| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| Other Sizes |
| 靶点 |
mGluR2 ( EC50 = 285 nM )
|
|---|---|
| 体外研究 (In Vitro) |
AZD-8529 mesylate 增强谷氨酸对 mGluR2 的作用,EC50 为 195 nM [1]。 AZD-8529 甲磺酸盐在 25 μM 时不会引起 mGluR 拮抗剂反应[1]。
AZD8529增强mGluR2受体功能[1] 我们通过测量在外源性激动剂(L-谷氨酸)浓度增加的情况下[35S]GTPγS结合的增强,评估了AZD8529对人类mGluR2受体的影响。AZD8529增强了谷氨酸对mGluR2的影响,EC50为195±62 nM,Emax为110%±11%(图1A)。为了评估AZD8529对mGluRs家族的选择性,我们使用了基于荧光的检测方法。AZD8529增强mGluR2活性,EC50为285±20 nM,在20-25 M下对mGluR1、3、4、5、6、7和8亚型没有产生任何正变构调节剂反应(表1)。此外,在25μM时,AZD8529对mGluRs没有引起拮抗剂反应。当在广泛的受体筛选中研究AZD8529(10μM)时(表2),我们观察到配体结合腺苷A3受体(51%抑制)和去甲肾上腺素转运蛋白(NET,IC50=4.73μM)的抑制率>50%。 体外电生理试验[2] mGlu2/3受体激动剂DCG-IV对海马CA1区锥体细胞中的fEPSPs具有抑制作用。AZD8418和AZD8529增强了DCG-IV对突触传递的抑制作用,EC50值分别为0.86和1.4μM(图2a)。AZD8418产生的最大增强作用(79.9±4.4)大于AZD8529(61.4±4.3,mGlu2/3受体拮抗剂LY341495(1μM)有效阻断了DCG-IV单独(10 nM)或DCG-IV与AZD8529(10μM)或AZD8418(10μM)联合诱导的fEPSPs的抑制作用;图2b)。 |
| 体内研究 (In Vivo) |
AZD8529(0.3 mg/kg,肌肉注射)可减少松鼠猴中尼古丁启动诱导和提示诱导的恢复[1]。 AZD-8529(30 mg/kg;腹腔注射)可降低自由活动大鼠伏隔核中尼古丁诱导的细胞外多巴胺增加[1]。动物模型:Sprague-Dawley大鼠[1] 剂量:10 mg/kg、30 mg/kg 给药方式:腹腔注射;尼古丁注射前 2 小时 结果:减少了自由活动大鼠伏隔核中由尼古丁(0.4 mg/kg,皮下)引起的细胞外多巴胺增加 [1]。
在猴子中,AZD8529在不影响食物自我给药的剂量(.3-3mg/kg)下减少了尼古丁的自我给药。AZD8529还减少了尼古丁引发和线索诱导的尼古丁恢复,在药物消失后寻求增强反应。在大鼠中,AZD8529减少了尼古丁诱导的伏隔核多巴胺释放。 结论:这些结果为mGluR2的正变构调节剂在尼古丁强化和复发的非人灵长类模型中的有效性提供了证据。这类药物应考虑用于尼古丁成瘾治疗。 AZD8418(0.37、1.12、3.73、7.46和14.92 mg/kg)和AZD8529(1.75、5.83、17.5和58.3 mg/kg)的急性治疗抑制了尼古丁的自我给药,对食物维持反应没有影响。AZD8418的慢性治疗减弱了尼古丁的自我给药,但对这种作用的耐受性迅速发展。慢性AZD8529给药对尼古丁自我给药的抑制作用在整个14天的治疗过程中持续存在。任何一种PAM的慢性治疗都会抑制食物的自我给药。AZD8418(急性)和AZD8529(急性和亚慢性)阻断了线索诱导的尼古丁和食物寻求行为的恢复。结论:这些发现表明,mGlu2受体在自我给药尼古丁的增强特性以及之前与尼古丁给药相关的线索的动机影响(即线索诱导的尼古丁寻求行为的恢复)中起着重要作用。因此,mGlu2-PAM可能是帮助人们戒烟和防止复发的有用药物[2]。 |
| 酶活实验 |
功能性mGluR2测定[1]
受体选择性测定[1] 为了确定mGluR家族中AZD8529的选择性,我们使用了基于荧光的检测和表达人mGluR构建体的HEK 293细胞系。所述细胞系表达嵌合融合构建体hmGluR2/hCaR*、hmGluR1/hCaR+、hmGluR3/hCaR+hmGluR4/hCaR*hmGluR5/hCaR>hmGluR6/hCaR=hmGluR7/hCaR*hmGluR8/hCaR*,各自包含人mGluR的细胞外结构域和跨膜结构域,以及如前所述与混杂嵌合蛋白Gqi5融合的人钙受体的细胞内结构域。 受体筛查[1] 我们根据已发表的方法,使用放射性配体结合分析(MDS Pharma)评估了10μM下AZD8529的脱靶效应。我们为每种测定都运行了参考标准。我们使用数据分析工具箱(MDL信息系统)的非线性最小二乘回归分析来确定IC50值。 [35S]GTPγS结合人mGlu2-CHO膜[1] 我们使用由表达人mGluR2的CHO细胞系制备的膜,并以闪烁邻近试验(SPA)形式进行了试验。我们将表达人mGluR2的中国仓鼠卵巢(CHO)细胞培养至约80%融合,在冰冷的磷酸盐缓冲盐水中洗涤细胞,并冷冻保存直至膜制备。测定缓冲液含有0.05 M HEPES、0.10 M NaCl、0.01 M MgCl2,pH 7.4,加上100 M二硫苏糖醇和3 M鸟苷二磷酸。我们通过在含有AZD8529或载体的测定缓冲液中加入小麦胚芽凝集素SPA珠(0.75mg/ml)和膜(6g/ml)的混合物来开始测定。孵育15分钟后,我们加入了一种含有[35S]GTPγS和L-谷氨酸盐的溶液(最终浓度为100 pM[35S]GTPγS和0-100 M谷氨酸盐)。在室温下孵育(60分钟)后,我们对测定板进行离心,并在TopCount™闪烁计数器上读取。我们分别测定了在没有谷氨酸和存在100-M谷氨酸的情况下[35S]GTPγS结合的0%和100%水平。我们根据AZD8529的浓度反应曲线估计了AZD8529s对mGluR2激活的调节活性,并用4参数逻辑斯谛方程进行了拟合,以计算表观效力(EC50)和最大效力(Emax)。 |
| 细胞实验 |
[35S]食蟹猴脑片GTPγS放射自显影术[1]
