| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg | |||
| 100mg | |||
| Other Sizes |
| 靶点 |
Tubulin polymerization; microtubule
|
|---|---|
| 体外研究 (In Vitro) |
Eribulin (1-100 nM; 72 h) 抑制细胞生长,对于 LM8 和 Dunn 细胞的 IC50 值分别为 22.8 和 21.5 nM [1]。 Eribulin(10-50 nM;12-72 小时)以 50 nM 剂量持续 24 小时可显着促进 LM8 细胞的早期凋亡 [1]。在 LM8 细胞中,艾日布林(10-50 nM;12-72 小时)在 50 nM 下产生 G2/M 期阻滞 12 小时,而在 10 nM 下长期治疗(72 小时)不会诱导 G2/M 期阻滞[1 ]。艾日布林(1-50 nM;12 小时)不会促进 LM8 细胞衰老 [1]。艾日布林(1-10 nM;16 小时)在 LM8 细胞中产生形态改变并在低浓度下抑制细胞迁移 [1]。
|
| 体内研究 (In Vivo) |
艾日布林(1 mg/kg;每周静脉注射一次,持续 2 周)可抑制大鼠骨肉瘤的初始肿瘤发展和肺转移 [1]。低剂量时,艾日布林(1 mg/kg;静脉注射一次)可抑制循环肿瘤细胞 (CTC) 的发育 [1]。
Eribulin mesylate (1-100 nM; 72 h) 抑制细胞生长,对于 LM8 和 Dunn 细胞的 IC50 值分别为 22.8 和 21.5 nM[1]。 Eribulin mesylate(10-50 nM;12-72 小时)可显着促进以 50 nM 剂量处理 24 小时的 LM8 细胞的早期凋亡[1]。在 LM8 细胞中,甲磺酸艾日布林(10-50 nM;12-72 小时)在 50 nM 下诱导 G2/M 期停滞 12 小时,而长期治疗在 10 nM(72 小时)不会诱导 G2/M 期停滞[1]。 Eribulin mesylate(1-50 nM;12 小时)不会促进 LM8 细胞衰老 [1]。 Eribulin mesylate(1-10 nM;16 小时)在低浓度下会产生形态改变并抑制 LM8 细胞的细胞迁移 [1]。
因此,在这项研究中,我们研究了微管抑制剂甲磺酸艾立布林(eribulin mesylate)对骨肉瘤肺转移的抑制作用。在浓度>增殖IC50时,艾里布林诱导转移性骨肉瘤细胞系LM8的细胞周期阻滞和凋亡。然而,在浓度<增殖IC50(低剂量)时,艾里布林改变了细胞形态并减少了LM8的迁移。低浓度的eribulin也降低了迁移过程中的方向性、腺瘤性息肉病大肠杆菌蛋白的外周定位和局灶性粘连的周转。在三维胶原培养系统中,低浓度的艾里布林抑制了肿瘤细胞增殖和集落形成。[1] Eribulin甲磺酸酯(E7389),一种海洋天然产物卤球粒蛋白B的合成类似物,正在进行治疗癌症的III期临床试验。Eribulin靶向微管,通过抑制微管生长来抑制微管+末端的动态不稳定性,而对缩短几乎没有影响或没有影响[Jordan,M.A.,et al.(2005)Mol.癌症Ther.41086-105]。使用[(3)H]艾里布林,我们发现艾里布林在单个位点结合可溶性微管蛋白;然而,这种结合是复杂的,总K(d)为46微M,但对25%的微管蛋白亚群也显示出真正的或明显的非常高的亲和力(K(d=0.4微M)。Eribulin还以每微管14.7+/-1.3个分子的最大化学计量比结合微管(K(d)=3.5微M),强烈表明微管末端存在相对较高的亲和力结合位点。在100 nM的浓度下,抑制微管+末端生长50%的浓度,我们发现每两个微管结合一个艾里布林分子,这表明在微管末端结合一个艾里布林分子可以有效地抑制其生长。Eribulin不能抑制微管负端的动态不稳定性。微管与2或4微M长春花碱预孵育诱导了额外的低亲和力艾里布林结合位点,最有可能在张开的微管末端。总的来说,我们的结果表明,艾里布林与微管正端结合具有高亲和力,从而抑制了动态不稳定性。[2] Eribulin(E7389)是癌症III期临床试验中卤软骨蛋白B的合成类似物,与微管蛋白和微管结合。在低浓度下,它抑制间期细胞中微管动态不稳定的生长期,阻止有丝分裂,并诱导细胞凋亡,这表明抑制纺锤体微管动态会诱导有丝分裂阻滞。为了进一步验证这一假设,我们通过延时共聚焦显微镜在活的有丝分裂U-2 OS人骨肉瘤细胞中测量了艾里布林对着丝粒及其附着的动粒微管动力学的影响。绿色荧光蛋白标记的着丝粒结合蛋白B标记着丝粒和动粒微管加末端。在对照细胞中,姐妹染色单体着丝粒对在张力下交替增加和减少分离(拉伸和放松)。Eribulin在阻止有丝分裂的浓度下抑制着丝粒动力学。在60 nmol/L的eribulin(2倍有丝分裂IC(50))下,松弛率被抑制了21%,暂停时间增加了67%,动态性降低了35%(但平均着丝粒间距没有减少),表明eribulin降低了运动粒处正常的微管依赖性纺锤体张力,阻止了有丝分裂检查点通过的信号。我们还研究了一种更有效但在肿瘤中效果较差的抗增殖线粒体衍生物ER-076349。在2 x IC(50)(4 nmol/L)时,有丝分裂阻滞也与着丝粒动力学的抑制同时发生。尽管两种化合物的培养基IC(50)值相差15倍,但细胞内浓度相似,表明与艾里布林相比,ER-076349在细胞中的相对摄取更广泛。动粒微管动力学的抑制与有丝分裂阻滞之间的强相关性表明,eribulin阻断有丝分裂的主要机制是抑制纺锤体微管动力学。[3] Eribulin(E7389),一种机制独特的微管抑制剂,在癌症的III期临床试验中,相对于更有效的化合物ER-076349,在体内表现出优异的疗效,这一事实无法通过不同的药代动力学特性来解释。通过观察,提出了一种基于细胞的药效学解释,即使用全剂量/反应治疗的流式细胞术有丝分裂阻滞可逆性测定表明,艾里布林(而非ER-076349)诱导的有丝分裂阻断是不可逆的。药物洗脱后5天的细胞存活率建立了有丝分裂阻滞可逆性和长期细胞存活之间的关系。U937、Jurkat、HL-60和HeLa细胞也出现了类似的结果,排除了细胞类型特异性作用。对其他微管蛋白药物的研究表明,有丝分裂阻滞的可逆性是抗有丝分裂药物的一个可量化的、化合物特异性的特征。Bcl-2磷酸化模式与eribulin和ER-076349有丝分裂阻断可逆模式平行,表明持续的Bcl-2磷酸化导致eribulin不可逆阻断后长期细胞存活率丧失。药物摄取和洗脱/保留研究表明,[3H]eribulin在细胞内的积累水平低于[3H]ER-076349,但保留时间更长,水平更高。不可逆长春新碱和可逆长春花碱也有类似的发现,表明持续的细胞滞留是不可逆性的一个组成部分。