| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg | |||
| Other Sizes |
| 靶点 |
PXR; HIV protease (IC50 = 14.6 ng/mL)
Amprenavir is a potent inhibitor of human immunodeficiency virus type 1 (HIV-1) protease, with an IC50 of 0.6 nM for wild-type HIV-1 protease in cell-free enzyme assays and an EC50 of 7 nM for HIV-1 (strain IIIB) replication in H9 lymphocytes [1] - Amprenavir activates the pregnane X receptor (PXR, a nuclear receptor regulating drug metabolism and lipid homeostasis) in vitro, with an EC50 of 15 μM for PXR-mediated luciferase reporter activity in HepG2 cells [3] - It inhibits human hepatocellular carcinoma (HCC) cell migration via downregulating matrix metalloproteinase-9 (MMP-9); no IC50/Ki provided for MMP-9, but 50 μM Amprenavir reduces MMP-9 protein levels by ~70% [2] |
|---|---|
| 体外研究 (In Vitro) |
Amprenavir 促进核受体孕烷 X 受体 (PXR) 与共激活剂 SRC-1 和 PBP 之间的特异性相互作用。 Amprenavir 与 SR12813 形成复合物,对接至人 PXR 的高分辨率晶体结构中。 Amprenavir 占据了所有四个子口袋,其羟基与位于 PXR 连接区域的 Ser247 形成氢键,有助于将药物定位在受体内的最佳方向。安普那韦与 PXR 激活功能 2 (AF-2) 表面的 αAF 上的一个残基 Phe429 形成直接接触,这可能稳定受体的活性 AF-2 构象,并有助于安普那韦对 PXR 的激动剂活性。 Amprenavir 在 HepaRG 细胞和 LS180 细胞中诱导参与 I 期 (CYP3A4)、II 期 (UGT1A1) 和 III 期 (MDR1) 代谢的真正 PXR 靶基因的表达。细胞测定:Amprenavir 在 HepaRG 肝癌细胞和 LS180 肠细胞中诱导 PXR 靶基因表达。
在HIV-1(IIIB株)感染的H9淋巴细胞中,20 nM Amprenavir 处理72小时可使HIV-1 RNA减少约99%(qRT-PCR),HIV-1 p24抗原减少约98%(ELISA);细胞活力保持>95%(MTT法)[1] - 在人肝癌HepG2细胞中,50 μM Amprenavir 处理48小时可抑制细胞迁移约65%(Transwell实验),抑制细胞侵袭约60%(Matrigel侵袭实验);Western blot显示MMP-9减少约70%,间充质标志物α-SMA减少约55% [2] - 在转染PXR的HepG2细胞中,20 μM Amprenavir 处理24小时可上调PXR靶基因表达:CYP3A4 mRNA(3.2倍)、ABCB1 mRNA(2.8倍,RT-PCR)及CYP3A4酶活性(2.5倍,荧光素-IPA实验)[3] - 在原代人肝细胞中,10 μM Amprenavir 处理48小时可诱导甘油三酯蓄积约40%(油红O染色),同时脂生成基因SREBP-1c mRNA上调2.1倍 [3] |
