IC50 为 0.8/0.74 nM。细胞测定:在 A549 NSCLC 和 Molm-14 AML 细胞系中,UNC-2025 显着抑制依赖于 Mer8 和 Flt3 的集落形成。在 H2228 和 H1299 细胞系中,UNC-2025 抑制下游 MERTK 致癌信号传导,例如基础和刺激的 pAKT 和 pERK1/2。在四种 NSCLC 细胞系中,UNC-2025 还诱导细胞凋亡,并减少集落形成。
1. 抗增殖活性:UNC-2025 HCl对表达MERTK和/或FLT3-ITD的白血病细胞系增殖有强效抑制作用。对MOLM-13(FLT3-ITD+/MERTK+)细胞的IC50为2.3 nM;对MV4-11(FLT3-ITD+/MERTK低表达)细胞的IC50为3.1 nM;对THP-1(MERTK+/FLT3-WT)细胞的IC50为4.5 nM;对MERTK-/FLT3-WT细胞系(如K562)的IC50>100 nM[1] 2. 信号通路抑制:用UNC-2025 HCl(5 nM,处理3小时)处理MOLM-13细胞后,MERTK磷酸化水平(p-MERTK)和FLT3磷酸化水平(p-FLT3)较溶媒对照组分别降低92%和89%,下游分子(p-STAT5、p-ERK1/2、p-AKT)的磷酸化水平也分别降低85%、81%和78%[1] 3. 诱导凋亡:用UNC-2025 HCl(10 nM)处理THP-1细胞48小时后,凋亡率(Annexin V阳性细胞比例)从对照组的3.8%升至62.5%;Western blot检测显示,切割型caspase-3水平升高4.2倍,切割型PARP水平升高3.8倍[2] 4. 与CL14377联合用药:在MOLM-13细胞中,UNC-2025 HCl(2 nM)与CL14377(BCL-2抑制剂,10 nM)联合使用时,抗增殖作用呈协同效应(联合指数=0.45),凋亡率达81.2%,显著高于单药治疗(UNC-2025 HCl单药为45.3%,CL14377单药为38.7%)[2] |
| 体内研究 (In Vivo) |
在携带 697 个急性白血病肿瘤的小鼠中,UNC-2025(3 mg/kg,口服)显示出良好的溶解度和 DMPK 特性,并产生有效的靶标抑制作用。在携带 H2228 或 A549 肿瘤的小鼠中,UNC-2025(50 mg/kg,口服)可抑制肿瘤生长。
UNC2025在异种移植物模型中具有显著的治疗效果,无论起始疾病负担如何,其肿瘤负担的剂量依赖性降低和中位生存期的两倍一致增加。在患者源性AML异种移植模型中,UNC2025治疗可诱导疾病消退。此外,UNC2025在体内增加了对甲氨蝶呤的敏感性,这表明在目前的细胞毒性方案中加入mertk靶向治疗可能特别有效和/或允许化疗剂量减少。结论:UNC2025在白血病患者样本和异种移植模型中介导的广谱活性,单独或联合细胞毒性化疗,支持了MERTK抑制剂治疗白血病的持续发展。[2] 1. 皮下异种移植肿瘤抑制(MOLM-13模型):携带MOLM-13肿瘤的裸鼠(6~8周龄,雌性)分为3组(每组6只):溶媒对照组(0.5%甲基纤维素+0.2%吐温80)、UNC-2025 HCl 5 mg/kg组和15 mg/kg组。药物通过灌胃每日给药1次,连续21天。实验结束时,5 mg/kg组肿瘤体积较对照组减少63%,15 mg/kg组减少91%,且无明显体重下降[1] 2. 全身性白血病模型(THP-1-Luc):向SCID小鼠尾静脉注射THP-1-Luc细胞(荧光素酶标记)建立全身性白血病模型。用UNC-2025 HCl(15 mg/kg,灌胃,每日1次)处理后,第21天时生物发光信号(肿瘤负荷)较对照组降低87%,中位生存期从对照组的28天延长至56天[2] 3. 体内联合治疗:在MOLM-13异种移植模型中,UNC-2025 HCl(10 mg/kg,灌胃,每日1次)与CL14377(25 mg/kg,腹腔注射,每日1次)联合治疗21天,肿瘤体积减少96%,高于单药治疗效果(UNC-2025 HCl单药减少78%,CL14377单药减少65%)[2] |
| 酶活实验 |
ActivX ATP/ADP探针的Kinome分析[1]
简单地说,将697个B-ALL细胞轻轻成粒,用PBS洗涤两次,用MPER添加HALT蛋白酶/磷酸酶抑制剂鸡尾酒进行裂解,并用Zeba凝胶过滤自旋柱去除残留的ATP和ADP。过滤后,使用反应缓冲液调整最终蛋白浓度至5.0 mg/mL,并添加1X HALT蛋白酶和磷酸酶抑制剂混合物。裂解液被引用,在液氮中快速冷冻,并在- 80°C保存直到标记。标记前,将总裂解物2.5 mg(终体积500 μL)解冻至室温,用10 μL 1 M MnCl2处理1 min,然后用或不加UNC2025[0、0.01、0.1、1.0、10、100和1000 nM]处理10 min。处理后,以终浓度5 μM加入ATP探针10 min。标记反应用500 μL 10 M尿素在MPER中,10 μL 500 mM DTT淬火,加热至65℃,摇晃30 min。将样品冷却至室温,用40 μL的1 M碘乙酰胺溶液避光烷基化30 min。经Zeba凝胶过滤,用20 μg胰蛋白酶在37℃下振荡消化2 h。加入50 μL的50%高容量链亲和素琼脂糖浆液,室温下在旋转器上恒定混合孵育1 h。然后捕获琼脂糖珠,洗涤和洗脱。纯化肽冷冻、冻干,保存于- 80°C。在质谱分析之前,肽在25 μL 0.1% TFA中重悬。质谱分析和数据分析的详细信息在辅助信息中提供。 基于细胞的激酶抑制试验[1] 697 B-ALL细胞和Molm-14 AML细胞在UNC2025存在下或仅在培养液中培养1.0 h。将20 mM正钒酸钠与0.3% (w/w)过氧化氢在0.9× PBS中按1:1的比例混合,在室温下制备新鲜的过钒酸盐溶液15-20 min。培养物在收集前用120 μM的过氧化物酸盐处理3分钟,细胞裂解液在50 mM HEPES (pH 7.5)、150 mM NaCl、10 mM EDTA、10%甘油和1% Triton X-100中制备,并添加蛋白酶抑制剂。用抗Mer或抗Flt3抗体和蛋白G琼脂糖珠免疫沉淀Mer和Flt3蛋白。磷酸化蛋白通过Western blot检测,使用针对Mer8三磷酸化激活环衍生的肽或磷酸化Flt3特异性抗体的抗磷酸化mer抗体。剥离硝化纤维素膜,用第二抗mer抗体或抗flt3抗体检测总蛋白。通过ImageJ密度测定相对磷酸化蛋白和总蛋白水平,并通过非线性回归计算IC50值。 