我们用戊巴比妥钠(100mg/kg)麻醉猴子,用生理盐水灌注,然后取出大脑并将其冷冻在冷却的异戊烷中。我们在低温恒温器上切下20-μm的纹状体和海马切片,将切片安装在载玻片上,并在80°C下储存直至使用。在实验当天,我们在真空室中将切片加热到室温超过3小时。我们在50 mM Tris-HCl、3 mM MgCl2、0.2 mM EGTA、100 mM NaCl和0.2 mM DTT(Tris测定缓冲液,TAB)中孵育切片;pH 7.4,在25°C下孵育10分钟。然后,我们将载玻片在含有2 mM二磷酸鸟苷(GDP)的TAB中,在25℃下孵育15分钟。我们将载玻片置于以下四种条件之一中,在25°C下放置2小时:基础:TAB+2 mM GDP+0.04 nM[35S]GTPγS;单独使用激动剂:TAB+2 mM GDP+0.04 nM[35S]GTPγS+1μM LY379268;单独使用调节剂:TAB+2 mM GDP+0.04 nM[35S]GTPγS+3μMAZD8529;调节剂+激动剂:TAB+2 mM GDP+0.04 nM[35S]GTPγS+1μM LY379268+3μM AZD8529;调节剂+激动剂+拮抗剂:TAB+2 mM GDP+0.04 nM[35S]GTPγS+1μM LY379268+3μM AZD8529+1μM LY341495。然后,我们在4°C 50 mM Tris-HCl(pH 7.4)中洗涤切片2次,每次5分钟,在冰冷的H2O中漂洗,并风干载玻片。然后,我们将载玻片暴露在Biomax MR胶片上2天,并使用标准技术进行显影、数字化和分析。 切片记录[2] 将切片浸入切片室中,以1-2ml/min的流速浸泡在32°C aCSF中。用铂丝制成的砝码将切片固定到位。用连接到隔离脉冲刺激器(型号2100)的单极钨电极(型号575300,0.5-1mΩ)刺激辐射层中的Schaeffer侧支纤维。用从硼硅酸盐玻璃(型号TW150-4)中拔出并填充2mM NaCl的电极记录CA1层锥体细胞的细胞外群体尖峰。用每30秒一次的10毫秒脉冲刺激切片。建立基线反应(最大值的50-70%),然后记录大约15分钟的控制期。在控制期后,将化合物浴敷40分钟或直至达到稳态响应。 |
| 动物实验 |
Sprague-Dawley rats
10 mg/kg, 30 mg/kg Intraperitoneal injection; 2 hours before nicotine injections Nicotine self-administration [1] We performed this phase over a period of 14 weeks and it included 1-hr sessions from Monday through Friday. Before the start of each session, we placed the monkeys into the Plexiglas chairs and restrained them in the seated position by waist locks. We first trained the monkeys to lever-press under a fixed-ratio schedule (FR10, timeout 60 s) of intravenous nicotine (30 μg/kg/injection) reinforcement. After flushing the catheters with 1 ml physiological saline, we connected them to a motor-driven syringe. At the start of each session, the white house-light was turned off and the green stimulus light was turned on; 10 lever-presses turned off the green light and produced 2-s amber light paired with nicotine injection (0.2 ml). During the 60-s timeout period the chamber was dark and lever-presses had no programmed consequences. When responses showed <15% variability for at least 5 consecutive sessions, we tested the effect of AZD8529 pretreatment (0.03, 0.3, 1, 3, and 10 mg/kg, i.m., 3 hr before the session) on nicotine self-administration for 3 sessions; we compared these data to three consecutive session of vehicle pretreatment immediately preceding each test session. The 3-hr pretreatment time is based on AstraZeneca Tmax pharmacokinetic studies (data not shown). Reinstatement of nicotine seeking [1] We performed this phase of the study over a period of 9 weeks. We first tested the monkeys for nicotine priming-induced reinstatement after extinction of the drug-reinforced responding. We then retrained them to self-administer nicotine over 5 days and then tested them for cue-induced reinstatement after extinction of the drug-reinforced responding. We tested AZD8529 doses of 3 mg/kg or lower, because 3 mg/kg was the highest effective dose that reduced nicotine but not food self-administration. Nicotine priming-induced reinstatement [1] We performed tests for nicotine priming-induced reinstatement after the monkeys underwent daily extinction sessions during which lever-presses led to saline infusions plus the visual cues previously paired with nicotine infusions, but not nicotine. We gave a non-contingent saline injection before each extinction session as a vehicle control for the nicotine-priming injections. After at least two extinction sessions, when responding had reached a low, stable level, we determined the effect of pretreatment with AZD8529 (0.3, 1 or 3 mg/kg, i.m.) or its vehicle on nicotine (0.1 mg/kg i.v.)