| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5g |
|
||
| 10g |
|
||
| 25g |
|
||
| 50g |
|
||
| 100g |
|
||
| Other Sizes |
|

| 靶点 |
Influenza A viruses; ion channels NMDA, M2; CDK2; Bcl-2; Bax
|
|---|---|
| 体外研究 (In Vitro) |
盐酸金刚烷胺 (0-500 μM,26 小时) 抑制 SARS-CoV-2 复制,IC50 浓度在 83 和 119 μM 之间[4]。 盐酸金刚烷胺 (0-100 μg/mL,24-72 h) 显着抑制 HepG2。盐酸金刚烷胺 (0-75 μg/mL,48 h) 将细胞周期阻滞在 G0/G1 期并诱导细胞的肿胀[6]。 盐酸金刚烷胺 (0-75 μg) 和 SMMC-7721 细胞的肿胀[6]。 /mL,48 h) 可降低细胞周期相关基因和蛋白(cyclin D1、cyclin E 和 CDK2),减少 Bcl-2 并增加 Bax 蛋白和 mRNA 水平[6]。 Cell Viability Assay[4] Cell Line: Vero E6细胞浓度:500 µM、100 µM、20 µM、4 µM 和 8 nM 孵育时间:26 小时 结果:10 ℃感染 26 小时后,导致上清液中病毒核酸浓度依赖性减少(IC50=83 µM) -500 µM。感染后 26 小时,导致细胞质中病毒核酸浓度依赖性减少 (IC50=119 µM)。细胞增殖测定[6] 细胞系:人 HCC 细胞系(HepG2 和 SMMC-7721)和正常肝细胞(L02 细胞) 浓度:0、1、2、5、10、25、50 和 100 µg/mL 孵育时间:24、48 和 72 小时 结果:在 HepG2 和 SMMC-7721 细胞中以时间和剂量依赖性方式抑制细胞增殖。细胞周期分析[6] 细胞系:HepG2 和 SMMC-7721 细胞 浓度:0、10、25、50 和 75 µg/mL 孵育时间:48 小时 结果:G0 期 HepG2 和 SMMC-7721 细胞数量显着增加/G1期呈剂量依赖性,并显着减少S期HepG2细胞的数量。细胞凋亡分析[6] 细胞系:HepG2 和 SMMC-7721 细胞 浓度:0、10、25、50 和 75 µg/mL 孵育时间:48 小时 结果:凋亡 HepG2 和 SMMC-7721 细胞的百分比显着增加(早期-和晚期细胞凋亡)以剂量依赖性方式。 Western Blot 分析[6] 细胞系:HepG2 和 SMMC-7721 细胞 浓度:0、10、25、50 和 75 µg/mL 孵育时间:48 h 结果:显示 cyclin D1、cyclin E 和 CDK2 下调,并显示HepG2 和 SMMC-7721 细胞中 Bcl-2 水平降低,Bax 水平升高。 RT-PCR[6] 细胞系:HepG2 和 SMMC-7721 细胞 浓度:0、10、25、50 和 75 µg/mL 孵育时间:48 小时 结果:显示 Bax 增加,Bcl-2 基因减少。
金刚烷胺(0-500 µM,26 小时)抑制 SARS-CoV-2 复制的 IC50 值范围为 83 至 119 µM [4]。金刚烷胺(0-100 µg/mL,24-72 小时)强烈抑制 HepG2 和 SMMC-7721 细胞生长 [6]。金刚烷胺(0-75 µg/mL,48 小时)会导致细胞凋亡并使细胞周期停止在 G0/G1 期 [6]。金刚烷胺(0-75 µg/mL,48 小时)可降低 Bcl-2,增加 Bax 蛋白和 mRNA 水平,并降低细胞周期相关基因和蛋白(细胞周期蛋白 D1、细胞周期蛋白 E 和 CDK2)[6]。 自2019年底严重急性呼吸系统综合征冠状病毒2型疫情开始以来,寻找保护性疫苗和药物治疗已成为应对全球卫生紧急情况的强制性措施。旅行限制、社交距离和口罩是合适的应对措施,但可能无法控制疫情,因为人们会无意中或在一定程度的限制严重程度或持续时间内不遵守规定。即使疫苗获得批准,对抗严重急性呼吸系统综合征冠状病毒2型的抗病毒药物的需求也将持续存在。然而,迄今为止,尚未有明确证据表明任何重新使用的抗病毒药物对严重急性呼吸系统综合征冠状病毒2型有疗效金刚烷胺已被批准为抗甲型流感的抗病毒药物,对严重急性呼吸系统综合征冠状病毒2型的抗病毒活性已通过类比得出,但没有数据。我们在体外测试了金刚烷胺对感染严重急性呼吸系统综合征冠状病毒2型的Vero E6细胞的疗效。事实上,金刚烷胺在两个单独的实验中抑制了严重急性呼吸系统综合征冠状病毒2型的复制,IC50浓度在83至119µM之间。尽管这些IC50浓度在全身给药后高于治疗性金刚烷胺水平,但通过吸入或鼻内滴注局部给药可能会导致气道上皮中金刚烷胺浓度充足,而不会产生高全身暴露。然而,需要在其他模型中进行进一步的研究来证明这一假设。[4] 肝细胞癌(HCC)是全球最具侵袭性的恶性肿瘤之一,近年来与病毒感染相关的发病率有所增加金刚烷胺是一种三环对称胺,可以有效预防丙型肝炎病毒。然而,其抗肿瘤特性尚不清楚。本研究探讨了金刚烷胺对肿瘤细胞存活率、细胞周期调控和凋亡的影响。MTT法检测HepG2和SMMC-7721细胞(HCC细胞系)的生长情况。流式细胞术用于研究细胞周期调控和凋亡。还进行了逆转录定量聚合酶链式反应和蛋白质印迹分析,以检测细胞周期和凋亡相关基因和蛋白质的表达,包括细胞周期蛋白E、细胞周期蛋白D1、细胞周期素依赖性激酶2(CDK2)、B细胞淋巴瘤2(Bcl-2)和Bax。我们的研究结果表明,金刚烷胺以剂量和时间依赖的方式显著抑制HepG2和SMMC-7721细胞的增殖,并将细胞周期阻滞在G0/G1期。金刚烷胺降低了细胞周期相关基因和蛋白质(细胞周期蛋白D1、细胞周期蛋白E和CDK2)的水平,并显著诱导了细胞凋亡。金刚烷胺治疗还降低了Bcl-2,增加了Bax蛋白和mRNA水平。此外,金刚烷胺治疗后,两种HCC细胞系的Bcl-2/Bax比值较低。总的来说,这些结果强调了金刚烷胺在抑制HCC细胞增殖和诱导凋亡方面的作用,主张将其作为一种新型的肿瘤抑制治疗候选药物[6]。 |
| 体内研究 (In Vivo) |
盐酸金刚烷胺(25 mg/kg,IP,每天一次,持续3天)抑制调节引起的神经调节和学习记忆障碍[5]。 动物模型:Fischer 344大鼠(4月龄,雄性,290-330 g,每组15只大鼠)[5] 剂量:25 mg/kg 给药方式:IP,每日一次,连续3天(手术前15分钟第一次给药) 结果:抑制手术引起的神经炎症和学习记忆障碍,增加GDNF(胶质细胞)线源性神经营养因子)与海马体中的神经胶质原纤维酸性蛋白(星形细胞标记物)共定位。