| 体内研究 (In Vivo) |
Amprenavir 会增加 WT 小鼠中致动脉粥样硬化的 LDL 胆固醇分数,但不会增加 PXR−/− 小鼠中的水平。 Amprenavir 刺激 WT 小鼠肠道中已知 PXR 靶基因的表达,包括 CYP3A11、谷胱甘肽转移酶 A1 和 MDR1a,但在 PXR−/− 小鼠中则不然。安普那韦介导的 PXR 激活刺激 WT 小鼠肠道中 LipF 和 LipA 的表达,但在 PXR−/− 小鼠中则不然,表明肠道 PXR 在介导哺乳动物饮食脂质分解和吸收中可能发挥作用。
在雄性Sprague-Dawley大鼠中,口服100 mg/kg Amprenavir(经静脉接种HIV-1的感染模型),给药后24小时血浆HIV-1 RNA降低2.8 log10 [1] - 在荷HepG2异种移植瘤的裸鼠(皮下注射5×10⁶个细胞)中,每日一次口服100 mg/kg Amprenavir,持续21天,肿瘤体积较溶剂对照组减少约50%,肿瘤重量减少约45%;免疫组化显示MMP-9阳性细胞减少约65% [2] - 在C57BL/6小鼠中,每日口服100 mg/kg Amprenavir,持续14天,血浆甘油三酯升高2.3倍,总胆固醇升高1.8倍;该效应在PXR敲除(PXR⁻/⁻)小鼠中消失,证实依赖PXR [3] - 在健康人志愿者中,每日两次口服1200 mg Amprenavir,达稳态血浆浓度12 μM(为HIV-1体外EC50的80倍)[1] |
| 酶活实验 |
HIV-1蛋白酶活性检测流程(基于[1]摘要描述):从大肠杆菌中纯化野生型HIV-1蛋白酶。将该酶与荧光肽底物(Ac-Thr-Ile-Nle-Phe-Gln-Arg-Lys-AMC)混合于检测缓冲液(50 mM醋酸钠pH 4.7,1 mM EDTA,10%甘油)中。加入0.1~10 nM的Amprenavir,在37°C孵育2小时。检测激发波长355 nm/发射波长460 nm处的荧光强度。相对于溶剂对照组计算抑制率,采用四参数逻辑回归确定IC50[1]
- PXR荧光素酶报告实验流程(基于[3]摘要描述):HepG2细胞共转染人PXR表达质粒和PXR响应性荧光素酶报告质粒(pGL3-PXRE)。转染24小时后,用1~50 μM Amprenavir 处理细胞24小时。裂解细胞后检测荧光素酶活性(归一化至β-半乳糖苷酶内参),通过剂量-反应拟合计算PXR激活的EC50[3] |
| 细胞实验 |
Amprenavir 诱导 LS180 肠细胞和 HepaRG 肝癌细胞中 PXR 靶基因的表达。
HIV-1感染H9细胞实验流程(基于[1]摘要描述):H9淋巴细胞在含10%胎牛血清的RPMI 1640培养基中培养,用HIV-1(IIIB株)以MOI=0.01感染24小时后,用5~50 nM Amprenavir 处理72小时。收集培养上清液,qRT-PCR检测HIV-1 RNA,ELISA检测p24抗原;MTT法(570 nm吸光度)评估细胞活力[1] - HepG2细胞迁移/侵袭实验流程(基于[2]摘要描述):HepG2细胞在含10%胎牛血清的DMEM培养基中培养至70%汇合。迁移实验:将2×10⁴个细胞接种于Transwell上室(含10~100 μM Amprenavir 的无血清DMEM),下室加10% FBS;24小时后结晶紫染色计数迁移细胞。侵袭实验:使用Matrigel包被的Transwell,孵育时间延长至48小时[2] - 原代肝细胞脂质蓄积实验流程(基于[3]摘要描述):从C57BL/6小鼠中分离原代肝细胞,在William’s E培养基中培养。用1~20 μM Amprenavir 处理细胞48小时。油红O染色检测脂质蓄积(510 nm吸光度定量);提取总RNA,RT-PCR检测SREBP-1c mRNA水平[3] |
| 动物实验 |
10 mg/kg; p.o.
