| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| Other Sizes |
|
| 体内研究 (In Vivo) |
在应激大鼠中,艾司西酞普兰(10 mg/kg;腹腔注射;每天给药,持续 28 天)可减轻认知障碍,并特别减少磷酸化 tau 蛋白的积累 [3]。每天服用 2.5 mg 和 5 mg 剂量的艾司西酞普兰,每天服用总共 4 个月,斑块负荷分别显着降低 28% 和 34% [4]。
|
|---|---|
| 动物实验 |
Animal/Disease Models: Male SD (SD (Sprague-Dawley)) rat [3]
Doses: 10 mg/kg Route of Administration: intraperitoneal (ip) injection; one time/day for 28 days. Experimental Results: It can selectively reduce the accumulation of phosphorylated tau protein in the hippocampus of stressed rats. And it can Dramatically relieve depression and resist the overactivity of the HPA axis in rats. Animal/Disease Models: APP-PS1 hemizygous female mice (4 months old) [4] Doses: 2.5-5 mg/kg Route of Administration: daily; drinking water for a total of 4 months Experimental Results: compared with littermates who only drank water Compared to mice, mice at both doses had Dramatically diminished plaque burden in their brains. ESC 2.5 mg/day and 5 mg/day Dramatically diminished hippocampal plaque burden by 28.7% and 34.4%, respectively. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Absorption of escitalopram following oral administration is expected to be almost complete, with an estimated absolute bioavailability of approximately 80%. Tmax occurs after about 4-5 hours. Cmax and AUC appear to follow dose proportionality - at steady state, patients receiving 10mg of escitalopram daily had a Cmax of 21 ng/mL and a 24h AUC of approximately 360 ng*h/mL, while patients receiving 30mg daily had a roughly 3-fold increase in both Cmax and 24h AUC, comparatively. After oral administration of escitalopram, approximately 8% of the total dose is eliminated in the urine as unchanged escitalopram and 10% is eliminated in the urine as S-desmethylcitalopram. The apparent hepatic clearance of escitalopram amounts to approximately 90% of the total dose. Escitalopram appears to distribute extensively into tissues, with an apparent volume of distribution of approximately 12-26 L/kg. The oral plasma clearance of escitalopram is 600 mL/min, of which approximately 7% is due to renal clearance. /MILK/ Escitalopram is excreted in human breast milk. Limited data from women taking 10-20 mg escitalopram showed that exclusively breast-fed infants receive approximately 3.9% of the maternal weight-adjusted dose of escitalopram and 1.7% of the maternal weight-adjusted dose of desmethylcitalopram. The absolute bioavailability of citalopram is about 80% relative to an intravenous dose, and the volume of distribution of citalopram is about 12 L/kg. Data specific on escitalopram are unavailable. The binding of escitalopram to human plasma proteins is approximately 56%. Following a single oral dose (20 mg tablet or solution) of escitalopram, peak blood levels occur at about 5 hours. Absorption of escitalopram is not affected by food. Metabolism / Metabolites The metabolism of escitalopram is mainly hepatic, mediated primarily by CYP2C19 and CYP3A4 and, to a lesser extent, CYP2D6. Oxidative N-demethylation by the CYP enzyme system results in S-desmethylcitalopram (S-DCT) and S-didesmethylcitalopram (S-DDCT) - these metabolites do not contribute to the pharmacologic activity of escitalopram, and exist in the plasma in small quantities relative to the parent compound (28-31% and <5%, respectively). There is also some evidence that escitalopram is metabolized to a propionic acid metabolite by monoamine oxidase A and B in the brain, and that these enzymes constitute the major route of escitalopram metabolism in the brain. The antidepressant escitalopram is predominantly metabolized by the polymorphic CYP2C19 enzyme. The authors investigated the effect of CYP2C19 genotype on exposure and therapeutic failure of escitalopram in a large patient population. A total of 4,228 escitalopram serum concentration measurements from 2,087 CYP2C19-genotyped patients 10-30 hours after drug intake were collected retrospectively from the drug monitoring database at Diakonhjemmet Hospital in Oslo. The patients were divided into subgroups based on CYP2C19 genotype: those carrying inactive (CYP2C19Null) and gain-of-function (CYP2C19*17) variant alleles. The between-subgroup differences in escitalopram exposure (endpoint: dose-harmonized serum concentration) and therapeutic failure (endpoint: switching to another antidepressant within 1 year after the last escitalopram measurement) were evaluated by multivariate mixed model and chi-square