金刚烷胺(25 mg/kg,IP,每天一次,持续 3 天)可减少手术引起的神经炎症以及学习和记忆缺陷 [5]。 在训练后1天或8天进行测试时,手术增加了在巴恩斯迷宫中识别目标框的时间[22(中位数)(11-66)(四分位数间距)对照组对158(29-180)手术组,n=15,P=0.022),并减少了恐惧条件测试中与背景相关的冷冻行为。这些影响被金刚烷胺和侧脑室GDNF减弱。金刚烷胺增加了与星形胶质细胞标志物胶质纤维酸性蛋白共定位的GDNF。海马。侧脑室注射抗GDNF抗体而不是变性抗体阻断了金刚烷胺对认知的影响。手术诱导的神经炎症被金刚烷胺抑制。脂多糖增加了C8-B4细胞白细胞介素1β的产生。这种作用被GDNF抑制[5]。 金刚烷胺减轻了手术引起的学习记忆障碍[5] 随着对照组大鼠、仅接受麻醉的大鼠、只接受Amantadine金刚烷胺的大鼠和接受手术加金刚烷胺的大鼠训练时间的增加,巴恩斯迷宫试验4天训练期间识别目标框的时间缩短了。这四组大鼠在第4天的时间明显短于第1天。这种效果在单独手术后的大鼠身上并不明显。手术对训练课程中识别目标框所需的时间有显著影响[F(1,28)=5.625,P=0.025]。金刚烷胺可消除这种作用[F(1,28)=0.840,P=0.367;与对照组相比]。金刚烷胺或麻醉对训练期间识别目标框的时间没有显著影响[F(1,28)=0.063,P=0.804;F(1,14)=0.074,P+0.790](图1和图2)。当在训练课程后1天对大鼠进行测试时,接受手术的大鼠识别目标框的时间比对照组大鼠长。金刚烷胺可以减轻这种延长。在训练课程结束8天后进行测试时,也出现了类似的变化模式。然而,无论测试是在训练后1天还是8天进行,单独使用麻醉和金刚烷胺都不会影响识别目标框的时间(图1B和2B)。 与对照组大鼠相比,手术组大鼠(而非仅麻醉组或金刚烷胺组大鼠)在恐惧条件反射测试中的情境相关冷冻行为较少。金刚烷胺消除了这种手术效果(图1C)。对照组、接受金刚烷胺治疗的大鼠、接受手术的大鼠和接受手术加金刚烷胺的大鼠在音调相关的冷冻行为方面没有差异(图1C和2C)。 金刚烷胺减轻了手术引起的神经炎症[5] 术后6小时和24小时,海马中Iba-1(一种小胶质细胞标志物)、IL-1β和IL-6的表达显著增加。Amantadine金刚烷胺消除了这些增加(图3和图4)。同样,手术后10天,海马齿状回区域的Iba-1表达也增加,这种增加被金刚烷胺阻断(图5)。这些结果表明,手术诱导了金刚烷胺抑制的神经炎症。 金刚烷胺增加了抑制小胶质细胞活化的GDNF的表达[5] 金刚烷胺/Amantadine显著增加了海马中的GDNF(图7)。GDNF主要与星形胶质细胞标志物GFAP共定位,但与Iba-1不共定位(图7A和7B)。一些GDNF似乎位于神经元标记物NeuN周围(图7C)。手术也增加了GFAP,但这种增加不受海马中金刚烷胺的影响(图7A和7E)。 抗GDNF抗体可抑制金刚烷胺诱导的术后学习记忆障碍的减弱[5] 与对照组大鼠相似,仅抗体组和手术加金刚烷胺/Amantadine加煮沸抗体组的大鼠找到目标框的时间缩短,训练次数增加。这两组大鼠在训练第4天的时间比训练第1天的时间短。对于手术加金刚烷胺加抗GDNF抗体组的大鼠来说,这种效果并不明显。研究发现,抗GDNF抗体对训练期间识别目标框的时间有显著影响[F(1,14)=19.009,P<0.001;与对照组相比)(图9A)。训练后第1天识别目标框所需的时间在对照组大鼠、接受抗体的大鼠、接受手术加金刚烷胺加抗-GDNF抗体或接受手术加金刚烷基胺加煮沸抗体的大白鼠之间没有差异。然而,接受手术加金刚烷胺加抗-DDNF抗体的大老鼠在训练后第8天需要比对照组大白鼠或接受手术加金刚烷胺加煮沸抗体的老鼠更长的时间来识别目标框(图9B)。 同样,在恐惧条件测试中,接受手术加金刚烷胺加抗GDNF抗体的大鼠也比对照组大鼠或接受手术加金刚烷胺加煮沸抗体的大白鼠有更少的与环境相关的冷冻行为。然而,三组之间与音调相关的冷冻行为没有差异(图9C)。 |
| 酶活实验 |
S-蛋白-ACE2结合试验[4]
使用严重急性呼吸系统综合征冠状病毒2型刺突:ACE2抑制剂筛选试剂盒测试化合物抑制严重急性呼吸系综合征冠状病毒2中刺突蛋白(S蛋白)与ACE2结合的能力。简而言之,将严重急性呼吸系统综合征冠状病毒2型刺突蛋白以1µg/mL的磷酸盐缓冲盐水包被到96微孔板上。去除未结合的蛋白质,并阻断孔中的非特异性结合位点。然后,去除阻断溶液,将稀释的化合物和对照样品加入孔中。将包被的刺突蛋白与化合物预孵育后,加入His标记的ACE2蛋白,并与化合物一起孵育,以允许与刺突蛋白结合。洗涤和阻断后,用与辣根过氧化物酶(HRP)偶联的抗His抗体检测结合的ACE2蛋白。使用化学发光HRP底物进行检测,并在微量滴定板读数器中读取发光强度。将含有稀释化合物的每个样品的发光信号除以不存在任何抑制剂时的发光,并将所得值与化合物浓度绘制成图。 RT-PCR读数抗病毒活性测定(第一次实验)[4] 将指数增长的Vero E6细胞以每孔8×104个细胞的密度接种到48孔板中,并孵育过夜。取出培养基,用严重急性呼吸系统综合征冠状病毒2型(hCoV-19/意大利/INMI1 isl/2020,MOI为0.01,在含有不同抑制剂浓度的300µL培养基中)感染细胞三次。将Amantadine金刚烷胺溶解在无菌水中,并用培养基进一步稀释至500µM、100µM、20µM、4µM和8 nM的浓度。将雷德西韦溶解在DMSO中,用培养基稀释至50µM、10µM、2µM、0.4µM和80 nM的剂量。雷德西维尔MOCK对照品含有不同量的DMSO。 用核衣壳蛋白读数进行抗病毒活性测定(第二次实验)[4] 将指数增长的Vero E6细胞在完全培养基中以最佳密度接种到96孔板中;24小时后,细胞以0.01 moi(多重感染)感染严重急性呼吸系统综合征冠状病毒2型(病毒株INMI1),然后暴露于不同浓度的药物(0-0.1-1-10-100-300μM的Amantadine/金刚烷胺)72小时。在培养基中进行药物稀释。检查每个浓度点的复制品。在潜伏期结束时,通过ELISA(定量严重急性呼吸系综合征冠状病毒-2核蛋白)和细胞保护试验(通过倒置显微镜检查毒性效应)检查抗病毒活性。 |
| 细胞实验 |
细胞活力测定[4]
细胞类型: Vero E6 细胞 测试浓度: 500 µM、100 µM、20 µM、4 µM 和 8 nM 孵育持续时间: 26 小时 实验结果:导致病毒浓度依赖性减少 (IC50=83 µM) 26 感染后上清液中的核酸浓度为10-500 µM。导致感染后 26 小时细胞质中病毒核酸浓度依赖性减少 (IC50=119 µM)。 细胞增殖测定[6] 细胞类型:人 HCC 细胞系(HepG2 和 SMMC-7721)和正常肝细胞(L02 细胞) 测试浓度:0、1、2、5、10、25、50 和 100 µg/mL 孵育时间:24、48 和 72 小时 实验结果:在HepG2和SMMC-7721细胞中以时间和剂量依赖性方式抑制细胞增殖。 细胞周期分析[6] 细胞类型: HepG2 和 SMMC-7721 细胞 测试浓度: 0、10、25、 50 和 75 µg/mL 孵育持续时间:48 小时 实验结果:HepG2 和 SMMC- 数量显着增加7721细胞以剂量依赖性方式处于G0/G1期,并且数量急剧减少 |