WT and PXR-/- mice Rat HIV-1 infection model (from [1] abstract description): Male Sprague-Dawley rats (250–300 g) were intravenously inoculated with HIV-1 (IIIB, 1×10⁵ TCID50/rat). 2 hours post-inoculation, Amprenavir was dissolved in 10% ethanol + 40% propylene glycol + 50% water (oral formulation) and administered via oral gavage at 100 mg/kg. Plasma samples were collected at 0, 6, 12, 24 hours post-dose for HIV-1 RNA quantification (qRT-PCR) [1] - Nude mouse HepG2 xenograft model (from [2] abstract description): Female BALB/c nude mice (6–8 weeks old) were subcutaneously injected with 5×10⁶ HepG2 cells (suspended in 0.1 mL PBS + 50% Matrigel) into the right flank. When tumors reached ~100 mm³, Amprenavir (dissolved in corn oil) was administered via oral gavage at 100 mg/kg once daily for 21 days. Vehicle controls received corn oil. Tumor volume (V=0.5×length×width²) was measured every 3 days; mice were euthanized on day 22 for tumor weight and immunohistochemistry [2] - Mouse PXR-mediated dyslipidemia model (from [3] abstract description): Male C57BL/6 wild-type (WT) and PXR⁻/⁻ mice (8–10 weeks old) were administered Amprenavir (dissolved in 0.5% methylcellulose) via oral gavage at 100 mg/kg/day for 14 days. Vehicle controls received 0.5% methylcellulose. Plasma triglycerides and total cholesterol were measured via enzymatic assays on day 15; liver tissues were collected for RT-PCR (lipogenic genes) [3] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Rapidly absorbed after oral administration in HIV-1-infected patients with a time to peak concentration (Tmax) typically between 1 and 2 hours after a single oral dose. The absolute oral bioavailability of amprenavir in humans has not been established. Amprenavir is absorbed rapidly after oral administration. Taking amprenavir with a standard meal reduces the plasma AUC by only about 13%, but high-fat meals may have greater effects and should be avoided. Only minimal amounts of amprenavir are eliminated unchanged in urine or feces; less than 3% of a dose is eliminated unchanged in urine. Following a single oral dose of radiolabeled amprenavir, approximately 14% of the dose is eliminated in urine and 75% is eliminated in feces; 2 metabolites account for more than 90% of radioactivity in feces. Distribution of amprenavir into body tissues and fluids has not been fully characterized. Studies in rats indicate that amprenavir is distributed to a variety of tissues following oral administration. The apparent volume of distribution of amprenavir in healthy adults is approximately 430 L. It is not known whether amprenavir crosses the human placenta; however, the drug crosses the placenta in rats. Information from an ex vivo human placental model for transplacental passage indicates that amprenavir crosses the human placenta. Although it is not known whether amprenavir is distributed in human milk, the drug is distributed into milk in rats. In patients with hepatic impairment, the peak plasma concentration and AUC of amprenavir may be increased. In adults with moderate cirrhosis who received a single 600-mg oral dose of amprenavir given as liquid-filled capsules, the AUC (0-4 hours) of the drug averaged 25.76 ug hour/mL compared with 12 ug hour/ml in healthy adults. In adults with severe cirrhosis who received the same dose, peak plasma concentrations averaged 9.43 ug/ml and the AUC (0-4 hours) averaged 38.66 ug hour/ml compared with 4.9 ug/ml or 12 ug hour/ml, respectively, in healthy adults. Metabolism / Metabolites Hepatic. Amprenavir is metabolized in the liver by the cytochrome P450 3A4 (CYP3A4) enzyme system. The 2 major metabolites result from oxidation of the tetrahydrofuran and aniline moieties. Glucuronide conjugates of oxidized metabolites have been identified as minor metabolites in urine and feces. The metabolic fate of amprenavir has not been fully determined, but the drug is metabolized in the liver. Amprenavir is metabolized principally by the cytochrome P450 (CYP) isoenzyme 3A4. The 2 major