| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| Other Sizes |
|
| 靶点 |
Indoleamine 2,3-dioxygenase 1 (IDO1) (IC50 = 1.1 nM)
|
|---|---|
| 体外研究 (In Vitro) |
当 SKOV-3 和 Jurkat 克隆 E6-1 细胞用林罗司他 (0.01-100 μM) 处理 72 小时时,活细胞的比例低于未处理的对照组。 linrodostat 的 IC50 为 6.3 μM,同样在低得多的浓度下也会导致细胞死亡[1]。
为了支持临床试验,对BMS-986205进行了临床前评估。体外特征包括在IDO-1-HEK293细胞中有效抑制犬尿氨酸(kyn)的产生(IC50=1.1 nM),但在TDO-HEK293细胞中没有,在洗脱后基于IDO1细胞的测定中持续抑制,以及在人类耐受性MLR测定中的单位数nM效力。[2] Linrodostat表现出强大的细胞活性,抑制过表达人IDO1的HEK293细胞和用IFNγ刺激的HeLa细胞中犬尿氨酸的产生,但未检测到对色氨酸2,3-双加氧酶或小鼠吲哚胺2,3-双合氧酶2的活性。Linrodostat在T细胞和表达同种异体IDO1的树突状细胞的混合淋巴细胞反应中恢复了T细胞增殖[3]。 |
| 体内研究 (In Vivo) |
根据临床前数据,预计 150 mg QD 人体剂量可最大程度地抑制 IDO1。在正在进行的临床研究中,已有 42 名患者接受了治疗。除三项 3 级毒性(自身免疫性肝炎 [剂量限制;BMS-986205 100 mg/nivo 240 mg]、皮疹和无症状低磷血症)外,所有治疗相关不良事件均为 1/2 级。第 14 天,个体谷浓度开始超过从 25 mg QD 开始的人全血 IC50,以及从 50 mg QD 开始的 IC90;所有接受 200 mg QD 治疗的患者均超过了 IC90。所有剂量下血清 kyn 均显着降低(每个剂量平均降低 > 45%),100 和 200 mg QD 剂量下平均降低 > 60%。重要的是,在可评估的配对治疗前和治疗中样本中,瘤内 kyn 减少了 90%。
人SKOV3异种移植物中Linrodostat PK/PD谱[3] 接下来,我们在小鼠异种移植物模型中使用SKOV3细胞评估了linrodostat的PK/PD特性。通过测量血清和肿瘤内犬尿氨酸水平来评估林罗多司坦的剂量依赖性PD活性,每天给药一次,剂量为5、25或125 mg/kg(补充表S1;PK报告为AUC0-24,μmol/L×h)。在5、25和125 mg/kg的剂量下,林罗达治疗的肿瘤中犬尿氨酸减少百分比的AUEC测量值分别为60%、63%和76%,表明肿瘤中存在剂量依赖性PD活性。在评估的时间点中,治疗后6小时观察到最大的PD效应(犬尿氨酸减少96%)(图4A)。在最后一次服用10mg/kg林罗司他和100mg/kg依帕卡多斯塔后24小时,犬尿氨酸水平保持降低(≥30%)。根据这些PK/PD分析,利诺司他在SKOV3肿瘤血清中的体内IC50中值为3.4 nmol/L,与人全血中的体外IC50中值9.4 nmol/L相似(图4B)。我们还检测了另一种IDO1抑制剂依帕卡多斯塔的效力,并检测到体内和体外的IC50中值分别为227和163 nmol/L(图4C)。这些数据表明,linrodostat显示出个位数的纳摩尔效力。 |
| 酶活实验 |
IDO1抑制[3]
用含有1mmol/L色氨酸、50μmol/L琥珀酰丙酮和50ng/mL人IFNγ 的培养基处理SKOV3人癌症细胞(ATCC)以诱导IDO1合成,并用10、50或100nmol/L的载体(DMSO)、Linrodostat /林洛司他或依帕洛司他 处理72小时。用Ehrlich比色法测定犬尿氨酸水平。用平板读数器(490nm)检测比色变化。根据犬尿氨酸标准曲线测定犬尿氨素浓度。 IDO1抑制的逆转[3] SKOV3细胞用5μg/mL环己酰亚胺处理以防止IDO1的进一步合成,并用50μmol/L琥珀酰丙酮孵育。将培养基替换为含有1 mmol/L色氨酸、50μmol/L琥珀酰丙酮和5μg/mL环己酰亚胺的培养基,并用载体(DMSO)或10μmol/L血红素处理重复培养基。如上所述,在0、2、4、6、8和10小时时测量犬尿氨酸水平。 芳烃受体测定[3] 根据制造商的说明使用人类AhR报告检测系统(96孔格式)。将分配到96孔板中的报告细胞立即给予2,3,7,8-四氯二苯并对二恶英(TCDD;1或10 nmol/L)、犬尿氨酸(1或10μmol/L)或林诺司他(1或0μmol/L)。孵育22至24小时后,取出培养基,加入萤光素酶检测试剂(100μL)。约5分钟后,使用板读数光度计检测每个孔的萤光素酶活性。 SKOV-3 IDO1测定(细胞平板、IDO1诱导、犬尿氨酸测定)[1] 细胞以3×104个细胞/孔的速度铺板,并允许其附着过夜。第二天,将IFNγ以100ng/mL的终浓度加入细胞培养物中以诱导IDO1表达,然后在37°C和5%CO2下孵育24小时。 使用犬尿氨酸标准曲线来插值试验样品中的犬尿氨素浓度。 半胱天冬酶3/7激活[1] 根据制造商的说明,使用Promega的Caspase 3/7 Glo试剂测量Caspase 3/6的活性。 |
| 细胞实验 |
基于细胞的检测中的半最大抑制浓度[3]
