| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| Other Sizes |
|
| 体外研究 (In Vitro) |
体外活性:多非利特可阻断非洲爪蟾卵母细胞大斑块中的 HERG 电流。通过 200 毫秒测试脉冲和 IKr 失活尾电流分析测量,多非利特 (1 μM) 将豚鼠心肌细胞中 IKr 的幅度降低至对照电流的 61%。多非利特增加了复极的心尖-基底差异,因为在完整的犬心脏中,心尖部的 ERP 比基部的 ERP 增加更显着。
|
|---|---|
| 体内研究 (In Vivo) |
多非利特(Dofetilide,3~100 μg/kg;iv)选择性延长激活-复极延迟,同时保持激活时间不变,从而延长复极时间[2]。肾脏排出多种无活性的极性代谢物,这些代谢物是 CYP3A4 代谢多非利特时产生的[1]。
|
| 动物实验 |
Animal/Disease Models: Adult beagle dogs (13-15 kg)[2]
Doses: 3~100 μg/kg Route of Administration: Iv Experimental Results: Increased repolarisation time via a selective prolongation of activation repolarisation interval, activation time being unchanged. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
>90% 3 L/kg Approximately 80% of a single dose of dofetilide is excreted in urine, of which approximately 80% is excreted as unchanged dofetilide with the remaining 20% consisting of inactive or minimally active metabolites. Renal elimination involves both glomerular filtration and active tubular secretion (via the cation transport system, a process that can be inhibited by cimetidine, trimethoprim, prochlorperazine, megestrol and ketoconazole). ... The oral bioavailability of dofetilide is >90%, with maximal plasma concentrations occurring at about 2-3 hours in the fasted state. Oral bioavailability is unaffected by food or antacid. The terminal half life of Tikosyn is approximately 10 hours; steady state plasma concentrations are attained within 2-3 days, with an accumulation index of 1.5 to 2.0. Plasma concentrations are dose proportional. Plasma protein binding of dofetilide is 60-70%, is independent of plasma concentration, and is unaffected by renal impairment. Volume of distribution is 3 L/kg. 1. Pharmacokinetics of dofetilide were studied in man, dog, rat and mouse after single IV and oral doses of dofetilide or (14)C-dofetilide. 2. Dofetilide was absorbed completely in all species. Low metabolic clearance in man resulted in complete bioavailability following oral administration. Higher metabolic clearance in rodents, and to a lesser extent dogs, resulted in decreased bioavailability because of first-pass metabolism. 3. Following IV administration, the volume of distribution showed only moderate variation in all species (2.8-6.3 l/kg). High plasma clearance in rodents resulted in short half-life values (mouse 0.32, male rat 0.5 and female rat 1.2 hr), while lower clearance in dog and man gave longer terminal elimination half-lives (4.6 and 7.6 hr respectively). 4. After single IV doses of (14)C-dofetilide, unchanged drug was the major component excreted in urine of all species with several metabolites also present. 5. Metabolites identified in urine from all species were formed by N-oxidation or N-dealkylation of the tertiary nitrogen atom of dofetilide. 6. After oral and IV administration of (14)C-dofetilide to man, parent compound was the only detectable component present in plasma and represented 75% of plasma radioactivity. No single metabolite accounted for greater than 5% of plasma radioactivity. Metabolism / Metabolites Hepatic Dofetilide, a class III antidysrhythmic agent, undergoes both renal and metabolic clearance. Characterization of the metabolism in vitro allows explanation of species differences, whereas identification of the human enzymes involved permits assessment of potential drug interaction. In liver microsomes, the rate of oxidative metabolism of dofetilide is in the order: male rat > female rat > dog > humans, which correlates with the metabolic clearance seen in vivo. In vitro products of oxidative metabolism, formed by N-dealkylation, are the same as those formed in vivo, with the N-desmethyl being the major product. This route of dofetilide metabolism is mediated by cytochrome P450 (CYP). In humans, N-demethylation has a high KM of 657 +/- 116 uM, indicating low affinity for the enzyme's active site. In a number of human liver microsomal preparations, this rate correlated (r = 0.903) with the activity of CYP3A4. There was no correlation with the activities of other isozymes. Specific isozyme inhibitors also indicated the involvement of CYP3A4, with partial inhibition being observed with ketoconazole and troleandeomycin, whereas the activator, alpha-naphthaflavone, caused increased turnover. No inhibition was observed with specific inhibitors or competing substrates for other isozymes. Dofetilide did not significantly inhibit CYP2C9, CYP2D6, or CYP3A4 at concentrations up to 100 microM in vitro. In contrast, amiodarone (IC50, 25 uM) and flecainide (49 microM) inhibited CYP2C9 and quinidine (0.26 uM), and flecainide (0.44 uM) inhibited CYP2D6. Many antidysrhythmic drugs have active, circulating metabolites, complicating the relationship of dose and clinical response. In vitro pharmacology