-induced reinstatement. We gave the nicotine priming injections immediately before the start of the test sessions. During testing, lever-presses (FR10) continued to produce only saline injections and the discrete cues. We also tested the effect of 3 mg/kg of AZD8529 on saline priming to determine whether AZD8529 alone would affect nicotine seeking after extinction. Cue-induced reinstatement [1] After the completion of nicotine priming tests, we retrained the monkeys to self-administer nicotine for ~10 sessions. We then gave them 3 extinction sessions during which lever-presses had no reinforced consequences (neither nicotine nor cue were available); additionally, we did not inject monkeys with saline priming before these sessions. After extinction, we determined the effect of pretreatment with AZD8529 (0.3, 1 or 3 mg/kg, i.m.) or its vehicle on cue-induced reinstatement. During testing, lever-presses (FR10) produced the i.v. saline infusions and visual cue presentations. We also determined the effect of 3 mg/kg of AZD8529 on extinction responding in the absence of the cue. Each cue-induced reinstatement test was followed by one or two extinction sessions. Food self-administration [1] We determined the effect of AZD8529 in a separate group of monkeys that self-administered 190-mg food pellets under reinforcement schedule conditions identical to those we used with nicotine (FR 10, TO 60 s). We restricted food intake to maintain monkeys’ weights at a level that facilitates food-reinforced responding (no more than 10% below free-feeding weight). The number of reinforcers delivered per session, as well as rates of responding, in this group were very similar to the nicotine group (Figure 2). We injected each dose of AZD8529 (3, 10 and 30 mg/kg, i.m.) for three consecutive sessions, which was preceded by three sessions with vehicle injections before the sessions. AZD8529 plasma levels in squirrel monkeys [1] To determine whether plasma levels during the behavioral experiments reach levels that are well tolerated in humans (per AstraZeneca company information), we injected 3 squirrel monkeys with AZD8529 (1 mg/kg, i.m.) and 3 hr later we collected venous blood samples (approximately 1.5 ml) from the femoral vein under light ketamine (10 mg/kg, i.m.) anesthesia. We rapidly mixed the blood samples and immediately cooled them on ice until centrifugation. Plasma was prepared by centrifugation at 4°C for 10 min at 1500 x g within 30 min of blood sampling. We separated the plasma and transferred it to two 2-ml micro-centrifuge tubes. We stored the plasma samples at −80°C. We shipped the samples on dry ice to