研究中使用的所有细胞系都进行了支原体常规检测,并按照标准方案跟踪传代。使用含有10%胎牛血清(FBS)的RPMI无酚红培养基接种过表达人IDO1、人TDO、小鼠IDO1或小鼠Ido2的HEK293细胞。Linrodostat 的制备方法如专利合作条约国际申请WO 2016073774(实施例19;参考文献32,33)中所述。加入Linrodostat(100 nL;10μmol/L–10 pmol/L),在37°C的5%CO2中孵育细胞20小时。使用含有10%FBS的RPMI无酚红培养基接种HeLa或M109细胞。加入Linrodostat(50μL;10μmol/L–10 pmol/L),细胞在37°C下孵育2小时。加入重组人IFNγ(终浓度,10ng/mL)或重组小鼠IFNγ,终浓度,5ng/mL,以诱导IDO1。细胞在37°C的5%CO2中孵育18小时。停止治疗,计算IC50值。 相对存活率测定[1] 根据制造商的说明,使用Cell Titer Fluro 评估细胞存活率。根据未处理对照的读数计算相对细胞存活率。%相对存活率=试验值/未治疗对照值×100。 细胞活力测定[1] 细胞类型: SKOV-3 和 Jurkat 克隆 E6-1 细胞 测试浓度: 0.01-100 μM <孵化持续时间:72小时 实验结果:与未处理的对照相比,活细胞数量减少,并在低得多的浓度下诱导细胞死亡。 |
| 动物实验 |
During dose escalation, patients (pts) with advanced cancers were treated in escalating cohorts with BMS-986205 (25-200 mg as of Jan 5, 2017) orally once daily (QD) for 2 wk, followed by BMS-986205 + nivo 240 mg IV every 2 wk. Objectives included safety (primary), PK, and PD. [2]
Human SKOV3 xenograft tumor model [3] Female nu/nu mice (7–12 weeks old; Envigo) received food and water ad libitum and were maintained in a controlled environment according to Association for Assessment and Accreditation of Laboratory Animal Care International regulations. SKOV3 cells were maintained in RPMI 1640 with 10% FBS and were harvested in the log growth phase (6 × 107 cells/mL in Hank's balanced salt solution), mixed 1:1 with Matrigel, and s.c. implanted into the mouse flank (0.1 mL or 3 × 106 cells/mouse). After implantation (15 days), tumor volumes were measured, and tumor-bearing mice were randomized (five animals/group). Linrodostat was formulated as a solution in the vehicle ethanol/polyethylene glycol (PEG) 400/propylene glycol/d-α-tocopheryl PEG 1000 succinate (volume ratio, 5:55:20:20). Each group was orally administered a vehicle, Linrodostat (5, 25, or 125 mg/kg once a day), or epacadostat (30 or 100 mg/kg twice daily), for 5 days. Tumor volumes were measured before tumors were snap frozen. Sera were harvested (day 5) at designated times after dosing to quantify kynurenine and compound levels. PK analyses [3] PK parameters were determined by a noncompartmental model of analysis of plasma concentration versus time data using Phoenix 6.3.0.395. AUCs from time zero to last sampling time (AUC0-T) and time zero to infinity (AUCINF) were calculated using the linear-log trapezoidal method. The total plasma clearance (CLTp), steady-state volume of distribution (Vss), and apparent elimination half-life (t1/2) were estimated after IV administration. t1/2 estimations were calculated at ≥ 3 time points. The total blood clearance (CLTb) was calculated as the CLTp divided by the blood-to-plasma concentration ratio. The absolute oral bioavailability (F) was estimated as the ratio of dose-normalized AUCs following oral and IV doses. |