studies allow assessment of the potential contribution to the pharmacological profile by metabolites. Potency of dofetilide and metabolites has been compared for class III (K+ channel blockade) and class I (Na+ channel blockade) antidysrhythmic activities. Three of the metabolites of dofetilide displayed class III activity but at concentrations at least 20-fold higher than dofetilide. Dofetilide N-oxide showed class I activity, but only at high concentration. Neither resting membrane potential or action potential amplitude were affected by any metabolite. This lack of biologically relevant activity is in accord with the close correlation between plasma concentrations of dofetilide and pharmacological response. Approximately 80% of a single dose of dofetilide is excreted in urine, of which approximately 80% is excreted as unchanged dofetilide with the remaining 20% consisting of inactive or minimally active metabolites. ... In vitro studies with human liver microsomes show that dofetilide can be metabolized by CYP3A4, but it has a low affinity for this isoenzyme. Metabolites are formed by N-dealkylation and N-oxidation. There are no quantifiable metabolites circulating in plasma, but 5 metabolites have been identified in urine Biological Half-Life 10 hours Following IV administration, ... high plasma clearance in rodents resulted in short half-life values (mouse 0.32, male rat 0.5 and female rat 1.2 hr), while lower clearance in dog and man gave longer terminal elimination half-lives (4.6 and 7.6 hr respectively). ... The terminal half life of Tikosyn is approximately 10 hours |
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
In clinical trials, serum aminotransferase and alkaline phosphatase elevations were no more common during dofetilide than placebo therapy. Some degree of ALT elevation was reported in 15% of dofetilide but a similar proportion of placebo recipients; these elevations were above 3 times the upper limit of normal in 1.5% vs 2.0%. Thus, the background rate of serum ALT elevations in patients with atrial fibrillation eligible for dofetilide treatment appears to be high. Despite this, dofetilide has not been linked to instances of clinically apparent liver injury with symptoms or jaundice. The product label for dofetilide does not mention hepatotoxicity and does not specifically recommend monitoring of liver tests. Likelihood score: E (unlikely cause of clinically apparent liver injury). Protein Binding 60% -70% Interactions Concomitant use of verapamil is contraindicated. Co-administration of Tikosyn with verapamil resulted in increases in dofetilide peak plasma levels of 42%, although overall exposure to dofetilide was not significantly increased. In an analysis of the supraventricular arrhythmia and The Danish Investigations of Arrhythmia and Mortality on Dofetilide (DIAMOND) patient populations, the concomitant administration of verapamil with dofetilide was associated with a higher occurrence of torsade de pointes. Concomitant use of cimetidine is contraindicated. Cimetidine at 400 mg BID (the usual prescription dose) co-administered with Tikosyn (500 mcg BID) for 7 days has been shown to increase dofetilide plasma levels by 58%. Cimetidine at doses of 100 mg BID (OTC dose) resulted in a 13% increase in dofetilide plasma levels (500 mcg single dose). No studies have been conducted at intermediate doses of cimetidine. If a patient requires Tikosyn and anti-ulcer therapy, it is suggested that omeprazole, ranitidine, or antacids (aluminum and magnesium hydroxides) be used as alternatives to cimetidine, as these agents have no effect on the pharmacokinetic profile of Tikosyn. The use of Tikosyn in conjunction with other drugs that prolong the QT interval has not been studied and is not recommended. Such drugs include phenothiazines, cisapride, bepridil, tricyclic antidepressants, certain oral macrolides, and certain fluoroquinolones. Class I or Class III antiarrhythmic agents should be withheld for at least three half-lives prior to dosing with Tikosyn. In clinical trials, Tikosyn was administered to patients previously treated with oral amiodarone only if serum amiodarone levels were below 0.3 mg/L or amiodarone had been withdrawn for at least three months. Hypokalemia or hypomagnesemia may occur with administration of potassium-depleting diuretics, increasing the potential for torsade de pointes. Potassium levels should be within the normal range prior to administration of Tikosyn and maintained in the normal range during administration of Tikosyn. For more Interactions (Complete) data for Dofetilide (15 total), please visit the HSDB record page. |
| 参考文献 | |
| 其他信息 |
Therapeutic Uses