| 动物实验 |
Fischer 344 rats (Four-month old, male, 290-330 g, 15 rats each group)
25 mg/kg Administration: IP, once daily for 3 days (the first dose at 15 min before surgery) Animal/Disease Models: Fischer 344 rats (4 months old, male, 290-330 g, 15 rats per group) [5] Doses: 25 mg/kg Route of Administration: IP, one time/day for 3 days (first dose in 15 minutes before administration) Experimental Results: Inhibited surgery-induced neuroinflammation and learning and memory impairment, increased GDNF (glial cell line-derived neuronal neuron) co-localized with hippocampal glial fibrillary acidic protein (an astrocyte marker) nutritional factors). Four-month old male Fischer 344 rats weighing 290 – 330 g were randomly assigned to: 1) control group (not being exposed to surgery or any drugs), 2) Amantadine group, 3) surgery group (right carotid artery exposure), and 4) surgery plus Amantadine group in the first experiment. Each group had 15 rats. In the second experiment, the rats were assigned to: 5) control group, 6) anti-GDNF antibody group, 7) surgery plus amantadine plus boiled anti-GDNF antibody group, and 8) surgery plus amantadine plus anti-GDNF antibody group. Each group had 8 rats. In the third experiment, the rats were randomly assigned to: 7) control group, 8) anesthesia only group, and 9) surgery plus GDNF group. Each group had 8 rats. GDNF and the anti-GDNF antibody were injected intracerebroventricularly. One week later, these rats were started to be tested in Barnes maze and then fear conditioning. Separate rats were assigned to 1) control group, 2) surgery group, and 3) surgery plus amantadine group (n = 6 per condition) and sacrificed at 6 h, 24 h or 10 days after the surgery for Western blotting and immunohistochemistry. Amantadine was dissolved in normal saline and injected intraperitoneally at 25 mg/kg/day for three days with the first dose at 15 min before surgery. Similar injections were performed in the amantadine only group except that no surgery and anesthesia were performed. The amantadine dose was chosen based on previous studies.[5] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Amantadine is well absorbed orally from the gastrointestinal tract. It is primarily excreted unchanged in the urine by glomerular filtration and tubular secretion. 3 to 8 L/kg [healthy subjects] 0.2 - 0.3 L/hr/kg 0.10 +/- 0.04 L/hr/kg [healthy, elderly male] Rapidly and almost completely absorbed from gastrointestinal tract. Amantadine is distributed into breast milk. Elimination: Renal; >90% excreted unchanged in urine by glomerular filtration and renal tubular secretion. Rate of excretion rapidly increased in acid urine. In dialysis: Only small amounts (approximately 4%) removed from the blood by hemodialysis. Distributed into saliva, tear film, and nasal secretions; in animals, tissue (especially lung) concentrations are higher than serum