| 药代性质 (ADME/PK) |
Linrodostat PK profile in vivo [3]
To extend these SKOV3 xenograft studies, we assessed PK parameters of IV and oral linrodostat in higher species including rat, dog, and monkey (Table 1). After IV administration, the CLTp of linrodostat was comparable across species, with levels of 27, 25, and 19 mL/min/kg in rats, dogs, and monkeys, respectively. The CLTp were ≤ 48% of the respective reported liver blood flows, indicating that linrodostat has low-to-moderate systemic clearance. After IV administration, Vss values in rats, dogs, and monkeys were 3.8, 5.7, and 4.1 L/kg, respectively, indicating extravascular distribution. The t1/2 of linrodostat was 3.9, 4.7, and 6.6 hours in rats, dogs, and monkeys, respectively. After oral administration, the Tmax ranged from 0.5 to 1.7 hours in rats, dogs, and monkeys. The absolute oral bioavailability of linrodostat given as a solution was 64%, 39%, and 10% in rats, dogs, and monkeys, respectively. The rate of linrodostat metabolism by hepatocytes was higher in rats than dogs, monkeys, and humans. Based on the in vitro–in vivo correlation of hepatocyte clearance in animal species, clearance in humans is projected to be moderate. These data lead to a projected human t1/2 of 23 hours, supporting dosing once a day in a clinical setting. To extend these preclinical, in vivo PD/PK studies, we assessed kynurenine PD with linrodostat + nivolumab treatment in patients with advanced cancers. Substantial decreases in mean serum kynurenine levels were detected at all linrodostat doses evaluated, with an approximately 60% reduction observed with 100 and 200 mg once a day (Fig. 5A and B). Furthermore, pre- and on-treatment tumor samples from 13 patients demonstrated that intratumoral kynurenine levels were reduced across all doses following treatment, even in the presence of relatively high pretreatment kynurenine levels (Fig. 5C). These results demonstrate that linrodostat + nivolumab leads to substantial reductions in serum and intratumoral kynurenine levels. |
| 参考文献 |
|
| 其他信息 |
Linrodostat is under investigation in clinical trial NCT03247283 (Pharmacokinetics and Metabolism Study in Healthy Male Participants).