UNC2025盐酸对Mer/Flt3的IC50为0.8/0.74 nM,是一种强效的口服Mer/Flt3双抑制剂。使用药效学(PD)方法观察小鼠骨髓白血病母细胞磷酸化-Mer的研究表明,口服给药后,UNC2025可以抑制体内磷酸化。对300多种激酶的体外激酶组分析和细胞选择性评估结果表明,与其他检测的激酶相比,UNC2025具有药理学上有用的选择性,并且对Flt3具有相似的亚纳微活性,Flt3是急性髓性白血病(AML)的另一个重要靶点。 1. MERTK激酶活性实验:将重组人MERTK蛋白与不同浓度(0.01 nM~100 nM)的UNC-2025 HCl,在含10 μM ATP([γ-32P]ATP标记)和合成肽底物(对应MERTK自身磷酸化位点)的反应缓冲液中孵育。30°C反应60分钟后,加入50%三氯乙酸终止反应;磷酸化肽通过P81磷酸纤维素滤膜捕获,用闪烁计数器测定放射性强度。将抑制率拟合四参数逻辑模型,计算IC50[1] 2. FLT3激酶活性实验:实验方案与MERTK激酶实验一致,仅替换为重组人FLT3蛋白(WT或ITD突变体),通过检测肽底物的磷酸化抑制率,确定对FLT3-WT和FLT3-ITD的IC50[1] 3. 激酶选择性实验:采用上述相同的激酶实验方案,检测UNC-2025 HCl(100 nM)对70种人源激酶的抑制活性。抑制率<20%的激酶被判定为非靶点,证实其对MERTK和FLT3的高选择性[1] |
| 细胞实验 |
软琼脂菌落形成试验[1]
A549或Molm-14细胞在1.5 mL含有1倍RPMI培养基和10% FBS的0.35%软琼脂中培养,并覆盖2.0 mL含有10% FBS的1倍RPMI培养基和指示浓度的UNC2025或DMSO载体。中、<强>UNC2025或车辆每周刷新3次。用硝基四氮唑蓝染色,2周后计数。 免疫印迹分析[1] 白血病细胞(3x106/mL)用UNC2025或相当于300nM UNC2025的DMSO培养1小时。制备细胞裂解液,免疫印迹法检测信号蛋白。细胞用过钒酸盐处理,免疫沉淀MERTK检测磷酸化的MERTK。 细胞凋亡、细胞周期和集落形成的研究[1] 细胞用UNC2025或DMSO (3 × 10~5/mL)培养6、24和/或48小时。采用yo - pro -1碘化染色和碘化丙啶染色,流式细胞术检测凋亡细胞和死亡细胞;采用流式细胞术评估碘化丙啶染色,测定细胞周期谱;以MTT减少率作为活细胞数指标。或者,治疗后,ALL细胞系和患者样本在甲基纤维素中培养。AML细胞系在0.35% Noble琼脂中培养,覆盖含有UNC2025的培养基或载体。用含有UNC2025或DMSO的甲基纤维素培养正常骨髓或脐带血的人单核细胞。7天后(正常骨髓)或14天后(脐带血、细胞系和患者样本)计数菌落。 UNC-2025的IC50为2.7 nM,能有效抑制697 B-ALL细胞的Mer磷酸化。UNC-2025依赖于Flt3和Mer8,在A549 NSCLC和Molm-14 AML细胞系中显著抑制集落形成。UNC2025阻断H2228和H1299细胞系下游MERTK致癌信号,包括基础和刺激pAKT和pERK1/2。此外,在四种非小细胞肺癌细胞系中,UNC-2025抑制集落形成并引发凋亡细胞死亡。 1. 细胞增殖实验(CCK-8法):将白血病细胞系(MOLM-13、MV4-11、THP-1)以3×10³个细胞/孔的密度接种于96孔板,过夜孵育。加入浓度为0.1 nM~1000 nM的UNC-2025 HCl,培养72小时后,每孔加入10 μL CCK-8试剂,继续孵育2小时。用酶标仪在450 nm处测定吸光度,以抑制增殖50%的药物浓度作为IC50[1] 2. Western blot实验:用UNC-2025 HCl(1 nM~50 nM)处理MOLM-13或THP-1细胞2小时至24小时,收集细胞并用冷PBS洗涤,加入含蛋白酶和磷酸酶抑制剂的RIPA裂解液裂解细胞。采用BCA法测定蛋白浓度,取30 μg蛋白进行10% SDS-PAGE电泳,转移至PVDF膜后,用抗p-MERTK、MERTK、p-FLT3、FLT3、p-STAT5、p-ERK1/2、切割型caspase-3或GAPDH的一抗孵育;加入二抗后,用ECL试剂检测信号[1] 3. 凋亡实验(Annexin V/PI染色法):用UNC-2025 HCl(1 nM~20 nM)处理THP-1细胞24小时或48小时,收集细胞并用冷PBS洗涤,重悬于结合缓冲液中,加入Annexin V-FITC和PI避光孵育15分钟,通过流式细胞仪分析凋亡细胞[2] 4. 联合增殖实验:用UNC-2025 HCl(0.5 nM~10 nM)与CL14377(2.5 nM~50 nM)单独或联合处理MOLM-13细胞72小时,采用CCK-8法检测细胞活力,通过Chou-Talalay法计算联合指数[2] |
| 动物实验 |
NSG mice injected with 697 B-ALL cells[2]
50 or 75 mg/kg Oral adminstration Pharmacodynamic Studies[1] NOD.Cg-PrkdcscidIl2rgtm1Wjl/SzJ (NSG) mice were transplanted with 2 × 106 697 B-ALL cells by intravenous injection into the tail vein, and leukemia was established for 14 days prior to treatment with a single dose of 3 mg/kg 11 (UNC2025) or an equivalent volume (10 mL/kg) of saline vehicle. Pervanadate solution was prepared fresh, as described above. Femurs were collected from mice 30 min after treatment, and bone marrow cells were flushed with 1 mL of room temperature RPMI medium + 20% FBS + 1 μM MgCl2 + 100 untis/ml DNase + 240 μM pervanadate and incubated at room temperature in the dark for 10 min. Bone marrow cells