analysis, respectively. Compared with the CYP2C19*1/*1 group, escitalopram serum concentrations were significantly increased 3.3-fold in the CYP2C19Null/Null group, 1.6-fold in the CYP2C19*Null/*1 group, and 1.4-fold in the CYP2C19Null/*17 group, whereas escitalopram serum concentrations were significantly decreased by 10% in the CYP2C19*1/*17 group and 20% in the CYP1C19*17/*17 group. In comparison to the CYP2C19*1/*1 group, switches from escitalopram to another antidepressant within 1 year were 3.3, 1.6, and 3.0 times more frequent among the CYP2C19Null/Null, CYP2C19*1/*17, and CYP1C19*17/*17 groups, respectively. The CYP2C19 genotype had a substantial impact on exposure and therapeutic failure of escitalopram, as measured by switching of antidepressant therapy. The results support the potential clinical utility of CYP2C19 genotyping for individualization of escitalopram therapy. Escitalopram is metabolized to S-demethylcitalopram (S-DCT) and S-didemethylcitalopram (S-DDCT). In humans, unchanged escitalopram is the predominant compound in plasma. At steady state, the concentration of the escitalopram metabolite S-DCT in plasma is approximately one-third that of escitalopram. The level of S-DDCT was not detectable in most subjects. In vitro studies show that escitalopram is at least 7 and 27 times more potent than S-DCT and S-DDCT, respectively, in the inhibition of serotonin reuptake, suggesting that the metabolites of escitalopram do not contribute significantly to the antidepressant actions of escitalopram. S-DCT and S-DDCT also have no or very low affinity for serotonergic (5-HT1-7) or other receptors including alpha- and beta-adrenergic, dopamine (D1-5), histamine (H1-3), muscarinic (M1-5), and benzodiazepine receptors. S-DCT and S-DDCT also do not bind to various ion channels including Na+, K+, Cl-, and Ca++ channels. In vitro studies using human liver microsomes indicated that CYP3A4 and CYP2C19 are the primary isozymes involved in the Ndemethylation of escitalopram. Mainly hepatic. Escitalopram undergoes N-demethylation to S-demethylcitalopram (S-DCT) and S-didemethylcitalopram (S-DDCT). CYP3A4 and CYP2C19 are the enzymes responsible for this N-demethylation reaction. Route of Elimination: Following oral administrations of escitalopram, the fraction of drug recovered in the urine as escitalopram and S-demethylcitalopram (S-DCT) is about 8% and 10%, respectively. The oral clearance of escitalopram is 600 mL/min, with approximately 7% of that due to renal clearance. Escitalopram is metabolized to S-DCT and S-didemethylcitalopram (S-DDCT). Half Life: 27-32 hours Biological Half-Life The elimination half-life of escitalopram is 27-32 hours, though this is increased by approximately 50% in the elderly and doubled in patients with reduced hepatic function. The elimination half-life of escitalopram's primary metabolite, S-desmethylcitalopram, is approximately 54 hours at steady state. Biotransformation of escitalopram is mainly hepatic, with a mean terminal half-life of about 27-32 hours. |
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation Escitalopram is the active S-isomer of the antidepressant, citalopram. Limited information indicates that maternal doses of escitalopram up to 20 mg daily produce low levels in milk and would not be expected to cause any adverse effects in breastfed infants, especially if the infant is older than 2 months. If escitalopram is required by the mother, it is not a reason to discontinue breastfeeding. A safety scoring system finds escitalopram use to be possible during breastfeeding. One case of necrotizing enterocolitis was reported in a breastfed newborn whose mother was taking escitalopram during pregnancy and lactation, but causality was not established. A seizure-like event occurred in an infant who was also exposed to bupropion in milk. Other minor behavioral problems have also been reported. Monitor the infant for excess drowsiness, restlessness, agitation, poor feeding and poor weight gain, especially in younger, exclusively breastfed infants and when using combinations of psychotropic drugs. Mothers taking a selective serotonin reuptake inhibitor (SSRI) like escitalopram during pregnancy and postpartum may have more difficulty breastfeeding, although this might be a reflection of their disease state. These mothers may need additional breastfeeding support. Infants exposed to an SSRI during the third trimester of pregnancy have a lower risk of poor neonatal adaptation if they