我们的研究结果表明,eribulin的体内优势源于其诱导不可逆有丝分裂阻滞的能力,这似乎与持续的药物滞留和持续的Bcl-2磷酸化有关。更广泛地说,我们的研究结果表明,抗有丝分裂剂的化合物特异性可逆性特征有助于基于细胞的药效学和体内药代动力学之间的相互作用,从而定义了间歇给药条件下的抗肿瘤疗效[4]。 在患有骨肉瘤的小鼠中,甲磺酸艾日布林(1 mg/kg;每周一次静脉注射,持续两周)可减少原发肿瘤和肺转移瘤的生长[1]。低浓度时,甲磺酸艾日布林(1 mg/kg;静脉注射一次)可抑制循环肿瘤细胞 (CTC) 的出现 [1]。 在小鼠骨肉瘤转移模型中,按照标准时间表施用更高剂量的Eribulin抑制了肺转移和原发性肿瘤生长。频繁的低剂量艾里布林给药(每4天0.3mg/kg×4)有效地抑制了肺转移,但对原发性肿瘤的生长几乎没有影响。总的来说,我们的研究结果表明,eribulin可以减少骨肉瘤的肺转移。[1] Eribulin对小鼠模型肺转移的抑制作用 我们首先使用临床给药方案在小鼠模型中研究了Eribulin是否抑制骨肉瘤肺转移。根据包装说明书,在第1天和第8天以1.4mg/m2的剂量临床给药艾立布林。人类和小鼠的药代动力学数据显示,给小鼠服用1mg/kg艾立布林与人类服用1.4mg/m2艾立布林的药代学相似。因此,在骨肉瘤转移模型中,我们每7天×2次以1mg/kg的剂量给药艾立布林(图1A)。治疗组小鼠的体重明显低于对照组(图1B)。Eribulin治疗显著抑制了原发性肿瘤的生长(图1C)并诱导了肿瘤细胞的凋亡(图1D)。我们通过计算转移灶(图1E)并测量其在组织切片中的面积(图1F顶部)来评估肺转移。Eribulin明显减少了肺水肿。组织学图像显示,对照组大转移灶浸润肺实质。相比之下,治疗组正常肺泡结构内的小转移灶是孤立的(图1F底部)。为了确定艾里布林是否减少了CTC,收集了血液样本并培养形成菌落。与对照组相比,治疗组的菌落数显著减少(图1G)。这些结果表明,eribulin可减少骨肉瘤的原发性肿瘤生长和肺转移。 |
| 酶活实验 |
Eribulin与可溶性微管蛋白结合[2]
在室温(22°C)下,将磷酸纤维素纯化的微管蛋白(1.8μM)在PEM 50缓冲液(50 mM PIPES、1 mM EGTA和1 mM MgSO4,pH 6.9)和100μM GTP中与[3H]eribulin(0.1μM-70μM)一起孵育20分钟,然后将每个样品的100μL加入Zeba™微球脱盐柱中。在添加艾立布林后立即测量每个样品的比活性。按照制造商的说明,将柱在1500×g下离心2分钟。测定了微管蛋白流通中的蛋白质含量和放射性。背景放射性标记是通过在使用的艾里布林浓度下离心不含蛋白质的样品来评估的。背景放射性水平与艾里布林浓度相关,平均4.2%的起始艾里布林在没有蛋白质存在的情况下通过柱。从所有实验放射性测量值中减去该值。 通过测量不同艾里布林浓度和单一固定浓度的微管蛋白(2μM)下与艾里布林结合的微管蛋白分数来量化平衡结合数据。以下简单双曲绑定模型与数据相吻合: YD=Ymax D/(Kd+D) 在该模型中,D是艾里布林的总浓度,YD和Ymax分别是亚饱和和无限浓度D下结合的艾里布林与微管蛋白的比率,Kd是平衡结合常数。使用KaleidaGraph®3.5通过非线性回归确定Ymax和Kd的最佳拟合值。使用所有数据点作为单个数据集计算艾里布林与可溶性微管蛋白结合的Ymax和Kd值以及标准误差。 微管解聚[2] 使用温度控制的Beckman Coulter分光光度计通过浊度测量微管解聚。通过在PEM 100缓冲液(100 mM PIPES、1 mM EGTA和1 mM MgSO4,pH 6.9)和1 mM GTP中在30°C下孵育30分钟,引发富含MAP的微管蛋白(3 mg/ml)的聚合。然后通过25号针将微管剪切八次,并让其在15分钟内恢复稳定状态。将微管悬浮液(100μL)的等分试样加入试管中,并放置在30°C的加热分光光度计中。在时间零点加入Eribulin(1μM-20μM),在每分钟350 nm的波长下读取吸光度读数30分钟。 微管负端的动态不稳定性[2] 如前所述,测量了艾里布林存在下微管的动态不稳定性。简而言之,微管(18μM微管蛋白)由磷酸纤维素纯化的微管蛋白在PMEM缓冲液(86 mM PIPES、26 mM MES、1 mM EGTA和1.4 mM MgSO4,pH 6.8)和1 mM GTP中组装而成,存在或不存在艾里布林。使用海胆鞭毛轴突丝片段使微管成核,并在35°C下孵育30分钟以达到稳定状态。使用IX71奥林巴斯倒置显微镜通过视频增强微分干涉对比显微镜记录单个微管的行为,并分析其生长和缩短事件。如前所述,负端与正端是不同的。每种情况下测量了45到50次生长和缩短事件。 Eribulin与微管的结合和微管长度的测定[2] 如上所述,从富含MAP的微管蛋白(3mg/ml)组装微管并剪切以获得大量短微管,然后再孵育20分钟以恢复稳定状态。将[3H]厄立布林(0.1μM-10μM)加入375μL剪切的微管中,并将样品立即分层到微管稳定垫上(PEM缓冲液中的30%甘油和10%DMSO),以尽量减少高浓度厄立布林下的解聚(与药物的孵育时间约为1-2分钟)。使用Beckman Coulter Optima超离心机(108000×g,60分钟,30°C)在SW 50.1摆动斗式转子中离心收集微管。丢弃可溶性部分,用PEM缓冲液仔细洗涤微管颗粒,并在4°C下将其溶解在0.1 N NaOH中过夜。第二天测量了颗粒的蛋白质含量和放射性。背景放射性标记是通过使用20μM鬼臼毒素抑制微管聚合进行平行测定来测量的。所有结果均减去背景。 微管长度通过电子显微镜测定,用于测定艾里布林与微管结合的化学计量比。每个实验测量至少300个微管的长度。对于对照组,每个实验的平均微管长度在2.4至4.2μm之间,总体平均值约为3μm。用0.2%戊二醛固定微管,将其放置在电子显微镜网格上,用细胞色素c(1mg/mL)和1%醋酸铀酰染色,并使用JEOL 1230透射电子显微镜(80 kV)成像,其中对照组不含eribulin,或在如下所述的eribulin温育后。 为了在化学计量测定中解释艾里布林诱导的微管长度变化,将微管与规定的艾里布林浓度一起孵育1-2分钟,并通过DMSO/甘油稳定垫离心至更致密的70%蔗糖层。如上所述固定和染色颗粒微管,并通过电子显微镜测量其长度。在5和10μM的浓度下,艾里布林分别使微管的平均长度缩短了17%和29%。在计算这两种浓度下每微管结合的艾里布林时,考虑了这些长度变化。 使用每个颗粒的质量和放射性、微管长度的平均测量值和每μm 1690个微管蛋白异二聚体的因子计算每个微管结合的艾里布林分子的数量。使用该样品的微管颗粒质量计算每个样品的每升微管数。使用KaleidaGraph®3.5使用上述方程计算结合数据的非线性回归。