concentrations. Crosses the placenta and blood-brain barrier; distributed into breast milk. Cerebral spinal fluid concentrations were 52% of corresponding plasma concentrations in one patient. VolD - 4.4 + or - 0.2 L/kg (normal renal function); 5.1 + or - 0.2 L/kg (renal failure). For more Absorption, Distribution and Excretion (Complete) data for AMANTADINE (7 total), please visit the HSDB record page. Metabolism / Metabolites No appreciable metabolism, although negligible amounts of an acetyl metabolite have been identified. Eight metabolites of amantadine have been identified in human urine. One metabolite, an N-acetylated compound, was quantified in human urine and accounted for 5-15% of the administered dose. Plasma acetylamantadine accounted for up to 80% of the concurrent amantadine plasma concentration in 5 of 12 healthy volunteers following the ingestion of a 200 mg dose of amantadine. Acetylamantadine was not detected in the plasma of the remaining seven volunteers.. No appreciable metabolism, although negligible amounts of an acetyl metabolite have been identified. Amantadine is well absorbed orally from the gastrointestinal tract. The mechanism of its antiparkinsonic effect is not fully understood, but it appears to be releasing dopamine from the nerve endings of the brain cells, together with stimulation of norepinephrine response. The antiviral mechanism seems to be unrelated. The drug interferes with a viral protein, M2 (an ion channel), which is needed for the viral particle to become "uncoated" once it is taken inside the cell by endocytosis. Metabolites are excreted in the urine (A308). Route of Elimination: It is primarily excreted unchanged in the urine by glomerular filtration and tubular secretion. Half Life: Mean half-lives ranged from 10 to 14 hours, however renal function impairment causes a severe increase in half life to 7 to 10 days. Biological Half-Life Mean half-lives ranged from 10 to 14 hours, however renal function impairment causes a severe increase in half life to 7 to 10 days. Amantadine pharmacokinetics were determined in 24 normal adult male volunteers after the oral administration of a single amantadine hydrochloride 100 mg soft gel capsule. ... The half-life was 17 + or - 4 hours (range: 10 to 25 hours). Across other studies, amantadine plasma half-life has averaged 16 + or - 6 hours (range: 9 to 31 hours) in 19 healthy volunteers. Normal renal function: 11 to 15 hours. Elderly patients: 24 to 29 hours. Renal function impairment, severe: 7 to 10 days. Hemodialysis: 24 hours. The elimination half-life increases two to three fold or greater when creatinine clearance is less than 40 mL/min/1.73 sqm and averages eight days in patients on chronic maintenance hemodialysis. |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