metabolites of the drug result from oxidation of the tetrahydrofuran and aniline moieties; glucuronide conjugates of oxidized metabolites have been identified as minor metabolites in urine and feces. Hepatic. Amprenavir is metabolized in the liver by the cytochrome P450 3A4 (CYP3A4) enzyme system. The 2 major metabolites result from oxidation of the tetrahydrofuran and aniline moieties. Glucuronide conjugates of oxidized metabolites have been identified as minor metabolites in urine and feces. Half Life: 7.1-10.6 hours Biological Half-Life 7.1-10.6 hours The plasma elimination half-life of amprenavir in HIV-infected adults with normal renal and hepatic function ranges from 7.1-10.6 hours. In healthy human volunteers, oral Amprenavir (1200 mg twice daily) had an oral bioavailability of ~40%, a plasma elimination half-life (t₁/₂) of ~7.1 hours, and a peak plasma concentration (Cmax) of 12 μM (reached at 1.5 hours post-dose) [1] - In male Sprague-Dawley rats, oral Amprenavir (100 mg/kg) showed a t₁/₂ of ~4.5 hours, a Cmax of 8 μM, and a volume of distribution (Vd) of ~1.8 L/kg [1] - Amprenavir is primarily metabolized by hepatic cytochrome P450 3A4 (CYP3A4); ~70% of the dose is excreted as metabolites in feces, with <5% excreted unchanged in urine [1] - Plasma protein binding of Amprenavir is ~90% in humans, rats, and mice (measured via ultrafiltration) [1,3] |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
Amprenavir inhibits the HIV viral proteinase enzyme which prevents cleavage of the gag-pol polyprotein, resulting in noninfectious, immature viral particles. Protein Binding Very high (90%). Amprenavir has the highest affinity for alpha(1)-acid glycoprotein. Interactions Because amprenavir oral solution contains a large amount of propylene glycol, concurrent use /with alcohol, disulfiram, or metronidazole/ is not recommended. Although these medications /alprazolam, clorazepate, diazepam, or flurazepam/ have not been specifically studied with amprenavir, amprenavir may increase the serum concentrations of these medications. Although these medications /amiodarone, lidocaine (systemic), tricyclic antidepressants, or quinidine/ have not been specifically studied with amprenavir, amprenavir may interfere in the metabolism of these medications and cause serious or life threatening adverse events; monitoring of serum concentrations for these medications is recommended if amprenavir is used concurrently. Although antacids have not been specifically studied with amprenavir, based on data from other protease inhibitors, antacids (and didanosine due to the antacid content present in didanosine formulations) may interfere with the absorption of amprenavir; it is recommended that antacid and didanosine administration be separated from amprenavir administration by at least one hour. For more Interactions (Complete) data for AMPRENAVIR (21 total), please visit the HSDB record page. In HIV-1-infected H9 cells, Amprenavir up to 10 μM for 72 hours had no significant cytotoxicity (cell viability >90% vs. vehicle) [1] - In C57BL/6 mice, oral Amprenavir (100 mg/kg/day for 14 days) caused mild hepatomegaly (liver weight increased by ~15%) but no elevation in serum ALT/AST; PXR⁻/⁻ mice showed no hepatomegaly [3] - In healthy human volunteers (Phase I/II studies), common adverse events (AEs) included mild gastrointestinal symptoms (nausea: 22%, diarrhea: 18%) and rash (15%)[1] - In HepG2 cells, 100 μM Amprenavir for 72 hours induced apoptosis in ~20% of cells (Annexin V-FITC/PI staining), indicating low cytotoxicity at therapeutic concentrations [2] |
| 参考文献 |
|
| 其他信息 |
Therapeutic Uses