针对单个实验计算了艾里布林与微管结合的Ymax(每个微管结合的艾里布林分子的比率)和Kd值,并确定了所有实验的平均值和标准误差。 长春花碱对Eribulin与微管结合的影响[2] 在加入[3H]艾里布林之前,将未标记的长春花碱以2μM或4μM的浓度添加到剪切的富含MAP的微管中15分钟,然后如上所述处理样品。用于长度测量的电子显微镜样品是在长春花碱孵育后,但在艾立布林之前采集的。与之前的研究结果一致,即长春碱可以稳定微管末端,防止缩短,在长春碱(2或4μM)存在的情况下,艾里布林没有诱导微管长度的显著变化;因此,使用在每个实验中测量的长春碱处理的微管长度来计算长春碱存在下每个微管结合的艾里布林的化学计量比。 微管末端的形态[2] 为了确定药物对微管末端的影响,将未切除的微管与无药物、50μM艾瑞布林或50μM长春花碱一起孵育15分钟,然后将5μL样品轻轻加入电子显微镜网格上的15μL戊二醛(终浓度0.1%)中,并如上所述染色。对50个微管的两端进行了检查,每个微管用于对照和艾里布林处理的微管,30个微管用于长春花碱处理的微管。 |
| 细胞实验 |
细胞增殖测定[1]
细胞类型: LM8 细胞和 Dunn 细胞 测试浓度: 0、1、10、100 nM 孵育持续时间:72小时 实验结果:以剂量依赖性方式抑制细胞增殖。 细胞凋亡分析 [1] 细胞类型: LM8 细胞 测试浓度: 0、10、50 nM 孵育时间:12、24、48、72 小时 实验结果:50 nM 浓度在 12 小时后诱导早期细胞凋亡。在 10 nM 浓度下未检测到细胞凋亡。 细胞周期分析[1] 细胞类型: LM8 细胞 测试浓度: 0、10、50 nM 孵育持续时间:12、24、48、72 小时 实验结果:用 50 nM 处理 12 小时诱导G2/M 逮捕。 10 nM 处理不会诱导 G2/M 停滞。 细胞增殖试验[1] 根据制造商的说明,用CCK-8 WST检测试剂盒评估细胞存活率。简而言之,将LM8细胞以每孔1×104个细胞的密度铺在96孔板中,在含有10%FBS的DMEM中孵育24小时。然后,用不同浓度的Eribulin处理细胞72小时。然后将CCK-8试剂加入培养基中,在37°C下进一步孵育2小时。在450nm处用平板读数器测量吸光度。 流式细胞术分析[1] 将细胞以每孔3×105个细胞的浓度铺在24孔板上,生长24小时。然后用指定的Eribulin浓度处理细胞指定的时间段。它们用膜联蛋白-V和7-氨基放线菌素D(7-AAD)染色以鉴定凋亡,并用碘化丙啶染色以进行细胞周期分析。在Guava EasyCyte Plus流式细胞仪系统中分析样品。 免疫荧光[1] LM8细胞(1×103)在涂有纤维连接蛋白(10μg/mL)的8孔培养玻片上生长,孵育24小时。然后用Eribulin处理细胞16小时。用4%多聚甲醛固定20分钟,用0.1%Triton X-100(APC和p-FAK染色)或0.1%吐温20(α-微管蛋白染色)渗透10分钟,然后在室温下用0.1%牛血清白蛋白(BSA)和0.1%吐温20封闭60分钟。对于长春花素染色,在固定之前,用冰冷的渗透缓冲液(pH 6.9;10 mM HEPES,50 mM NaCl,3 mM MgCl2,0.5%Triton X-100,300 mM蔗糖和1 mM EGTA)在4°C下渗透细胞1分钟。细胞在4°C下用一抗(α-微管蛋白1:500;p-FAK 1:250;APC 1:250;长春花素1:50)染色过夜,然后进行二抗染色,并在室温下用Hoechst 33342复染30分钟。对于F-actin染色,根据制造商的说明,将细胞与罗丹明鬼笔环肽一起孵育。 突出测量[1] 将LM8细胞以每孔1×103个细胞的速度铺在8孔培养玻片上,生长24小时。用Eribulin处理细胞并孵育16小时。长度>20μm的微球被定义为突起。对来自三个生物复制品的150多个细胞进行了分析。 迁移分析[1] 如前所述,进行了改良的Boyden室迁移和伤口愈合试验。简而言之,在24孔Bio-Coat细胞迁移室中进行了12小时的改良Boyden室迁移试验。膜的下表面涂有30μg/mL的纤维连接蛋白,用于触觉迁移。LM8细胞以1×104个细胞的比例应用于上腔,用棉签从上表面去除非迁移性细胞。将迁移的细胞固定在70%v/v甲醇中,用结晶紫染色并计数。对于伤口愈合试验,将融合的LM8细胞刮伤,用磷酸缓冲盐水(PBS)彻底清洗,以去除分离的细胞和碎片。然后用Eribulin处理12小时。用斐济/ImageJ测量伤口图像。通过在伤口愈合过程中在室温下用100%冰冷的甲醇固定细胞10分钟,然后用含有1%BSA和0.1%吐温20的PBS封闭细胞30分钟来评估细胞方向性。MTOC在4°C下用抗周蛋白抗体(1:1000)染色过夜。然后将细胞与抗兔IgG和赫斯特在室温下孵育30分钟。对来自三个独立实验的100多个细胞进行了分析。 三维胶原蛋白培养[1] 通过将3.8mg/mL酸溶性大鼠尾胶原在DMEM中稀释至1.5mg/mL,并用1mol/L NaOH中和至pH 7.4,制备胶原凝胶。将细胞悬浮液以200个细胞/孔的密度加入孔中,然后立即转移到37°C的培养箱中30分钟以引发聚合。然后用含有Eribulin的培养基覆盖胶原凝胶。在第1、4和6天在显微镜下观察细胞或集落。使用Fiji/ImageJ软件分析了入侵媒介的长度和菌落大小。菌落形成率计算为第4天每施加一个细胞数的菌落数。 细胞增殖和有丝分裂指数[3] 将细胞接种在聚-L-赖氨酸处理过的无菌玻璃盖玻片上(50mg/ml,2小时,37°C,用无菌水洗涤一次),以1×105个细胞/2 ml/孔的速度接种在六孔板中。一天后,用含有不同浓度(0.003-10000 nmol/L)的Eribulin或ER-076349的新鲜培养基替换培养基,并进一步培养一个细胞周期(28小时)。通过将漂浮细胞与附着细胞结合来收获细胞,附着细胞是通过胰蛋白酶化(0.5 mg/ml的PBS溶液:137 mmol/L NaCl,2.7 mmol/L KCl,1.5 mmol/L KH2PO4,8.1 mmol/L Na2HPO4,0.5 mmol/L EDTA,pH 7.2)(5分钟,37°C)释放的,并使用血细胞计数器计数活细胞。台盼蓝染料用于区分活细胞和死细胞。为了评估有丝分裂指数,细胞在药物存在和不存在的情况下生长20小时。有丝分裂指数是通过显微镜检查福尔马林/甲醇(如下所述)固定的细胞中的染色体和GFP-CENP-B着丝粒来确定的,用4,6-二脒基-2-苯基吲哚(DAPI)染色,并使用尼康Eclipse E800显微镜进行成像,该显微镜具有60倍和100倍的物镜(两者的数值孔径均为1.4)。结果是5个独立实验的平均值和标准误差,其中每个实验中每个条件下至少计数1000个细胞。