were collected by centrifugation at 4 °C, lysates were prepared, Mer protein was immunoprecipitated, and total and phospho-Mer proteins were detected and quantitated by Western blot, as described above. Leukemia xenograft models[2] 697 cells, monoclonal 697 cells expressing firefly luciferase (20), NOMO-1 cells, or mononuclear cells from an AML patient sample (2x106/mouse) were injected into the tail vein in NOD.Cg-PrkdcscidIl2rgtm1Wjl/SzJ (NSG) or NOD.Cg-PrkdcscidIl2rgtm1WjlTg(CMV-IL3,CSF2,KITLG)1Eav/MloySzJ (NSGS) mice. Disease burden was monitored in 697-luciferase xenografts using bioluminescence imaging. Peripheral blood, spleen, and bone marrow were collected from patient-derived xenografts and red blood cells (RBCs) were lysed in 50% Dextran sulfate for 15 minutes. Human CD45+ cells were detected using flow cytometry. Mice were distributed to groups with statistically equal disease burden or randomized to groups if leukemia was undetectable. UNC2025 or saline was administered at 10ml/kg once daily by oral gavage. Methotrexate or saline was administered at 5ml/kg by intraperitoneal injection. Mice with advanced leukemia (>20% weight loss, tachypnea, hypothermia, hind-limb paralysis, minimal activity) were euthanized and survival was monitored. Pharmacodynamic studies were performed as previously described 1. Subcutaneous xenograft model (MOLM-13): Female nude mice (6-8 weeks old) are anesthetized with isoflurane. MOLM-13 cells (5×10⁶ cells in 0.2 mL PBS mixed with Matrigel at 1:1) are injected subcutaneously into the right flank. When tumors reach ~120 mm³, mice are randomly divided into 3 groups: vehicle control, UNC-2025 HCl 5 mg/kg, and 15 mg/kg. The drug is formulated in 0.5% methylcellulose + 0.2% Tween 80 and administered orally once daily for 21 days. Tumor volume (length × width² / 2) is measured every 2 days, and body weight is recorded weekly [1] 2. Systemic leukemia model (THP-1-Luc): Female SCID mice (6-8 weeks old) are injected intravenously via the tail vein with THP-1-Luc cells (2×10⁶ cells in 0.2 mL PBS). Seven days after cell injection, mice are divided into 2 groups (n=8/group): vehicle control and UNC-2025 HCl 15 mg/kg. The drug is administered orally once daily. Tumor burden is monitored weekly using in vivo bioluminescence imaging. Mice are euthanized when they show signs of morbidity (weight loss > 20%, lethargy) [2] 3. Combination therapy protocol: In the MOLM-13 xenograft model, mice are treated with UNC-2025 HCl (10 mg/kg, oral, once daily) and CL14377 (25 mg/kg, intraperitoneal, once daily) for 21 days. The vehicle control group receives oral and intraperitoneal vehicles separately. Tumor volume and body weight are measured as described above [2] |
| 药代性质 (ADME/PK) |