The mechanism of its antiparkinsonic effect is not fully understood, but it appears to be releasing dopamine from the nerve endings of the brain cells, together with stimulation of norepinephrine response. It also has NMDA receptor antagonistic effects. The antiviral mechanism seems to be unrelated. The drug interferes with a viral protein, M2 (an ion channel), which is needed for the viral particle to become "uncoated" once it is taken inside the cell by endocytosis. Hepatotoxicity Despite widespread use, there is little evidence that amantadine when given orally causes liver injury, either in the form of serum enzyme elevations or clinically apparent liver disease. Likelihood score: E (unlikely cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation It is probably best to avoid amantadine during breastfeeding because of its potential negative effect on lactation. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Amantadine is a dopamine agonist. Clinical studies using amantadine dosages of 100 mg 2 or 3 times daily have demonstrated a decrease in serum prolactin and decreased galactorrhea in patients taking dopaminergic neuroleptic drugs such as phenothiazines, haloperidol and loxapine.[1][2] No studies have been reported on the effects of amantadine on the milk supply in nursing mothers. The maternal prolactin level in a mother with established lactation may not affect her ability to breastfeed. Protein Binding Approximately 67% bound to plasma proteins over a concentration range of 0.1 to 2.0 µg/mL. Toxicity Data LD50: 800 mg/kg (Oral, Rat) LD50: 700 mg/kg (Oral, Mouse) Interactions The anti-influenza A activities of amantadine and ribavirin were investigated seperately and in combination. In ferret tracheal ciliated epithelium, the combination of drugs synergistically delayed the virus-induced cytopathic effect. Concurrent use /of alcohol/ with amantadine is not recommended since this may increase the potential for CNS effects such as dizziness, lightheadedness, orthostatic hypotension, or confusion. Concurrent use /of anticholinergics, or other medications with anticholinergic activity; tricyclic antidepressants; other antidyskinetics; antihistamines; or phenothiazines/ with amantadine may potentiate the anticholinergic-like side effects, especially those of confusion, hallucinations, and nightmares; dosage adjustments of these medications or of amantadine may be necessary; also, patients should be advised to report occurrences of gastrointestinal problems promptly since paralytic ileus may occur with concurrent therapy. Concurrent use /of opioid- and anticholinergic-containing antidiarrheals/ with amantadine may potentiate the anticholinergic-like side effects; although significant interaction is unlikely with usual doses of opioid- and anticholinergic-containing antidiarrheals, significant interaction may occur if these medications are abused. For more Interactions (Complete) data for AMANTADINE (10 total), please visit the HSDB record page. |
| 参考文献 | |
| 其他信息 |
Amantadine Hydrochloride can cause developmental toxicity according to state or federal government labeling requirements.