are breastfed than formula-fed infants. ◉ Effects in Breastfed Infants Eight breastfed infants whose mothers were taking escitalopram in an average dose of 199 mcg/kg daily for postpartum depression were evaluated by a pediatric specialist using the Denver developmental scale. Their mothers had taken escitalopram for a median of 55 days postpartum (range 23 to 240 days). The infants' scores on this scale was 110% of normal. A woman began taking escitalopram 5 mg daily immediately after birth. Her dosage was increased to 10 mg daily and valproic acid 1200 mg daily was added by 7 weeks postpartum. Her breastfed infant was judged to be healthy and have normal neuropsychological development by a general practitioner at 7.5 weeks of age. One woman was taking escitalopram 20 mg daily and reboxetine 4 mg daily orally while nursing her infant (extent not stated). She had taken reboxetine for 1.5 months, but the start of her escitalopram therapy was not stated. At 9.5 months of age, her breastfed infant had normal weight gain and a Denver developmental score of 105% of chronological age. A nursing mother was given escitalopram 10 mg daily for depression beginning at 3 weeks postpartum and increasing to 20 mg daily thereafter. At 4 months of age, her exclusively breastfed infant was admitted to the hospital for irritability, vomiting and fever of 4 days duration. He had been irritable with prolonged periods of crying for the past 3 months according to his mother and had gained only 400 grams per month since birth. Liver enzymes were moderately elevated. The infant was discharged after 5 days and breastfeeding was continued, but only twice daily for 2 weeks, then discontinued at 4.5 months of age. At 5 months, symptom improvement was noted and at 6 months, serum liver enzymes had normalized. The author noted that the time course of the adverse effects were consistent with the treatment with escitalopram. A mother began taking escitalopram 20 mg daily in the morning on day 15 postpartum. She exclusively breastfed her infant on demand. At 3 months of age, no adverse effects had been reported in the infant by his pediatrician. At 5 days of age, an infant was readmitted to the neonatal intensive care unit with a diagnosis of necrotizing enterocolitis. The infant had spent the first 2 days of life in intensive care because of respiratory distress. The infant's mother had taken escitalopram 20 mg daily throughout pregnancy and while breastfeeding (extent not stated). The authors hypothesized that escitalopram might have been responsible for the enterocolitis because of its effect on platelet aggregation. The drug was possibly a cause of the reaction. One author reported on the newborn infant of a mother who was taking escitalopram (dose and duration not stated). The hyperirritable infant had high-pitched crying 2 hours after breastfeeding every afternoon which was 5 to 6 hours after maternal dose of escitalopram. Changing the time of the mother's escitalopram dose resulted in a shift in the time of the infant's crying at the same time interval after the dose. The infant's symptoms improved with partial substitution of formula and ceased on day 11 of life with complete formula feeding. An uncontrolled online survey compiled data on 930 mothers who nursed their infants while taking an antidepressant. Infant drug discontinuation symptoms (e.g., irritability, low body temperature, uncontrollable crying, eating and sleeping disorders) were reported in about 10% of infants. Mothers who took antidepressants only during breastfeeding were much less likely to notice symptoms of drug discontinuation in their infants than those who took the drug in pregnancy and lactation. A 6.5-month-old infant developed severe vomiting and an apparent tonic seizure after being breastfed by her mother. The mother had been taking escitalopram 10 mg daily since birth and had begun extended-release bupropion 150 mg daily 3 weeks earlier. The seizure occurred 8 hours after the mother's morning dose of bupropion. The infant's mother had noted disturbances in sleep behavior, unusual movements, and unresponsiveness followed by sleep on several previous occasions. The baby was partially breastfed, also receiving pumped breastmilk, formula, and solid foods. Breastfeeding was discontinued and the baby was discharged after being asymptomatic for 48 hours. The seizure was probably drug-related, most likely caused by bupropion and hydroxybupropion in breastmilk, but a