Anti-Arrhythmia Agents, Potassium Channel Blockers Tikosyn is indicated for the conversion of atrial fibrillation and atrial flutter to normal sinus rhythm. /Included in US product label/ Tikosyn is indicated for the maintenance of normal sinus rhythm (delay in time to recurrence of atrial fibrillation/atrial flutter (AF/AFl)) in patients with atrial fibrillation/atrial flutter of greater than one week duration who have been converted to normal sinus rhythm. Because Tikosyn can cause life threatening ventricular arrhythmias, it should be reserved for patients in whom atrial fibrillation/atrial flutter is highly symptomatic. /Included in US product label/ Drug Warnings /BOXED WARNING/ To minimize the risk of induced arrhythmia, patients initiated or re-initiated on Tikosyn should be placed for a minimum of 3 days in a facility that can provide calculations of creatinine clearance, continuous electrocardiographic monitoring, and cardiac resuscitation ... . Tikosyn is available only to hospitals and prescribers who have received appropriate Tikosyn dosing and treatment initiation education; Tikosyn (dofetilide) can cause serious ventricular arrhythmias, primarily torsade de pointes (TdP) type ventricular tachycardia, a polymorphic ventricular tachycardia associated with QT interval prolongation. QT interval prolongation is directly related to dofetilide plasma concentration. Factors such as reduced creatinine clearance or certain dofetilide drug interactions will increase dofetilide plasma concentration. The risk of TdP can be reduced by controlling the plasma concentration through adjustment of the initial dofetilide dose according to creatinine clearance and by monitoring the ECG for excessive increases in the QT interval. Treatment with dofetilide must therefore be started only in patients placed for a minimum of three days in a facility that can provide electrocardiographic monitoring and in the presence of personnel trained in the management of serious ventricular arrhythmias. Calculation of the creatinine clearance for all patients must precede administration of the first dose of dofetilide. In patients with mild to moderate renal failure, decreases in dosage based on creatinine clearance are required to minimize the risk of torsades de pointes. The drug should not be used in patients with advanced renal failure or with inhibitors of renal cation transport. Torsades de pointes occurred in 1-3% of patients in clinical trials where strict exclusion criteria (e.g., hypokalemia) were applied and continuous ECG monitoring was used to detect marked QT prolongation in the hospital. The incidence of this adverse effect during more widespread use of the drug, marketed since 2000, is unknown. Other adverse effects were no more common than with placebo during premarketing clinical trials. For more Drug Warnings (Complete) data for Dofetilide (16 total), please visit the HSDB record page. Pharmacodynamics Dofetilide is an antiarrhythmic drug with Class III (cardiac action potential duration prolonging) properties and is indicated for the maintenance of normal sinus rhythm. Dofetilide increases the monophasic action potential duration in a predictable, concentration-dependent manner, primarily due to delayed repolarization. At concentrations covering several orders of magnitude, Dofetilide blocks only IKr with no relevant block of the other repolarizing potassium currents (e.g., IKs, IK1). At clinically relevant concentrations, Dofetilide has no effect on sodium channels (associated with Class I effect), adrenergic alpha-receptors, or adrenergic beta-receptors. |
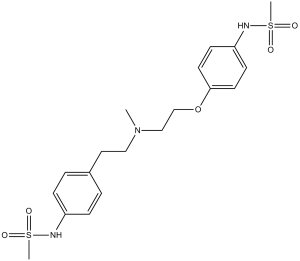
| 分子式 |
C19H27N3O5S2
|
|
|---|---|---|
| 分子量 |
441.56
|
|
| 精确质量 |
441.139
|
|
| CAS号 |
115256-11-6
|
|
| 相关CAS号 |
Dofetilide-d4;1189700-56-8
|
|
| PubChem CID |
71329
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 密度 |
1.3±0.1 g/cm3
|
|
| 沸点 |
614.1±65.0 °C at 760 mmHg
|
|
| 熔点 |
147-1490C
|
|
| 闪点 |
325.2±34.3 °C
|
|
| 蒸汽压 |
0.0±1.8 mmHg at 25°C
|
|
| 折射率 |
1.614
|
|
| LogP |
1.56
|
|
| tPSA |
121.57
|
|
| 氢键供体(HBD)数目 |
2
|
|
| 氢键受体(HBA)数目 |
8
|
|
| 可旋转键数目(RBC) |
11
|
|
| 重原子数目 |
29
|
|
| 分子复杂度/Complexity |
672
|
|
| 定义原子立体中心数目 |
0
|
|
| InChi Key |
IXTMWRCNAAVVAI-UHFFFAOYSA-N
|
|
| InChi Code |
InChI=1S/C19H27N3O5S2/c1-22(13-12-16-4-6-17(7-5-16)20-28(2,23)24)14-15-27-19-10-8-18(9-11-19)21-29(3,25)26/h4-11,20-21H,12-15H2,1-3H3
|
|
| 化学名 |
N-(4-(2-(methyl(2-(4-(methylsulfonamido)phenoxy)ethyl)amino)ethyl)phenyl)methanesulfonamide
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (5.66 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (5.66 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (5.66 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.2647 mL | 11.3235 mL | 22.6470 mL | |
| 5 mM | 0.4529 mL | 2.2647 mL | 4.5294 mL | |
| 10 mM | 0.2265 mL | 1.1323 mL | 2.2647 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。