IC50是通过增殖或有丝分裂指数与药物浓度的双倒数图的线性回归来确定的。 细胞摄取和洗脱/保留研究[4] U-937细胞中[3H]Eribulin、[3H]ER-076349、[3H]长春新碱和[3H]长春花碱的摄取和清除/保留评估如下。将氚化化合物加入到无菌的1.5 mL螺旋盖微量离心管中,并风干以去除溶剂。在100μL细胞培养基中重新悬浮化合物后,将22.2×106个细胞加入0.9 mL完全培养基(包括胎牛血清、谷氨酰胺和抗生素)中。孵化温度为37°C,经常涡旋。60分钟后,根据经验确定了达到最大放射性吸收所需的最小时间,即化合物吸收与药物浓度的函数关系。细胞相关放射性测定如下。取三份25-μL细胞样品,分层放置在400μL Sarstedt管中300μL冰冷的20%蔗糖上,然后以8500×g离心1分钟,将细胞与标记培养基分离,并在离心通过蔗糖的过程中洗涤细胞。带有颗粒细胞的试管立即在干冰/乙醇浴中冷冻。立即将含有颗粒的仍然冷冻的试管底部直接切入闪烁瓶中,然后加入闪烁液和放射性计数(Beckman LS 6000计数器)。由于配对药物之间细胞摄取的差异出乎意料地大(图6),不同的预加载浓度用于洗脱/保留研究,以相等的细胞内药物水平开始(虚线,图6A和B)。因此,洗脱/保留研究的预加载浓度使用了800 nmol/L[3H]艾里布林和100 nmol/L[4H]ER-076349,以及600 nmol/L ~3H]长春新碱和190 nmol/L的[3H]长春碱。 |
| 动物实验 |
Animal/Disease Models: C3H/HeN mice (4 weeks old) were injected with LM8 cells [1]
Doses: 1 mg/kg Route of Administration: intravenous (iv) (iv)injection once a week for 2 weeks Experimental Results: Inhibited primary tumor growth and induced tumor cell apoptosis Death. Reduce lung metastasis. Lost weight. Four-week-old C3H/HeN mice were used. LM8 cells metastasize to the lungs by both subcutaneous and intraosseous transplantation. Researchers chose subcutaneous transplantation because of its high reproductivity of the metastatic process, such as CTC appearance and lung metastasis formation, compared to intraosseous transplantation. For the Eribulin metastasis reduction experiments, LM8 cells (5 × 106 per mouse) were injected into the subcutaneous tissue of the backs of syngeneic mice. The animals were randomized into control and treatment groups. Eribulin was injected into the tail veins at 1 mg/kg every 7 days × 2 or 0.3 mg/kg every 4 days × 4. Histological evaluations and pulmonary metastasis foci counts were performed four weeks after tumor cell injection because tumor-bearing mice die from lung metastasis around 5 weeks after subcutaneous transplantation. Lungs were fixed with 10% formalin, embedded in paraffin, cut into 8-μm sections, and stained with hematoxylin and eosin (H&E). Apoptosis in the primary tumors was assessed by a TUNEL assay of the paraffin sections using an In Situ Cell Death Detection Kit according to the manufacturer's instructions. For CTC quantification, Eribulin was injected into the tail veins at a rate of 1 mg/kg two weeks after LM8 transplantation as mentioned above. Peripheral blood samples (40 μL) were collected from the tail veins and maintained in DMEM supplemented with 10% FBS and penicillin (100 U/mL)-streptomycin (100 μg/mL) to form colonies as previously described. Colonies were fixed with 10% formalin, stained with crystal violet, and counted. [1] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Eribulin is eliminated primarily in feces unchanged. 