Amprenavir is indicated in combination with other antiretroviral agents in the treatment of HIV-1 infection. /Included in US product labeling/ Amprenavir is a human immunodeficiency virus (HIV)-protease inhibitor. The use of amprenavir for the treatment of human immunodeficiency virus type 1 (HIV-1) infection in combination with other antiretrovirals is based on analyses of plasma HIV-RNA levels and CD4 cell counts in controlled studies of up to 24 weeks duration. Results from controlled trials evaluating the long-term suppression of HIV-RNA or disease progression with amprenavir have not yet been obtained. Amprenavir is a viral protease inhibitor with specificity for the HIV protease enzyme. The resistance profile of amprenavir appears to differ from that of other protease inhibitors such as saquinavir and indinavir. Twelve hours after single-dose administration of amprenavir 1200 mg to HIV-infected individuals, the mean plasma concentration of the drug was more than 10-fold greater than the 50% inhibitory concentration for HIV-1IIIB in peripheral blood lymphocytes. In a small nonblind study, amprenavir monotherapy increased CD4+ cell count and decreased viral load in 37 patients with HIV infection and no previous exposure to protease inhibitor therapy. Combination therapy comprising amprenavir and other antiretroviral agents (abacavir, zidovudine, lamivudine, indinavir, saquinavir or nelfinavir) decreased viral load and increased CD4+ cell counts in patients with HIV infection. Antiviral efficacy was maintained during up to 24 weeks' follow-up. Drug Warnings The usually recommended dosage of amprenavir oral solution (22.5 mg/kg twice daily) provides a propylene glycol intake of 1650 mg/kg daily; however, an acceptable intake of propylene glycol used as an excipient in pharmaceuticals has not been established to date. Propylene glycol is metabolized in the liver by the alcohol and aldehyde dehydrogenase enzyme pathway, and the possibility exists that young infants, patients with renal or hepatic impairment, and certain patient groups (females, Asians, Native Alaskans, Native Americans) may be at increased risk of propylene glycol-associated adverse effects if they receive amprenavir oral solution because of diminished ability to metabolize propylene glycol. Therefore, amprenavir oral solution is contraindicated during pregnancy; in infants younger than 4 years of age; in patients with renal or hepatic failure; and in patients receiving disulfiram or metronidazole. In addition, although metabolism of propylene glycol has not been specifically studied in these patient groups, the possibility that females may have lower concentrations of alcohol dehydrogenase compared with males and that certain ethnic populations (Asians, Native Alaskans, Native Americans) may have alcohol dehydrogenase polymorphism should be considered. Because amprenavir oral solution contains large amounts of propylene glycol and because young infants may be at increased risk of propylene glycol-associated adverse effects, the oral solution is contraindicated in pediatric patients younger than 4 years of age. Propylene glycol is metabolized in the liver by the alcohol and aldehyde dehydrogenase enzyme pathway. Although alcohol dehydrogenase is present in human fetal liver at 2 months of gestational age, this represent only about 3% of the activity reported in adults. Limited data indicate that alcohol dehydrogenase activity in infants 12-30 months of age is equal to or greater than that reported in adults. Oral or IV administration of various drugs (e.g., multivitamins) containing high concentrations of propylene glycol in pediatric patients has resulted in various propylene glycol-associated adverse effects, including hyperosmolality, lactic acidosis, respiratory depression, and seizures. Patients being treated with amprenavir oral solution should be closely monitored for propylene glycol associated side effects including hemolysis, hyperosmolality, lactic acidosis, renal toxicity, seizures, stupor, and tachycardia. The pharmacokinetics of amprenavir do not differ between females and males or between Blacks and non-Blacks. However, amprenavir oral solution contains a large amount of propylene glycol and because Asians, Eskimos, Native Americans, and women have a decreased ability to metabolize this compound, they may have an increased risk of developing propylene glycol-associated