contribution by escitalopram cannot be ruled out. A cohort of 247 infants exposed to an antidepressant in utero during the third trimester of pregnancy were assessed for poor neonatal adaptation (PNA). Of the 247 infants, 154 developed PNA. Infants who were exclusively given formula had about 3 times the risk of developing PNA as those who were exclusively or partially breastfed. None of the infants were exposed to escitalopram in utero, but 51 were exposed to citalopram, the racemic form of the drug. A case-control study in Israel compared 280 infants of nursing mothers taking long-term psychotropic drugs to the infants of 152 women taking antibiotics. Infant sleepiness at 3 days of age was reported by 3 mothers taking escitalopram during pregnancy and breastfeeding and by none taking antibiotics. The sleepiness resolved within 24 hours with no developmental effect. A mother with mixed anxiety-depressive order was taking sertraline and breastfeeding her 9-month-old infant. Because of side effects, sertraline was stopped and citalopram 10 daily was started. After 2 weeks of therapy, she reported signs of bruxism in her infant who was breastfed 5 to 6 times daily, as well as supplementary feedings such as fruits, vegetables, meat, and biscuits. The infant had sporadic, pulsatile, and momentary movements in her jaws, which usually began with movements of the head, especially during sleep. Furthermore, the mother mentioned her child had a habit of biting and clenching her teeth while awake. Pediatric and dental examinations found no abnormalities, but the dentist observed bruxism during the examination. Citalopram was discontinued and bruxism symptoms resolved after 72 hours. The mother resumed breastfeeding with no return of symptoms and the infant had no bruxism symptoms for the next 2 years. Bruxism was probably caused by citalopram in breastmilk. ◉ Effects on Lactation and Breastmilk The SSRI class of drugs, including escitalopram, can cause increased prolactin levels and galactorrhea in nonpregnant, nonnursing patients. Euprolactinemic galactorrhea has also been reported. The prolactin level in a mother with established lactation may not affect her ability to breastfeed. In a small prospective study, 8 primiparous women who were taking a serotonin reuptake inhibitor (SRI; 3 taking fluoxetine and 1 each taking citalopram, duloxetine, escitalopram, paroxetine or sertraline) were compared to 423 mothers who were not taking an SRI. Mothers taking an SRI had an onset of milk secretory activation (lactogenesis II) that was delayed by an average of 16.7 hours compared to controls (85.8 hours postpartum in the SRI-treated mothers and 69.1 h in the untreated mothers), which doubled the risk of delayed feeding behavior in the untreated group. However, the delay in lactogenesis II may not be clinically important, since there was no statistically significant difference between the groups in the percentage of mothers experiencing feeding difficulties after day 4 postpartum. A case control study compared the rate of predominant breastfeeding at 2 weeks postpartum in mothers who took an SSRI antidepressant throughout pregnancy and at delivery (n = 167) or an SSRI during pregnancy only (n = 117) to a control group of mothers who took no antidepressants (n = 182). Among the two groups who had taken an SSRI, 33 took citalopram, 18 took escitalopram, 63 took fluoxetine, 2 took fluvoxamine, 78 took paroxetine, and 87 took sertraline. Among the women who took an SSRI, the breastfeeding rate at 2 weeks postpartum was 27% to 33% lower than mother who did not take antidepressants, with no statistical difference in breastfeeding rates between the SSRI-exposed groups. An observational study looked at outcomes of 2859 women who took an antidepressant during the 2 years prior to pregnancy. Compared to women who did not take an antidepressant during pregnancy, mothers who took an antidepressant during all 3 trimesters of pregnancy were 37% less likely to be breastfeeding upon hospital discharge. Mothers who took an antidepressant only during the third trimester were 75% less likely to be breastfeeding at discharge. Those who took an antidepressant only during the first and second trimesters did not have a reduced likelihood of breastfeeding at discharge. The antidepressants used by the mothers were not specified. A retrospective cohort study of hospital electronic medical records from 2001 to 2008 compared women who had been dispensed an antidepressant