43 L/m2 to 114 L/m2 1.16 L/hr/m2 to 2.42 L/hr/m2 (dose range of 0.25 mg/m2 to 4.0 mg/m2). [FDA] Metabolism / Metabolites There are no major human metabolites of eribulin, CYP3A4 negligibly metabolizes eribulin in vitro. Biological Half-Life about 40 hours Eribulin (eribulin mesylate) is a synthetic analog of halichondrin B, a natural product derived from the marine sponge Halichondria okadai. It is a microtubule dynamics inhibitor used in the treatment of metastatic breast cancer and liposarcoma. Below is a summary of its pharmacokinetic (PK) characteristics based on available data: Absorption Eribulin is administered intravenously (IV) over 2–5 minutes, ensuring complete bioavailability. Distribution It has a large volume of distribution (~43–114 L/m²), indicating extensive tissue distribution. Plasma protein binding is moderate, ranging from 49% to 65%. Metabolism Eribulin undergoes limited hepatic metabolism, primarily via CYP3A4 to a minor extent, but most of the drug is eliminated unchanged. It is not a significant substrate, inhibitor, or inducer of major CYP enzymes, reducing the risk of drug-drug interactions. Elimination The elimination half-life is approximately 40 hours, allowing for a dosing schedule of Day 1 and Day 8 of a 21-day cycle. Excretion occurs mainly via the feces (82%), with a smaller portion (9%) excreted unchanged in the urine. Special Populations Hepatic impairment: Patients with mild (Child-Pugh A) or moderate (Child-Pugh B) liver dysfunction require dose reductions due to increased exposure. Severe impairment (Child-Pugh C) has not been studied. Renal impairment: Moderate renal impairment (CrCl 30–50 mL/min) also necessitates dose adjustment, while severe renal impairment (CrCl <30 mL/min) has limited data. Key Considerations Eribulin’s PK is not significantly affected by age, body weight, or race. Due to its long half-life, accumulation can occur with repeated dosing, necessitating monitoring for toxicity (e.g., neutropenia, peripheral neuropathy). These PK properties support its clinical use in advanced cancers, with adjustments needed for hepatic or renal dysfunction to minimize toxicity. For more details, refer to prescribing information or clinical studies. |
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
Eribulin is a cytotoxic chemotherapeutic agent and serum aminotransferase and alkaline phosphatase elevations are common during cyclic therapy of breast cancer and liposarcoma. The reported rates of ALT elevations have ranged from 8% to 83% with values above 5 times the upper limit or normal (ULN) in 2% to 5%. Isolated mention of “toxic hepatitis” have been made in reports of clinical trials of eribulin but no details of the onset, clinical features and course have been published and the role of eribulin in these outcomes is uncertain. Nevertheless, despite high rates of serum enzyme elevations during treatment, cases of clinically apparent liver injury have not been reported in detail and must be rare. Likelihood score: E* (unproven but suspected cause of liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation No information is available on the clinical use of eribulin during breastfeeding. The manufacturer recommends that breastfeeding be discontinued during eribulin therapy and for 2 weeks after the last dose. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding 49 to 65%. Eribulin (eribulin mesylate) is a microtubule inhibitor used in the treatment of metastatic breast cancer and liposarcoma. While effective, it is associated with several toxicities, primarily affecting the hematologic, neurological, and gastrointestinal systems. Below is a summary of its key toxicities: 1. Hematologic Toxicity Neutropenia: The most common and dose-limiting toxicity, occurring in ≥25% of patients. Severe (Grade 3/4) neutropenia has been reported in up to 57% of cases, increasing the risk of infections. Anemia: Frequently observed (≥25%), with some cases requiring transfusion support. Thrombocytopenia: Less common but can lead to bleeding complications in severe cases. 2. Neurological Toxicity Peripheral Neuropathy: A frequent adverse event (≥25%), manifesting as numbness, tingling, or pain in the extremities. It can be dose-dependent and sometimes irreversible. Fatigue: Reported in a significant proportion of patients, impacting quality of life. 3. Gastrointestinal Toxicity Nausea & Vomiting: Common (≥25%) but generally manageable with antiemetics. Constipation: Frequently reported, sometimes requiring medical intervention. 4. Other Toxicities Alopecia: Hair loss is common but typically reversible after treatment cessation. Cardiac Effects: Rare cases of QT prolongation and arrhythmias have been reported, requiring monitoring in high-risk patients. Hepatotoxicity: Elevated liver enzymes may occur, particularly in patients with pre-existing liver impairment. Management Recommendations Dose Adjustments: Required for severe neutropenia, neuropathy, or hepatic/renal impairment. Prophylactic Measures: Growth factor support (e.g., G-CSF) may be needed for neutropenia, and dose delays are advised for unresolved toxicities. Eribulin’s toxicity profile necessitates careful patient monitoring, particularly in those with pre-existing conditions. Dose modifications and supportive care are essential to mitigate adverse effects while maintaining therapeutic efficacy. For detailed guidelines, refer to prescribing information. |
| 参考文献 |
|
| 其他信息 |
Eribulin is a fully synthetic macrocyclic ketone analogue of marine sponge natural products. Inhibits growth phase of microtubules via tubulin-based antimitotic mechanism, which leads to G2/M cell-cycle block, disruption of mitotic spindles, and, ultimately, apoptotic cell death after prolonged mitotic blockage It has a role as an antineoplastic agent and a microtubule-destabilising agent. It is a macrocycle, a polyether, a polycyclic ether, a cyclic ketone, a primary amino compound and a cyclic ketal. It is a conjugate base of an eribulin(1+).