AstraZeneca where AZD8529 levels were measured using a standardized LC/MS/MS method. In vivo microdialysis in rats [1] The general procedure was described previously (36). We performed microdialysis in Sprague-Dawley rats 20-24 hr after implantation of probes aimed at the accumbens shell (2.0 mm anterior,1.1 mm lateral from bregma, and 8.0 mm below the dura) (37). We collected samples (20 μl) every 20 min (perfusion rate: 1ul per min) and immediately analyzed dopamine levels by HPLC coupled to electrochemical detection. We injected the test drugs or their vehicle after observing stable dopamine levels (<15% variation) in 3 consecutive samples. We injected vehicle or AZD8529 (10 or 30 mg/kg i.p.) 2 hr before vehicle or nicotine (0.4 mg/kg s.c.) injections. We collected dialysate samples for 2 hr after nicotine injections. We based the AZD8529 doses on previous unpublished work of AstraZeneca in rat behavioral models and a recent study on the effect of the drug on ‘incubation’ of methamphetamine craving in rats. [1] AZD8529 free-base was dissolved in sterile water.[1] Experimental design [2] Experiment 1: effects of acute AZD8418 and AZD8529 treatment on nicotine and food self-administration [2] After establishing stable nicotine or food self-administration (<20 % variability in responding over three consecutive days), the effects of acute AZD8418 (0, 0.37, 1.12, 3.73, 7.46, and 14.92 mg/kg) and AZD8529 (0, 1.75, 5.83, 17.5, and 58.3 mg/kg) treatment on nicotine and food self-administration were assessed using a within-subjects Latin square design. Four groups of naive rats were used to examine the effects of acute treatment with (i) AZD8418 on nicotine self-administration (n = 12) and food self-administration (n = 10) and (ii) AZD8529 on nicotine self-administration (n = 12) and food self-administration (n = 7). At least 5 days elapsed between drug administrations. Experiment 2: effects of chronic AZD8418 and AZD8529 treatment on nicotine and food self-administration [2] The effects of 14-day repeated AZD8418 and AZD8529 treatment regimens on nicotine and food self-administration were assessed using a between-subjects design. Four groups of naive rats were used to examine the effects of chronic treatment with (i) AZD8418 (0, 3.73, 7.46, and 14.92 mg/kg/day) on nicotine self-administration (n = 10–11/subgroup), (ii) AZD8418 (0 and 14.92 mg/kg/day) on food-self-administration (n = 10–11/subgroup), (iii) AZD8529 (0 and 58.3 mg/kg/day) on nicotine self-administration (n = 10–12/subgroup), and (iv) AZD8529 (0 and 58.3 mg/kg/day) on food self-administration (n = 8–13/subgroup). The subgroups for each tested compound were balanced for weight and nicotine/food intake before initiating the chronic treatments. Experiment 3: effects of acute AZD8418 and AZD8529 treatment on cue-induced reinstatement of nicotine- and food-seeking behavior [2] After completing experiment 1, nicotine self-administering rats were