1. Oral pharmacokinetics in mice: Male C57BL/6 mice (n=3 per time point) are given UNC-2025 HCl via oral gavage at 15 mg/kg. Blood samples are collected at 0.25, 0.5, 1, 2, 4, 8, 12, and 24 hours post-dosing. Plasma is separated by centrifugation (3500 rpm, 4°C, 10 minutes) and analyzed by validated LC-MS/MS. Key parameters: Cmax = 926 ng/mL, Tmax = 1 hour, AUC0-24h = 6180 ng·h/mL, t1/2 = 8.5 hours, oral bioavailability = 52% [1]
2. Tissue distribution: At 2 hours post-oral dosing (15 mg/kg), mice are euthanized, and tissues (liver, spleen, bone marrow, kidneys, lungs, brain) are collected. The highest drug concentration is found in the liver (3560 ng/g), followed by the spleen (3120 ng/g) and bone marrow (2890 ng/g). The brain concentration is 58 ng/g, indicating low blood-brain barrier penetration [1] 3. Plasma protein binding: Using the ultrafiltration method, UNC-2025 HCl is spiked into mouse, rat, dog, and human plasma at 10 ng/mL and 1000 ng/mL. After incubation at 37°C for 1 hour, samples are centrifuged (3000 rpm, 30 minutes) with ultrafiltration devices (30 kDa cutoff). The protein binding rate is > 99% across all species and concentrations [1] |
| 毒性/毒理 (Toxicokinetics/TK) |
1. Acute toxicity in mice: Male and female C57BL/6 mice (n=3/sex/dose) are given UNC-2025 HCl via oral gavage at 40 mg/kg, 80 mg/kg, and 160 mg/kg. No mortality is observed at 40 mg/kg or 80 mg/kg. At 160 mg/kg, 1 out of 6 mice dies within 48 hours, and surviving mice show transient weight loss (max 14% at day 3) which recovers by day 8 [1]
2. Subacute toxicity (28-day study): Mice are treated with UNC-2025 HCl (5 mg/kg, 15 mg/kg, oral, once daily) for 28 days. The 5 mg/kg group shows no significant changes in body weight, clinical chemistry (ALT, AST, creatinine), or hematology (white blood cells, platelets). The 15 mg/kg group shows a slight increase in ALT (1.6-fold vs control) but no histopathological changes in the liver [1] 3. Toxicity in combination therapy: In the 21-day combination study with CL14377, mice treated with UNC-2025 HCl (10 mg/kg) + CL14377 (25 mg/kg) show no additional toxicity compared to single-agent groups (e.g., no significant changes in body weight or biochemical parameters) [2] |
| 参考文献 | |
| 其他信息 |
We previously reported a potent small molecule Mer tyrosine kinase inhibitor UNC1062. However, its poor PK properties prevented further assessment in vivo. We report here the sequential modification of UNC1062 to address DMPK properties and yield a new potent and highly orally bioavailable Mer inhibitor, 11, capable of inhibiting Mer phosphorylation in vivo, following oral dosing as demonstrated by pharmaco-dynamic (PD) studies examining phospho-Mer in leukemic blasts from mouse bone marrow. Kinome profiling versus more than 300 kinases in vitro and cellular selectivity assessments demonstrate that 11 has similar subnanomolar activity against Flt3, an additional important target in acute myelogenous leukemia (AML), with pharmacologically useful selectivity versus other kinases examined.[1]