Amantadine Hydrochloride is the hydrochloride salt of amantadine, a synthetic tricyclic amine with antiviral, antiparkinsonian, and antihyperalgesic activities. Amantadine appears to exert its antiviral effect against the influenza A virus by interfering with the function of the transmembrane domain of the viral M2 protein, thereby preventing the release of infectious viral nucleic acids into host cells; furthermore, this agent prevents virus assembly during virus replication. Amantadine exerts its antiparkinsonian effects by stimulating the release of dopamine from striatal dopaminergic nerve terminals and inhibiting its pre-synaptic reuptake. This agent may also exert some anticholinergic effect through inhibition of N-methyl-D-aspartic acid (NMDA) receptor-mediated stimulation of acetylcholine, resulting in antihyperalgesia. An antiviral that is used in the prophylactic or symptomatic treatment of influenza A. It is also used as an antiparkinsonian agent, to treat extrapyramidal reactions, and for postherpetic neuralgia. The mechanisms of its effects in movement disorders are not well understood but probably reflect an increase in synthesis and release of dopamine, with perhaps some inhibition of dopamine uptake. See also: Amantadine (has active moiety). Drug Indication Treatment of Parkinson's disease and parkinsonism. Therapeutic Uses Antiparkinson Agents; Antiviral Agents; Dopamine Agents Amantadine is used in the management of certain aspects of fatigue associated with multiple sclerosis, including lowered energy level, deceased sense of well-being, decreased perceived attention and memory, and diminished problem solving ability. /NOT included in US or Canadian product labeling/ Amantadine is indicated in the treatment of idiopathic parkinsonism (paralysis agitans; shaking palsy), post-encephalitic parkinsonism, drug-induced extrapyramidal reactions, symptomatic parkinsonism following injury to the nervous system caused by carbon monoxide intoxication, and parkinsonism associated with cerebral arteriosclerosis in the elderly. /Included in US product labeling/ Amantadine is indicated as a primary agent in the prophylaxis and treatment of respiratory tract infections caused by influenza A virus strains in high-risk patients (including those with pulmonary or cardiovascular disease, the elderly, and residents of nursing homes and other chronic care facilities who have chronic medical conditions), hospital ward contacts of high-risk patients, immunocompromised patients, those in critical public service positions (eg, police, firefighters, medical personnel), in high-risk patients for whom the influenza vaccine is contraindicated, and patients with severe influenza A viral infections. It is effective against all strains of influenza A virus that have been tested to date, including Russian, Brazilian, Texan, London, and others. It may be given as chemoprophylaxis concurrently with inactivated influenza A virus vaccine until protective antibodies develop. However, it should be emphasized that vaccination of high-risk persons each year is the single most important measure for reducing the impact of influenza. No well-controlled studies have examined whether amantadine prevents complication of influenza A in high-risk persons. Resistant strains of influenza A have been reported in patients receiving rimantadine; these resistant strains were also apparently transmitted household contacts. Rimantadine has a similar chemical structure, spectrum of activity, and mechanism of action to amantadine, and drug-resistant strains of virus have cross-resistance to amantadine and rimantadine. /Included in US product labeling/ For more Therapeutic Uses (Complete) data for AMANTADINE (6 total), please visit the HSDB record page. Drug Warnings Swine influenza (H1N1) viruses contain a unique combination of gene segments that have not been reported previously among swine or human influenza viruses in the US or elsewhere. The H1N1 viruses are resistant to amantadine and rimantadine but not to oseltamivir or zanamivir. Suicide attempts (resulting in death in some patients) have been reported rarely in patients receiving amantadine, many of whom received short courses of the drug for influenza prophylaxis or treatment. The manufacturer states that the incidence and pathophysiology of these suicide attempts are not known. Suicide ideation or attempts have been reported in patients with or without a prior history of psychiatric disorders. Amantadine can exacerbate mental status in patients with a history of psychiatric disorders or substance abuse. Patients with suicidal tendencies may exhibit abnormal mental states including disorientation, confusion, depression, personality changes, agitation, aggressive