tested under extinction conditions. All of the rats reached the predetermined criterion of extinction (see above) by the end of the 10th extinction session. The first reinstatement session was conducted after vehicle administration to ensure that each subject exhibited robust reinstatement as defined above (>50 % increase in responding compared to the mean of the last three extinction sessions) before initiating the drug treatments. Only rats that exhibited robust nicotine-seeking behavior during this first reinstatement session were included in the remainder of the experiments. Each reinstatement session was preceded by three daily extinction sessions to re-extinguish responding. AZD8418 (0, 1.12, 3.73, 7.46, and 14.92 mg/kg) and AZD8529 (0, 1.75, 5.83, 17.5, and 58.3 mg/kg) were administered prior to each reinstatement session using a within-subjects Latin square design. Independent naive rats (n = 9–13/group) that were trained to self-administer food were used to assess the effects of AZD8418 (0, 3.73, 7.46, and 14.92 mg/kg) and AZD8529 (0, 1.75, 5.83, 17.5, and 58.3 mg/kg) on cue-induced reinstatement of food-seeking behavior using a between-subjects design because food-seeking behavior exhibits rapid extinction with repeated reinstatement testing (Bespalov et al. 2005). The groups were balanced for weight and food responding before treatment. Pharmacokinetic studies [2] AZD8529 (4.7 mg/kg) and AZD8418 (5 mg/kg) were administered orally by gavage to groups of male Wistar rats (n = 3–4), either as a single dose or as daily doses for 7 days. Tail vein blood samples (0.25 ml) were collected from all rats at 0.5, 1, 3, 6, 12, and 24 h after drug administration on day 1 or 7 of dosing. The plasma was prepared by centrifugation at 4 °C for 10 min at 1500×g within 30 min of blood sampling and analyzed for concentrations of AZD8529 or AZD8418 by a standard reverse-phase liquid chromatography and electrospray ionization tandem mass spectrometry (LC/MS/MS) method. |
| 药代性质 (ADME/PK) |
PK profiles of AZD8529 [2]
Peak plasma concentrations (T max) of AZD8418 were reached at 1 h post-administration after a single dose of 5 mg/kg. Peak plasma concentrations of AZD8529 were reached at 3 h post-administration after a single dose of 4.7 mg/kg. The peak plasma concentration (C max) for AZD8418 (690 ± 108 nM) was considerably higher than that for AZD8529 (158 ± 30 nM). Similarly, the area under the curve (AUC) for AZD8418 was also higher than that for AZD8529, indicating higher bioavailability of AZD8418 than that of AZD8529. Repeated daily administration of AZD8418 or AZD8529 for 7 days did not alter the T max or C max of plasma exposure. Based on findings of the PK studies, doses and pretreatment time were determined for AZD8418 (0, 0.37, 1.12, 3.73, 7.46, and 14.92 mg/kg; 1 h pretreatment) and AZD8529 (0, 1.75, 5.83, 17.5, and 58.3 mg/kg; 3 h pretreatment) administration to reflect differences in C max and T max.