during late gestation (n = 575) to those who had a psychiatric illness but did not receive an antidepressant (n = 1552) and mothers who did not have a psychiatric diagnosis (n = 30,535). Women who received an antidepressant were 37% less likely to be breastfeeding at discharge than women without a psychiatric diagnosis, but no less likely to be breastfeeding than untreated mothers with a psychiatric diagnosis. None of the mothers were taking escitalopram. In a study of 80,882 Norwegian mother-infant pairs from 1999 to 2008, new postpartum antidepressant use was reported by 392 women and 201 reported that they continued antidepressants from pregnancy. Compared with the unexposed comparison group, late pregnancy antidepressant use was associated with a 7% reduced likelihood of breastfeeding initiation, but with no effect on breastfeeding duration or exclusivity. Compared with the unexposed comparison group, new or restarted antidepressant use was associated with a 63% reduced likelihood of predominant, and a 51% reduced likelihood of any breastfeeding at 6 months, as well as a 2.6-fold increased risk of abrupt breastfeeding discontinuation. Specific antidepressants were not mentioned. Protein Binding Escitalopram exhibits relatively low protein binding at approximately 55-56%. |
| 参考文献 |
|
| 其他信息 |
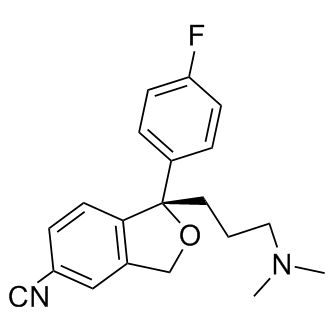
Escitalopram is a 1-[3-(dimethylamino)propyl]-1-(4-fluorophenyl)-1,3-dihydro-2-benzofuran-5-carbonitrile that has S-configuration at the chiral centre. It is the active enantiomer of citalopram. It has a role as an antidepressant and an EC 3.4.21.26 (prolyl oligopeptidase) inhibitor. It is a conjugate base of an escitalopram(1+). It is an enantiomer of a (R)-citalopram.
Escitalopram is a selective serotonin re-uptake inhibitor (SSRI) and the S-enantiomer of racemic [citalopram]. It is used to restore serotonergic function in the treatment of depression and anxiety. Escitalopram is approximately 150 times more potent than citalopram’s R-enantiomer and is responsible for the vast majority of citalopram’s clinical activity, with some evidence suggesting that the R-enantiomer of racemic citalopram actively dampens the activity of escitalopram rather than existing simply as an inactive enantiomer. Amongst SSRIs, escitalopram exerts the highest degree of selectivity for the serotonin transporter (SERT) relative to other off-targets which may explain its lower rates of adverse effects as compared to other agents in this class. Escitalopram also differentiates itself from other SSRIs via allosteric action on its target - this may be the mechanism responsible for its observed superior efficacy and faster onset compared to other SSRIs. Escitalopram is a Serotonin Reuptake Inhibitor. The mechanism of action of escitalopram is as a Serotonin Uptake Inhibitor. Escitalopram is the active S-stereoisomer of the selective serotonin reuptake inhibitor (SSRI) citalopram with antidepressant, anti-obsessive-compulsive and antibulimic properties. Escitalopram inhibits the reuptake of the neurotransmitter serotonin (5-HT) at the serotonin reuptake pump of the neuronal membrane of the presynaptic cell, thereby increasing levels of 5-HT within the synaptic cleft and enhancing the actions of serotonin on 5HT1A autoreceptors. Unlike other SSRIs, escitalopram appears to not only bind to a primary high-affinity site on the serotonin transporter protein but also to a secondary lower-affinity allosteric site that is considered to stabilize and prolong drug binding. Escitalopram, the S-enantiomer of citalopram, belongs to a class of antidepressant agents known as selective serotonin-reuptake inhibitors (SSRIs). Despite distinct structural differences between compounds in this class, SSRIs possess similar pharmacological activity. As with other antidepressant agents, several weeks of therapy may be required before a clinical effect is seen. SSRIs are potent inhibitors of neuronal serotonin reuptake. They have little to no effect on norepinephrine or dopamine reuptake and do not antagonize α- or β-adrenergic, dopamine D2 or histamine H1 receptors. During acute use, SSRIs block serotonin reuptake and increase serotonin stimulation of somatodendritic 5-HT1A and terminal autoreceptors. Chronic use leads to desensitization of somatodendritic 5-HT1A and terminal autoreceptors. The overall clinical effect of increased mood and decreased anxiety is thought to be due to adaptive changes in neuronal function that leads