behavior, hallucinations, paranoia, other psychotic reactions, somnolence, or insomnia. Possible neuroleptic malignant syndrome (NMS) has been reported in patients receiving amantadine and was associated with dosage reduction or withdrawal of the drug. NMS is potentially fatal and requires immediate initiation of intensive symptomatic and supportive care. Patients should be observed closely when the dosage of amantadine is reduced or the drug is discontinued; this precaution is especially important in patients receiving concomitant therapy with an antipsychotic agent. Nausea is one of the most frequent adverse effects of amantadine and has been reported in 5-10% of patients receiving the usual dosage of the drug. Anorexia, constipation, diarrhea, and dry mouth have been reported in 1-5% and vomiting has been reported in up to 1% of patients receiving amantadine. Abdominal discomfort or dysphagia also has been reported. The incidence of adverse GI effects is comparable for amantadine and rimantadine. For more Drug Warnings (Complete) data for AMANTADINE (19 total), please visit the HSDB record page. Pharmacodynamics Amantadine is an antiviral drug which also acts as an antiparkinson agent, for which it is usually combined with L-DOPA when L-DOPA responses decline (probably due to tolerance). It is a derivate of adamantane, like a similar drug rimantadine. The mechanism of action of amantadine in the treatment of Parkinson's disease and drug-induced extrapyramidal reactions is not known. It has been shown to cause an increase in dopamine release in the animal brain, and does not possess anticholinergic activity. At present, three licensed antiviral influenza agents are available in Japan: amantadine, zanamivir, and oseltamivir. These antiviral agents can be used for controlling and preventing influenza, but they are not a substitute for vaccination. Amantadine is an antiviral drug with activity against influenza A viruses, but not influenza B viruses. Persons who have influenza A infection and who are treated with amantadine can shed sensitive viruses early in the course of treatment and later shed drug-resistant viruses, especially after 5-7 days of therapy. Such persons can benefit from therapy even when resistant viruses emerge. In screening for amantadine susceptibility, enzyme-linked immunoassays, plaque reduction assays, and TCID50/0.2 ml titration are employed. The molecular changes associated with resistance have been identified as single-nucleotide changes, leading to corresponding amino acid substitutions in one of four critical sites, amino acids 26, 27, 30, and 31, in the transmembrane region of the M2 protein. The polymerase chain reaction (PCR)-restriction fragment length polymorphism analysis method is quite useful. Resistant viruses have been circulated in outbreak situations at nursing homes where amantadine was used not only for treating influenza virus infection but also for Parkinson's disease. Measures should be taken to reduce contact, as much as possible, between persons taking and those not taking antiviral drugs for treatment or chemoprophylaxis.[1] Objective: To explore how amantadine transitioned from an anti-flu drug to antiparkinsonian agent. Methods: A review of the historical literature on the use of amantadine from 1966 to the present was performed. Results: Amantadine was originally introduced and utilized as an antiviral medication. A single patient noticed relief in her Parkinson disease (PD) symptoms after taking amantadine for a flu infection, and this observation sparked an interest, and several important studies that eventually led to a new drug indication. Conclusion: Amantadine has over the years fallen out of favor as a drug to address influenza infection; however, it has become part of the arsenal utilized for early symptomatic treatment of PD, as well an option for treating dyskinesia.[2] Several animal models using mice (most frequently), rabbits, or monkeys have been used to identify compounds active against orthopoxvirus infections. The treatment of vaccinia virus infections has been well studied in models involving infection of scarified skin or eyes, or resulting from intravenous, intraperitoneal, intracerebral, or intranasal virus inoculation. Cowpox virus has been used in intranasal or aerosol infection studies to evaluate the treatment of lethal respiratory infections. Rabbitpox, monkeypox, and variola viruses have been employed to a lesser extent than the other viruses in chemotherapy experiments. A review of the literature over the past 50 years has identified a number of compounds effective in treating one or more of these infections, which include thiosemicarbazones, nucleoside and nucleotide analogs, interferon, interferon inducers, and other unrelated compounds. Substances that appear to have the greatest potential as anti-orthopoxvirus agents are the acyclic nucleotides, (S)-1-(3-hydroxy-2-phosphonylmethoxypropyl)cytosine (cidofovir, HPMPC) and 1-[((S)-2-hydroxy-2-oxo-1,4,2-dioxaphosphorinan-5-yl)methyl]cytosine (cyclic HPMPC), and the acyclic nucleoside analog, 2-amino-7-[(1,3-dihydroxy-2-propoxy)methyl]purine (S2242). Other classes of compounds that have not been sufficiently studied in lethal infection models and deserve further consideration are thiosemicarbazones related to methisazone, and analogs of adenosine-N(1)-oxide and 1-(benzyloxy)adenosine.