Plasma concentrations of AZD8529 [2] In a group of squirrel monkeys (n=3), the plasma concentration of AZD8529 3 hr (the pretreatment time in the self-administration and reinstatement experiments) after drug (1 mg/kg) injections was 112±17 nM. Effect of AZD8529 on nicotine-induced dopamine release in the rat accumbens shell We determined the effect of systemic AZD8529 injections on nicotine-induced elevations of extracellular dopamine levels in accumbens shell of freely-moving rats. Nicotine (0.4 mg/kg, s.c.) increased extracellular dopamine and this effect was decreased by 30 mg/kg but not 10 mg/kg AZD8529 (Supplementary Figure S1; AZD8529 Dose x Time interaction: F(34,170)=2.24; p<0.001). When given alone, AZD8529 (10 or 30 mg/kg) had no effect on dopamine levels (Supplementary Figure S1). |
| 参考文献 |
|
| 其他信息 |
AZD8529 is under investigation in clinical trial NCT00921804 (Study to Assess the Efficacy, Safety, and Tolerability of AZD8529 in Adult Schizophrenia Patients).
Background: Based on rodent studies, group II metabotropic glutamate receptors (mGluR2 and mGluR3) were suggested as targets for addiction treatment. However, LY379268 and other group II agonists do not discriminate between the mainly presynaptic inhibitory mGluR2 (the proposed treatment target) and mGluR3. These agonists also produce tolerance over repeated administration and are no longer considered for addiction treatment. Here, we determined the effects of AZD8529, a selective positive allosteric modulator of mGluR2, on abuse-related effects of nicotine in squirrel monkeys and rats. Methods: We first assessed modulation of mGluR2 function by AZD8529 using functional in vitro assays in membranes prepared from a cell line expressing human mGluR2 and in primate brain slices. We then determined AZD8529 (.03-10 mg/kg, intramuscular injection) effects on intravenous nicotine self-administration and reinstatement of nicotine seeking induced by nicotine priming or nicotine-associated cues. We also determined AZD8529 effects on food self-administration in monkeys and nicotine-induced dopamine release in accumbens shell in rats.[1] Rationale: Numerous medication development strategies seek to decrease nicotine consumption and prevent relapse to tobacco smoking by blocking glutamate transmission. Decreasing glutamate release by activating presynaptic inhibitory metabotropic glutamate (mGlu)2/3 receptors inhibits the reinforcing effects of nicotine and blocks cue-induced reinstatement of nicotine-seeking behavior in rats. However, the relative contribution of mGlu2 receptors in nicotine dependence is still unknown. Objectives: The present study evaluated the role of mGlu2 receptors in nicotine-taking and nicotine-seeking behavior using the novel, relatively selective mGlu2 positive allosteric modulators (PAMs) AZD8418 and AZD8529. Results: Acute treatment with AZD8418 (0.37, 1.12, 3.73, 7.46, and 14.92 mg/kg) and AZD8529 (1.75, 5.83, 17.5, and 58.3 mg/kg) deceased nicotine self-administration and had no effect on food-maintained responding. Chronic treatment with AZD8418 attenuated nicotine self-administration, but tolerance to this effect developed quickly. The inhibition of nicotine self-administration by chronic AZD8529 administration persisted throughout the 14 days of treatment. Chronic treatment with either PAMs inhibited food self-administration. AZD8418 (acute) and AZD8529 (acute and subchronic) blocked cue-induced reinstatement of nicotine- and food-seeking behavior. Conclusions: These findings indicate an important role for mGlu2 receptors in the reinforcing properties of self-administered nicotine and the motivational impact of cues that were previously associated with nicotine administration (i.e., cue-induced reinstatement of nicotine-seeking behavior). Thus, mGlu2 PAMs may be useful medications to assist people to quit tobacco smoking and prevent relapse.[2] |