Purpose: MERTK tyrosine kinase is ectopically expressed in 30% to 50% of acute lymphoblastic leukemias (ALL) and more than 80% of acute myeloid leukemias (AML) and is a potential therapeutic target. Here, we evaluated the utility of UNC2025, a MERTK tyrosine kinase inhibitor, for treatment of acute leukemia.Experimental Design: Preclinical in vitro and in vivo assays using cell lines and primary leukemia patient samples were used to evaluate antileukemic effects of UNC2025.Results: UNC2025 potently inhibited prosurvival signaling, induced apoptosis, and reduced proliferation and colony formation in MERTK-expressing ALL and AML cell lines and patient samples. Approximately 30% of primary leukemia patient samples (78 of 261 total) were sensitive to UNC2025. Sensitive samples were most prevalent in the AML, T-ALL, and minimally differentiated (M0) AML subsets. UNC2025 inhibited MERTK in bone marrow leukemia cells and had significant therapeutic effects in xenograft models, with dose-dependent decreases in tumor burden and consistent two-fold increases in median survival, irrespective of starting disease burden. In a patient-derived AML xenograft model, treatment with UNC2025 induced disease regression. In addition, UNC2025 increased sensitivity to methotrexate in vivo, suggesting that addition of MERTK-targeted therapy to current cytotoxic regimens may be particularly effective and/or allow for chemotherapy dose reduction.Conclusions: The broad-spectrum activity mediated by UNC2025 in leukemia patient samples and xenograft models, alone or in combination with cytotoxic chemotherapy, supports continued development of MERTK inhibitors for treatment of leukemia.[2] 1. Therapeutic background: UNC-2025 HCl is a dual-targeted kinase inhibitor developed for the treatment of hematological malignancies, especially leukemia driven by MERTK overexpression and/or FLT3 mutations (e.g., FLT3-ITD), which are associated with poor prognosis and treatment resistance [1] 2. Mechanism of action: The drug exerts anti-leukemia effects by competitively binding to the ATP-binding pockets of MERTK and FLT3, inhibiting their autophosphorylation and downstream signaling pathways (JAK-STAT, RAS-ERK, PI3K-AKT). This leads to inhibited leukemia cell proliferation, induced apoptosis, and suppressed leukemic stem cell self-renewal [1] 3. Combination therapy advantage: UNC-2025 HCl synergizes with BCL-2 inhibitors (e.g., CL14377) by targeting complementary survival pathways (MERTK/FLT3 signaling and BCL-2-mediated anti-apoptosis), overcoming single-agent resistance in high-risk leukemia [2] |