Eribulin is a microtubule inhibitor indicated for the treatment of patients with metastatic breast cancer who have previously received at least two chemotherapeutic regimens for the treatment of metastatic disease. Eribulin was isolated from the marine sponge Halichondria okadai. Eribulin is also being investigated for use in the treatment of advanced solid tumors. Eribulin is a Microtubule Inhibitor. The physiologic effect of eribulin is by means of Microtubule Inhibition. Eribulin mesylate is an inhibitor of microtubule function and is used as an antineoplastic agent for refractory, metastatic breast cancer and liposarcoma. Despite its cytotoxic activity against cancer cells, eribulin has rarely been implicated in causing clinically apparent acute liver injury. Eribulin is an analogue of halichondrin B, a substance derived from a marine sponge (Lissodendoryx sp.) with antineoplastic activity. Eribulin binds to the vinca domain of tubulin and inhibits the polymerization of tubulin and the assembly of microtubules, resulting in inhibition of mitotic spindle assembly, induction of cell cycle arrest at G2/M phase, and, potentially, tumor regression. See also: Eribulin Mesylate (has salt form). Drug Indication For the treatment of patients with metastatic breast cancer who have previously received at least two chemotherapeutic regimens for the treatment of metastatic cancer. FDA Label Halaven monotherapy is indicated for the treatment of patients with locally advanced or metastatic breast cancer who have progressed after at least one chemotherapeutic regimens for advanced disease (see section 5. 1). Prior therapy should have included an anthracycline and a taxane unless patients were not suitable for these treatments. Halaven is indicated for the treatment of adult patients with unresectable liposarcoma who have received prior anthracycline containing therapy (unless unsuitable) for advanced or metastatic disease (see section 5. 1). Treatment of soft tissue sarcoma Mechanism of Action Eribulin inhibits the growth phase of microtubules without affecting the shortening phase and sequesters tubulin into nonproductive aggregates. Eribulin exerts its effects via a tubulin-based antimitotic mechanism leading to G2/M cell-cycle block, disruption of mitotic spindles, and, ultimately, apoptotic cell death after prolonged mitotic blockage. [FDA] Pharmacodynamics Linear Eribulin mesylate is a methanesulfonate salt obtained by reaction of eribulin with one equivalent of methanesulfonic acid. A fully synthetic macrocyclic ketone analogue of marine sponge natural products. Inhibits growth phase of microtubules via tubulin-based antimitotic mechanism, which leads to G2/M cell-cycle block, disruption of mitotic spindles, and, ultimately, apoptotic cell death after prolonged mitotic blockage. It has a role as an antineoplastic agent and a microtubule-destabilising agent. It contains an eribulin(1+). Eribulin Mesylate is the mesylate salt of a synthetic analogue of halichondrin B, a substance derived from a marine sponge (Lissodendoryx sp.) with antineoplastic activity. Eribulin binds to the vinca domain of tubulin and inhibits the polymerization of tubulin and the assembly of microtubules, resulting in inhibition of mitotic spindle assembly, induction of cell cycle arrest at G2/M phase, and, potentially, tumor regression. See also: Eribulin (has active moiety). ERIBULIN MESYLATE is a small molecule drug with a maximum clinical trial phase of IV (across all indications) that was first approved in 2010 and has 4 approved and 18 investigational indications. Our study has several limitations. We used C3H mice for our syngeneic metastasis model, however, the pharmacokinetics data we referred to in this study were measured using different strains (BALB/c and CF-1). We assume that the pharmacokinetics of eribulin in C3H mice is similar to that in other strains as most eribulin is excreted into the bile and urine without being metabolized after intravenous injection. Sampson et al. reported that some osteosarcoma cell lines regrew in the presence of eribulin, but remained sensitive to eribulin [42]. We did not examine the delayed growth of LM8 cells at metastatic sites. It is possible that lung metastasis of LM8 proliferate later during long-term administration of eribulin, therefore, we need to examine a combination strategy with other chemotherapeutic agents. Collectively, eribulin is a potential therapeutic option for lung metastasis of osteosarcoma. Its anti-metastatic effects at concentrations lower than IC50 suggest that it has a wide application range. Frequent low-dose eribulin administration can reduce lung metastasis for a long time with relatively few side effects.