Linrodostat is an orally available inhibitor of indoleamine 2,3-dioxygenase 1 (IDO1), with potential immunomodulating and antineoplastic activities. Upon administration, linrodostat specifically targets and binds to IDO1, a cytosolic enzyme responsible for the oxidation of the amino acid tryptophan into the immunosuppressive metabolite kynurenine. By inhibiting IDO1 and decreasing kynurenine in tumor cells, BMS-986205 restores and promotes the proliferation and activation of various immune cells, including dendritic cells (DCs), natural killer (NK) cells, and T-lymphocytes, and causes a reduction in tumor-associated regulatory T-cells (Tregs). Activation of the immune system, which is suppressed in many cancers, may induce a cytotoxic T-lymphocyte (CTL) response against the IDO1-expressing tumor cells, thereby inhibiting the growth of IDO1-expressing tumor cells. IDO1, overexpressed by multiple tumor cell types, plays an important role in immunosuppression. Tryptophan depletion inhibits T-lymphocyte proliferation and activation, and subsequently suppresses the immune system. Indoleamine 2,3-dioxygenase 1 (IDO1) is a new immune-oncology target and its inhibitors have shown promise in the clinic especially in combination with other immune-stimulating agents. Here we describe two robust cell-based assays for screening IDO1 inhibitors. Both assays can be easily adopted by most laboratories and utilized for screening of IDO1 inhibitors. Endogenous IDO1 expression is induced in a cancer cell line with interferon gamma and its activity is assessed by measuring kynurenine secreted into the media. The effect of cancer cell IDO1 induction and inhibition on T cell activation is evaluated in a co-culture assay using Jurkat T cell line. Additional readouts assessing cell viability are employed for early detection of false positive IDO1 inhibitors and toxic compounds. Clinical candidates epacadostat and BMS-986205 were evaluated in the assays as control compounds, the former can completely inhibit IDO1 activity while the maximum effect of the later is limited (to about 80% in our system) consistent with the differences in their interaction with IDO1. Nanomolar concentrations of both compounds rescued IDO1 mediated inhibition of T cell activation. However, treatment with micromolar concentrations of BMS-986205 blocked Jurkat T cell activation and after prolonged incubation induced cell death.[1] Background: IDO1 is highly expressed in multiple cancers and may be an immunosuppressive mechanism for tumor escape via its production of metabolites that inhibit T-cell function. Nivo, a mAb that targets PD-1, causes IDO1 upregulation, supporting a rationale for combining it with an IDO1 inhibitor. Our preclinical program aimed to identify a best in class IDO1 inhibitor with favorable pharmacokinetic (PK) characteristics (Hunt J, et al. AACR 2017 [abst 6774]). Here we present BMS-986205, a selective IDO1 inhibitor validated in a novel phase 1/2a trial alone and in combination with nivo. Methods: During dose escalation, patients (pts) with advanced cancers were treated in escalating cohorts with BMS-986205 (25-200 mg as of Jan 5, 2017) orally once daily (QD) for 2 wk, followed by BMS-986205 + nivo 240 mg IV every 2 wk. Objectives included safety (primary), PK, and PD. Preclinical analyses included measurement of enzyme inhibition in HEK293 cells overexpressing human IDO1 or tryptophan 2,3-dioxygenase (TDO) and IFNγ-stimulated HeLa cells. Results: In support of clinical testing, BMS-986205 was evaluated preclinically. In vitro characteristics included potent inhibition of kynurenine (kyn) production in IDO1-HEK293 cells (IC50 = 1.1 nM) but not in TDO-HEK293 cells, sustained inhibition in IDO1 cell-based assays after washout, and single-digit nM potency in human tolerogenic MLR assays. Based on preclinical data, a 150 mg QD human dose was projected to maximally inhibit IDO1. In the ongoing clinical study, 42 pts have been treated. All treatment-related adverse events were grade 1/2 except three grade 3 toxicities (autoimmune hepatitis [dose limiting; BMS-986205 100 mg/nivo 240 mg], rash, and asymptomatic hypophosphatemia). Day 14 individual trough concentrations began exceeding the human whole blood IC50 starting with 25 mg QD, and the IC90 starting with 50 mg QD; all pts treated at 200 mg QD exceeded the IC90. Serum kyn was substantially reduced at all doses (> 45% mean reduction at each dose), with > 60% mean reduction at the 100 and 200 mg QD