side effects. For more Drug Warnings (Complete) data for AMPRENAVIR (18 total), please visit the HSDB record page. Pharmacodynamics Amprenavir is a protease inhibitor with activity against Human Immunodeficiency Virus Type 1 (HIV-1). Protease inhibitors block the part of HIV called protease. HIV-1 protease is an enzyme required for the proteolytic cleavage of the viral polyprotein precursors into the individual functional proteins found in infectious HIV-1. Amprenavir binds to the protease active site and inhibits the activity of the enzyme. This inhibition prevents cleavage of the viral polyproteins resulting in the formation of immature non-infectious viral particles. Protease inhibitors are almost always used in combination with at least two other anti-HIV drugs. Amprenavir is a first-generation HIV-1 protease inhibitor approved by the FDA in 2001 for the treatment of HIV-1 infection in adults and adolescents; it is administered orally (capsules or oral solution) [1] - Its anti-HIV mechanism involves binding to the HIV-1 protease active site, blocking cleavage of the viral Gag-Pol polyprotein into mature proteins (e.g., p24, reverse transcriptase), thus inhibiting viral assembly [1] - Amprenavir exhibits off-target effects: activation of PXR leads to dyslipidemia (hypertriglyceridemia, hypercholesterolemia) in vivo, and inhibition of HCC cell migration suggests potential repurposing for liver cancer therapy [2,3] - Due to CYP3A4 metabolism, Amprenavir has drug-drug interactions with CYP3A4 inhibitors (e.g., ritonavir, increasing its plasma concentration) and inducers (e.g., rifampin, decreasing its concentration) [1] |
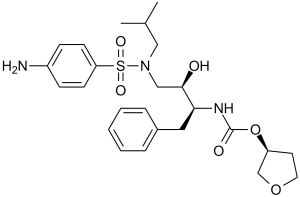
| 分子式 |
C25H35N3O6S
|
|
|---|---|---|
| 分子量 |
505.63
|
|
| 精确质量 |
505.224
|
|
| 元素分析 |
C, 59.39; H, 6.98; N, 8.31; O, 18.99; S, 6.34
|
|
| CAS号 |
161814-49-9
|
|
| 相关CAS号 |
Amprenavir-d4;1217661-20-5;Amprenavir-d4-1;2738376-78-6
|
|
| PubChem CID |
65016
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 密度 |
1.3±0.1 g/cm3
|
|
| 沸点 |
722.5±70.0 °C at 760 mmHg
|
|
| 熔点 |
72-74ºC
|
|
| 闪点 |
390.8±35.7 °C
|
|
| 蒸汽压 |
0.0±2.5 mmHg at 25°C
|
|
| 折射率 |
1.602
|
|
| LogP |
4.68
|
|
| tPSA |
139.57
|
|
| 氢键供体(HBD)数目 |
3
|
|
| 氢键受体(HBA)数目 |
8
|
|
| 可旋转键数目(RBC) |
12
|
|
| 重原子数目 |
35
|
|
| 分子复杂度/Complexity |
745
|
|
| 定义原子立体中心数目 |
3
|
|
| SMILES |
S(C1C([H])=C([H])C(=C([H])C=1[H])N([H])[H])(N(C([H])([H])C([H])(C([H])([H])[H])C([H])([H])[H])C([H])([H])[C@]([H])([C@]([H])(C([H])([H])C1C([H])=C([H])C([H])=C([H])C=1[H])N([H])C(=O)O[C@]1([H])C([H])([H])OC([H])([H])C1([H])[H])O[H])(=O)=O
|
|
| InChi Key |
YMARZQAQMVYCKC-OEMFJLHTSA-N
|
|
| InChi Code |
InChI=1S/C25H35N3O6S/c1-18(2)15-28(35(31,32)22-10-8-20(26)9-11-22)16-24(29)23(14-19-6-4-3-5-7-19)27-25(30)34-21-12-13-33-17-21/h3-11,18,21,23-24,29H,12-17,26H2,1-2H3,(H,27,30)/t21-,23-,24+/m0/s1
|
|
| 化学名 |
[(3S)-oxolan-3-yl] N-[(2S,3R)-4-[(4-aminophenyl)sulfonyl-(2-methylpropyl)amino]-3-hydroxy-1-phenylbutan-2-yl]carbamate
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (4.94 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (4.94 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (4.94 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.9777 mL | 9.8887 mL | 19.7773 mL | |
| 5 mM | 0.3955 mL | 1.9777 mL | 3.9555 mL | |
| 10 mM | 0.1978 mL | 0.9889 mL | 1.9777 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT00002417 | Completed | Drug: Amprenavir | HIV Infections | Glaxo Wellcome | Not Applicable | |
| NCT00002205 | Completed | Drug: Abacavir sulfate Drug: Amprenavir |
HIV Infections | Glaxo Wellcome | Not Applicable | |
| NCT00038519 | Completed | Drug: Amprenavir/ritonavir Drug: Saquinavir/ritonavir |
HIV Infections | Abbott | April 2001 | Phase 2 Phase 3 |
| NCT00002245 | Completed | Drug: Amprenavir Drug: Lamivudine |
HIV Infections | Glaxo Wellcome | April 1999 | Phase 3 |
| NCT00001758 | Completed | Drug: Abacavir Drug: Amprenavir |
HIV Infection | National Institute of Allergy and Infectious Diseases (NIAID) |
August 2003 | Phase 2 |