[1] By electron microscopy, we showed that eribulin at high concentration (50 μM) did not induce extensive protofilament spiraling at microtubule ends as occurs with vinblastine (Fig. 5). The ends of the microtubules were blunt or slightly splayed (Table 2). This finding supports the model that eribulin binds β-tubulin with high affinity and α-tubulin with low or no affinity, and thus eribulin does not “link” tubulin heterodimers together in the manner of vinblastine, which binds both subunits nearly equally. However, the presence of the slightly splayed microtubule ends suggests a possible low affinity binding to α-tubulin. Since 22% of eribulin-treated microtubules showed slight splaying at both ends, therefore it appears that at sufficiently high concentrations, eribulin may bind minus ends. Vinblastine inhibited eribulin binding to microtubules at low eribulin concentrations (≤ 5 μM), (Fig. 4A and B). Unexpectedly, vinblastine induced an increase in the number of eribulin binding sites per microtubule at higher eribulin concentrations, increasing from 11 to 14 and to 17 eribulin molecules per microtubule in the presence of 2 μM and 4 μM vinblastine, respectively (Fig. 4A). This slight increase in binding suggests that the vinblastine-induced splaying of protofilaments allows increased access of eribulin to additional sites at the microtubule end. [2] Eribulin is chemically distinct from the microtubule-targeted drugs paclitaxel and Vinca alkaloids, it binds differently to microtubules than paclitaxel, and it suppresses microtubule dynamics in a distinct manner from paclitaxel and Vinca alkaloids. However, at concentrations that induce mitotic arrest, all of these drugs suppress centromere dynamics. These results provide strong support for the idea that suppression of spindle microtubule dynamics by these drugs and the resulting disruption of tension on the chromosome kinetochores/centromeres is the primary mechanism responsible for their abilities to induce mitotic arrest. [3] In summary, our results point to eribulin's ability to induce irreversible mitotic blockade as a cell-based pharmacodynamic explanation for its superior in vivo efficacy relative to the more potent ER-076349. Eribulin's irreversible mitotic blockade leads to persistent inactivation of Bcl-2, leading to apoptosis and complete long-term loss of cell viability. Eribulin's irreversible mitotic blockade is associated with lower cellular drug uptake yet more persistent postwashout retention compared with ER-076349, although the precise mechanisms behind this remain unclear. Preferential binding of eribulin to small numbers of high affinity sites at microtubule ends may explain its persistent postwashout retention, although further studies are needed to confirm this. Regardless of mechanism, correlations between eribulin's irreversibility and long-term postwashout cell-viability loss provide a satisfying explanation for its in vivo superiority over ER-076349 in preclinical tumor models using intermittent dosing. In ongoing clinical trials, eribulin is administered using intermittent dosing. Its ability to induce irreversible mitotic blockade in cancer cells may thus have important pharmacodynamic implications for its clinical activity as well, in which fluctuations in circulating drug levels associated with intermittent dosing routinely occur. [4] |
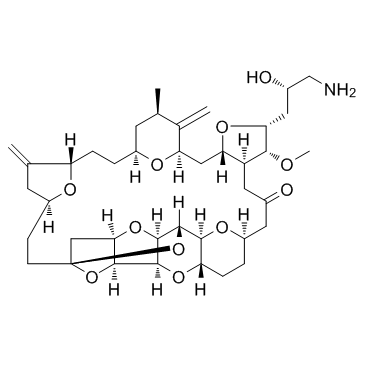
| 分子式 |
C₄₀H₅₉NO₁₁
|
|---|---|
| 分子量 |
729.90
|
| 精确质量 |
729.408
|
| 元素分析 |
C, 65.82; H, 8.15; N, 1.92; O, 24.11
|
| CAS号 |
253128-41-5
|
| 相关CAS号 |
Eribulin mesylate;441045-17-6
|
| PubChem CID |
11354606
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
1.29±0.1 g/cm3
|
| 折射率 |
1.584
|
| LogP |
3.88
|
| tPSA |
146.39
|
| 氢键供体(HBD)数目 |
2
|
| 氢键受体(HBA)数目 |
12
|
| 可旋转键数目(RBC) |
4
|
| 重原子数目 |
52
|
| 分子复杂度/Complexity |
1380
|
| 定义原子立体中心数目 |
19
|
| SMILES |
C[C@@H]1C[C@@H]2CC[C@H]3C(=C)C[C@@H](O3)CC[C@]45C[C@@H]6[C@H](O4)[C@H]7[C@@H](O6)[C@@H](O5)[C@@H]8[C@@H](O7)CC[C@@H](O8)CC(=O)C[C@H]9[C@H](C[C@H](C1=C)O2)O[C@@H]([C@@H]9OC)C[C@@H](CN)O
|
| InChi Key |
UFNVPOGXISZXJD-JBQZKEIOSA-N
|
| InChi Code |
InChI=1S/C40H59NO11/c1-19-11-24-5-7-28-20(2)12-26(45-28)9-10-40-17-33-36(51-40)37-38(50-33)39(52-40)35-29(49-37)8-6-25(47-35)13-22(42)14-27-31(16-30(46-24)21(19)3)48-32(34(27)44-4)15-23(43)18-41/h19,23-39,43H,2-3,5-18,41H2,1,4H3/t19-,23+,24+,25-,26+,27+,28+,29+,30-,31+,32-,33-,34-,35+,36+,37+,38-,39+,40+/m1/s1
|
| 化学名 |
(1S,3S,6S,9S,12S,14R,16R,18S,20R,21R,22S,26R,29S,31R,32S,33R,35R,36S)-20-[(2S)-3-amino-2-hydroxypropyl]-21-methoxy-14-methyl-8,15-dimethylidene-2,19,30,34,37,39,40,41-octaoxanonacyclo[24.9.2.13,32.13,33.16,9.112,16.018,22.029,36.031,35]hentetracontan-24-one
|
| 别名 |
B1939; E7389; ER086526; Eribulin; 253128-41-5; Eribulin [INN]; eribuline; Eribulina; UNII-LR24G6354G; CHEBI:63587; LR24G6354G; B 1939; E 7389; ER 086526; B-1939; E-7389; ER-086526
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中(例如氮气保护),避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ~200 mg/mL (~274.01 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 5 mg/mL (6.85 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 50.0 mg/mL澄清DMSO储备液加入400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 5 mg/mL (6.85 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 50.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 5 mg/mL (6.85 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.3701 mL | 6.8503 mL | 13.7005 mL | |
| 5 mM | 0.2740 mL | 1.3701 mL | 2.7401 mL | |
| 10 mM | 0.1370 mL | 0.6850 mL | 1.3701 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
A Phase-3, Open-Label, Randomized Study of Dato-DXd Versus Investigator's Choice of Chemotherapy (ICC) in Participants With Inoperable or Metastatic HR-Positive, HER2-Negative Breast Cancer Who Have Been Treated With One or Two Prior Lines of Systemic Chemotherapy (TROPION-Breast01)
CTID: NCT05104866
Phase: Phase 3 Status: Active, not recruiting
Date: 2024-11-21