doses. Importantly, intratumoral kyn was reduced up to 90% in evaluable paired pre- and on-treatment samples. Conclusions: BMS-986205 is an optimized, once-daily, selective and potent oral IDO1 inhibitor at clinically relevant concentrations. It is well tolerated up to at least 200 mg in combination with nivo in this novel trial. Evidence of substantial serum kyn reduction was observed at doses as low as 25 mg QD; inhibition at 100 and 200 mg QD appears greater than that reported for other in-class compounds. In addition, we have presented the first evidence of intratumoral kyn reduction by an IDO1 inhibitor. These data suggest the potential of BMS-986205 as an IDO1 inhibitor with superior PD properties and support further evaluation in combination with nivo.[2] Tumors can exploit the indoleamine 2,3-dioxygenase 1 (IDO1) pathway to create an immunosuppressive microenvironment. Activated IDO1 metabolizes tryptophan into immunosuppressive kynurenine, leading to suppressed effector T-cell (Teff) proliferation, allowing for tumor escape from host immune surveillance. IDO1 inhibition counteracts this immunosuppressive tumor microenvironment and may improve cancer outcomes, particularly when combined with other immunotherapies. Linrodostat mesylate (linrodostat) is a potent, selective oral IDO1 inhibitor that occupies the heme cofactor-binding site to prevent further IDO1 activation and is currently in multiple clinical trials for treatment of patients with advanced cancers. Here, we assess the in vitro potency, in vivo pharmacodynamic (PD) activity, and preclinical pharmacokinetics (PKs) of linrodostat. Linrodostat exhibited potent cellular activity, suppressing kynurenine production in HEK293 cells overexpressing human IDO1 and HeLa cells stimulated with IFNγ, with no activity against tryptophan 2,3-dioxygenase or murine indoleamine 2,3-dioxygenase 2 detected. Linrodostat restored T-cell proliferation in a mixed-lymphocyte reaction of T cells and allogeneic IDO1-expressing dendritic cells. In vivo, linrodostat reduced kynurenine levels in human tumor xenograft models, exhibiting significant PD activity. Linrodostat demonstrated a PK/PD relationship in the xenograft model, preclinical species, and samples from patients with advanced cancers, with high oral bioavailability in preclinical species and low to moderate systemic clearance. Our data demonstrate that linrodostat potently and specifically inhibits IDO1 to block an immunosuppressive mechanism that could be responsible for tumor escape from host immune surveillance with favorable PK/PD characteristics that support clinical development.[3] |
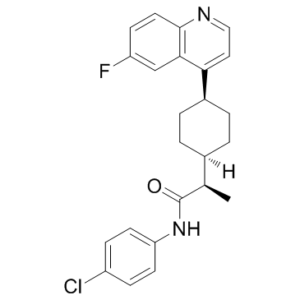
| 分子式 |
C24H24CLFN2O
|
|
|---|---|---|
| 分子量 |
410.9116
|
|
| 精确质量 |
410.156
|
|
| 元素分析 |
C, 70.15; H, 5.89; Cl, 8.63; F, 4.62; N, 6.82; O, 3.89
|
|
| CAS号 |
1923833-60-6
|
|
| 相关CAS号 |
1923833-60-6;2221034-29-1 (mesylate);1791396-46-7 (dimesylate );
|
|
| PubChem CID |
121328278
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| LogP |
6.5
|
|
| tPSA |
42
|
|
| 氢键供体(HBD)数目 |
1
|
|
| 氢键受体(HBA)数目 |
3
|
|
| 可旋转键数目(RBC) |
4
|
|
| 重原子数目 |
29
|
|
| 分子复杂度/Complexity |
545
|
|
| 定义原子立体中心数目 |
1
|
|
| SMILES |
ClC1C=CC(=CC=1)NC([C@H](C)C1CCC(C2C=CN=C3C=CC(=CC=23)F)CC1)=O
|
|
| InChi Key |
KRTIYQIPSAGSBP-KLAILNCOSA-N
|
|
| InChi Code |
InChI=1S/C24H24ClFN2O/c1-15(24(29)28-20-9-6-18(25)7-10-20)16-2-4-17(5-3-16)21-12-13-27-23-11-8-19(26)14-22(21)23/h6-17H,2-5H2,1H3,(H,28,29)/t15-,16?,17?/m1/s1
|
|
| 化学名 |
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 2.5 mg/mL (6.08 mM) in 5% DMSO + 40% PEG300 + 5% Tween80 + 50% Saline (这些助溶剂从左到右依次添加,逐一添加), 悬浮液;超声助溶。
*生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: 2.5 mg/mL (6.08 mM) in 5% DMSO + 95% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 悬浊液; 超声助溶。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.08 mg/mL (5.06 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: 2.08 mg/mL (5.06 mM) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 悬浊液; 超声助溶。 例如,若需制备1 mL的工作液,可将100μL 20.8mg/mL澄清的DMSO储备液加入到900μL 20%SBE-β-CD生理盐水中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 配方 5 中的溶解度: ≥ 2.08 mg/mL (5.06 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将100 μL 20.8 mg/mL 澄清 DMSO 储备液加入到 900 μL 玉米油中并混合均匀。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.4336 mL | 12.1681 mL | 24.3362 mL | |
| 5 mM | 0.4867 mL | 2.4336 mL | 4.8672 mL | |
| 10 mM | 0.2434 mL | 1.2168 mL | 2.4336 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。