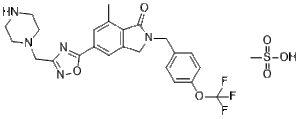
| 分子式 |
C25H28F3N5O6S
|
|---|---|
| 分子量 |
583.579935073853
|
| 精确质量 |
583.171
|
| 元素分析 |
C, 51.45; H, 4.84; F, 9.77; N, 12.00; O, 16.45; S, 5.49
|
| CAS号 |
1314217-69-0
|
| 相关CAS号 |
AZD-8529; 1092453-15-0; 1314217-69-0 (mesylate); 1344999-56-9 (mesylate hydrate)
|
| PubChem CID |
53495155
|
| 外观&性状 |
White to off-white solid powder
|
| tPSA |
147
|
| 氢键供体(HBD)数目 |
2
|
| 氢键受体(HBA)数目 |
13
|
| 可旋转键数目(RBC) |
6
|
| 重原子数目 |
40
|
| 分子复杂度/Complexity |
822
|
| 定义原子立体中心数目 |
0
|
| SMILES |
S(C)(=O)(=O)O.FC(OC1C=CC(=CC=1)CN1C(C2C(C)=CC(C3=NC(CN4CCNCC4)=NO3)=CC=2C1)=O)(F)F
|
| InChi Key |
HRHCPVNKPOTCGB-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C24H24F3N5O3.CH4O3S/c1-15-10-17(22-29-20(30-35-22)14-31-8-6-28-7-9-31)11-18-13-32(23(33)21(15)18)12-16-2-4-19(5-3-16)34-24(25,26)27;1-5(2,3)4/h2-5,10-11,28H,6-9,12-14H2,1H3;1H3,(H,2,3,4)
|
| 化学名 |
methanesulfonic acid;7-methyl-5-[3-(piperazin-1-ylmethyl)-1,2,4-oxadiazol-5-yl]-2-[[4-(trifluoromethoxy)phenyl]methyl]-3H-isoindol-1-one
|
| 别名 |
AZD-8529; AZD8529 mesylate; AZD 8529 mesylate; 1314217-69-0; AZD-8529 (mesylate); 29K1DH0MV7; 7-Methyl-5-(3-(piperazin-1-ylmethyl)-1,2,4-oxadiazol-5-yl)-2-(4-(trifluoromethoxy)benzyl)isoindolin-1-one methanesulfonate; methanesulfonic acid;7-methyl-5-[3-(piperazin-1-ylmethyl)-1,2,4-oxadiazol-5-yl]-2-[[4-(trifluoromethoxy)phenyl]methyl]-3H-isoindol-1-one; 1H-Isoindol-1-one, 2,3-dihydro-7-methyl-5-(3-(1-piperazinylmethyl)-1,2,4-oxadiazol-5-yl)-2-((4-(trifluoromethoxy)phenyl)methyl)-, methanesulfonate (1:1); AZD-8529 mesylate
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO: ~41.7 mg/mL (~71.4 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.08 mg/mL (3.56 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 20.8 mg/mL澄清DMSO储备液加入400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.08 mg/mL (3.56 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 20.8 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.08 mg/mL (3.56 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.7136 mL | 8.5678 mL | 17.1356 mL | |
| 5 mM | 0.3427 mL | 1.7136 mL | 3.4271 mL | |
| 10 mM | 0.1714 mL | 0.8568 mL | 1.7136 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT00755378 | Completed | Drug: AZD8529 Drug: Placebo |
Healthy Volunteer | AstraZeneca | September 2008 | Phase 1 |
| NCT00765492 | Completed | Drug: AZD8529 Drug: Placebo |
Healthy Volunteer | AstraZeneca | October 2008 | Phase 1 |
| NCT00886756 | Completed | Drug: AZD8529 Drug: Placebo |
Healthy | AstraZeneca | April 2009 | Phase 1 |
| NCT02401022 | Completed | Drug: AZD8529 | Tobacco Use Disorder | National Institute on Drug Abuse (NIDA) |
July 2015 | Phase 2 |
| NCT00921804 | Completed | Drug: AZD 8529 Drug: Risperidone |
Schizophrenia | AstraZeneca | June 2009 | Phase 2 |
|
AZD8529 decreased nicotine priming-induced and cue-induced reinstatement in squirrel monkeys.Biol Psychiatry. 2015 Oct 1;78(7):452-62. |
Effect of AZD8529 on nicotine and food self-administration in squirrel monkeys.Biol Psychiatry. 2015 Oct 1;78(7):452-62. |