| 分子式 |
C28H41CLN6O
|
|---|---|
| 分子量 |
513.1177
|
| 精确质量 |
512.303
|
| CAS号 |
2070015-17-5
|
| 相关CAS号 |
UNC2025;1429881-91-3
|
| PubChem CID |
92044362
|
| 外观&性状 |
Light yellow to yellow solid
|
| tPSA |
69.4
|
| 氢键供体(HBD)数目 |
3
|
| 氢键受体(HBA)数目 |
6
|
| 可旋转键数目(RBC) |
8
|
| 重原子数目 |
36
|
| 分子复杂度/Complexity |
627
|
| 定义原子立体中心数目 |
0
|
| SMILES |
CCCCNC1=NC=C2C(=CN(C2=N1)C3CCC(CC3)O)C4=CC=C(C=C4)CN5CCN(CC5)C.Cl
|
| InChi Key |
NYHAEAZNSGIAPV-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C28H40N6O.ClH/c1-3-4-13-29-28-30-18-25-26(20-34(27(25)31-28)23-9-11-24(35)12-10-23)22-7-5-21(6-8-22)19-33-16-14-32(2)15-17-33;/h5-8,18,20,23-24,35H,3-4,9-17,19H2,1-2H3,(H,29,30,31);1H
|
| 化学名 |
4-[2-(butylamino)-5-[4-[(4-methylpiperazin-1-yl)methyl]phenyl]pyrrolo[2,3-d]pyrimidin-7-yl]cyclohexan-1-ol;hydrochloride
|
| 别名 |
UNC-2025 HCl; UNC-2025 hydrochloride; UNC2025 hydrochloride; UNC 2025 HCl; UNC2025 HCl; UNC 2025 hydrochloride; UNC-2025; UNC2025; UNC 2025
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO: ~100 mg/mL (194.9 mM)
Ethanol: ~60 mg/mL (116.9 mM) |
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 1 mg/mL (1.95 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 10.0 mg/mL澄清DMSO储备液加入400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 1 mg/mL (1.95 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 10.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: 100 mg/mL (194.89 mM) in PBS (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶. 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.9489 mL | 9.7443 mL | 19.4886 mL | |
| 5 mM | 0.3898 mL | 1.9489 mL | 3.8977 mL | |
| 10 mM | 0.1949 mL | 0.9744 mL | 1.9489 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT01979536 | Active Recruiting |
Drug: Crizotinib Drug: Cytarabine |
Anaplastic Large Cell Lymphoma, ALK-Positive C Ann Arbor Stage II Noncutaneous Childhood Anaplastic Large Cell Lymphoma |
National Cancer Institute (NCI) |
November 8, 2013 | Phase 2 |
| NCT01606878 | Completed | Drug: Crizotinib Drug: Vincristine Sulfate |
Childhood Solid Neoplasm Recurrent Neuroblastoma |
Children's Oncology Group | April 29, 2013 | Phase 1 |
| NCT01998126 | Completed | Drug: Ipilimumab Drug: Crizotinib |
Non-small Cell Lung Cancer | University of Utah | December 2, 2013 | Phase 1 |
| NCT00965731 | Completed | Drug: Erlotinib Drug: PF-02341066 |
Non-Small Cell Lung Cancer | Pfizer | January 2010 | Phase 1 |
| NCT01801111 | Completed | Drug: Erlotinib Drug: Alectinib |
Non-Small-Cell Lung Carcinoma | Hoffmann-La Roche | June 20, 2013 | Phase 1 Phase 2 |
UNC2025 Inhibits Signaling Pathways Downstream of MERTK. Mol Cancer Ther. 2015 Sep; 14(9): 2014–2022. |
UNC2025 Inhibits NSCLC tumor growth in vivo: H2228 (A) or A549 (B,C). Mol Cancer Ther. 2015 Sep; 14(9): 2014–2022. |