[3] Background: Postoperative cognitive dysfunction is a clinical entity that is associated with poor outcome. We determined the effectiveness of amantadine in reducing surgery-induced cognitive impairment and the role of glial cell line-derived neurotrophic factor (GDNF) in this effect. Methods: Four-month old male Fischer 344 rats were subjected to right carotid exposure under intravenous anesthesia. Some rats received intraperitoneal injection of 25 mg/kg/day amantadine for 3 days with the first dose at 15 min before the surgery or intracerebroventricular injection of GDNF or an anti-GDNF antibody at the end of surgery. One week later, rats were started to be tested by Barnes maze and fear conditioning. Hippocampus was harvested at 6 h, 24 h or 10 days after the surgery for biochemical analysis. C8-B4 cells, a microglial cell line, were pretreated with 1 ng/ml GDNF for 30 min before being exposed to 5 ng/ml lipopolysaccharide for 2 h.[5] In conclusion, amantadine inhibits viral replication in the Vero E6 cell system. In this study, a functionally relevant interference with the binding of the viral spike protein to ACE2 on target cells could not be shown, with the limitations discussed above. The question was triggered by the predicted docking with close contact of amantadine to Tyr489 and Phe456 in the receptor-binding domain (RBD) of SARS-CoV-2; SARS-CoV-2 RBD (residues Arg319–Phe541) interacts with the N-terminal peptidase domain of ACE2 (residues Ser19–Asp615), which might have indicated a potential antiviral mode of action of amantadine, but our data do not substantiate the in silico hypothesis. Inhibition of a viroporin as an alternative mode of action needs to be analyzed in future studies. In a recently published preprint, amantadine inhibited the recombinant SARS-CoV-2 viroporin protein E and the putative SARS-CoV-2 viroporin Orf10. The authors observed in the Xenopus laevis oocyte model a 77% inhibition of the protein E ion channel-mediated current at 10 µM amantadine, which appears even more potent than the inhibition of the overall virus replication in the more complex eukaryotic cell culture model at an IC50 of 83–119 µM that we have found; these data indicate that viroporin inhibitors merit a closer look. Finally, so far, amantadine appears to also affect the known SARS-CoV-2 mutations because few or no mutations have been identified in protein E or Orf10 in mutated SARS-CoV-2 lineages collected from patients in India. Lineage B 1.1.7 neither contains mutations in protein E nor in Orf10. Nevertheless, a single amino acid exchange can reduce the efficacy of a small molecule, as happened with the influenza A virus years ago. |
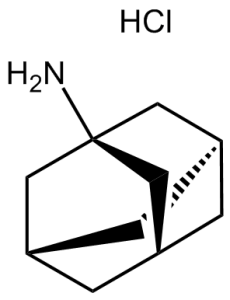
| 分子式 |
C10H18CLN
|
|
|---|---|---|
| 分子量 |
187.7
|
|
| 精确质量 |
187.112
|
|
| 元素分析 |
C, 63.99; H, 9.67; Cl, 18.89; N, 7.46
|
|
| CAS号 |
665-66-7
|
|
| 相关CAS号 |
Amantadine; 768-94-5; Amantadine sulfate; 31377-23-8
|
|
| PubChem CID |
64150
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 密度 |
1.067g/cm3
|
|
| 沸点 |
225.7ºC at 760 mmHg
|
|
| 熔点 |
>300 °C(lit.)
|
|
| 闪点 |
96ºC
|
|
| 折射率 |
1.558
|
|
| LogP |
3.416
|
|
| tPSA |
26.02
|
|
| 氢键供体(HBD)数目 |
2
|
|
| 氢键受体(HBA)数目 |
1
|
|
| 可旋转键数目(RBC) |
0
|
|
| 重原子数目 |
12
|
|
| 分子复杂度/Complexity |
144
|
|
| 定义原子立体中心数目 |
0
|
|
| SMILES |
Cl[H].N([H])([H])C12C([H])([H])C3([H])C([H])([H])C([H])(C([H])([H])C([H])(C3([H])[H])C1([H])[H])C2([H])[H]
|
|
| InChi Key |
WOLHOYHSEKDWQH-UHFFFAOYSA-N
|
|
| InChi Code |
InChI=1S/C10H17N.ClH/c11-10-4-7-1-8(5-10)3-9(2-7)6-10;/h7-9H,1-6,11H2;1H
|
|
| 化学名 |
adamantan-1-amine;hydrochloride
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 6.88 mg/mL (36.65 mM) in PBS (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶。 (<60°C).
请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 5.3277 mL | 26.6383 mL | 53.2765 mL | |
| 5 mM | 1.0655 mL | 5.3277 mL | 10.6553 mL | |
| 10 mM | 0.5328 mL | 2.6638 mL | 5.3277 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
A Safety and Efficacy Study of ADS-5102 in Patients With Multiple Sclerosis and Walking Impairment
CTID: NCT03567057
Phase: Phase 3 Status: Completed
Date: 2022-01-18
|
|
|
|
|
|