to enhanced serotonergic neurotransmission. Side effects include dry mouth, nausea, dizziness, drowsiness, sexual dysfunction and headache. Side effects generally occur within the first two weeks of therapy and are usually less severe and frequent than those observed with tricyclic antidepressants. Escitalopram may be used to treat major depressive disorder (MDD) and generalized anxiety disorder (GAD). Escitalopram is a furancarbonitrile that is one of the Serotonin uptake inhibitors used as an antidepressant. The drug is also effective in reducing ethanol uptake in alcoholics and is used in depressed patients who also suffer from tardive dyskinesia in preference to tricyclic antidepressants, which aggravate this condition; Escitalopram (Cipralex) is a medication developed by the Danish pharmaceutical company Lundbeck, that acts as a selective serotonin reuptake inhibitor (SSRI). It is typically used as an antidepressant to treat depression associated with mood disorders, although it also may be used in the treatment of body dysmorphic disorder and anxiety, including OCD. In the United States, the drug is marketed under the name Lexapro by Forest Laboratories, Inc; Escitalopram is a medication that acts as a selective serotonin reuptake inhibitor (SSRI). It is typically used as an antidepressant to treat depression associated with mood disorders, although it also may be used in the treatment of body dysmorphic disorder and anxiety, including OCD; Discontinuation from antidepressants, especially abruptly, has been known to cause certain withdrawal symptoms. One possible discontinuation symptom from Escitalopram is a type of spontaneous nerve pulse known as paresthesia or 'electric shock sensations', described by some patients as a feeling of small electric shocks, which may be accompanied by dizziness. These pulses may be short in duration, only milliseconds long, may affect any region of the body, and recur up to several times a minute, throughout all waking hours. They can be increased by physical activity, but are not solely linked to muscular activity. Other discontinuation symptoms include extreme sensitivity to loud sounds and bright lights, chills, hot flushes, cold sweats, reddening of the face, abdominal pain, weight gain and extreme mental fatigue. S-enantiomer of CITALOPRAM. Belongs to a class of drugs known as SELECTIVE SEROTONIN REUPTAKE INHIBITORS, used to treat depression and generalized anxiety disorder. See also: Escitalopram Oxalate (has salt form); Citalopram (annotation moved to). Drug Indication Escitalopram is indicated for the acute and maintenance treatment of major depressive disorder (MDD) in adults and pediatric patients 12 years old and older and for the acute treatment of generalized anxiety disorder (GAD) in adults and pediatric patients 7 years old and older. It is additionally indicated for symptomatic relief of obsessive-compulsive disorder (OCD) in Canada. Mechanism of Action Escitalopram, like other selective serotonin re-uptake inhibitors, enhances serotonergic activity by binding to the orthosteric (i.e. primary) binding site on the serotonin transporter (SERT), the same site to which endogenous 5-HT binds, and thus prevents the re-uptake of serotonin into the presynaptic neuron. Escitalopram, along with [paroxetine], is also considered an allosteric serotonin re-uptake inhibitor - it binds to a secondary allosteric site on the SERT molecule to more strongly inhibit 5-HT re-uptake. Its combination of orthosteric and allosteric activity on SERT allows for greater extracellular 5-HT levels, a faster onset of action, and greater efficacy as compared to other SSRIs. The sustained elevation of synaptic 5-HT eventually causes desensitization of 5-HT1A auto-receptors, which normally shut down endogenous 5-HT release in the presence of excess 5-HT - this desensitization may be necessary for the full clinical effect of SSRIs and may be responsible for their typically prolonged onset of action. Escitalopram has shown little-to-no binding affinity at a number of other receptors, such as histamine and muscarinic receptors, and minor activity at these off-targets may explain some of its adverse effects. The mechanism of antidepressant action of escitalopram, the S-enantiomer of racemic citalopram, is presumed to be linked to potentiation of serotonergic activity in the central nervous system (CNS) resulting from its inhibition of CNS neuronal reuptake of serotonin (5-HT). |
| 分子式 |
C19H18FN2O
|
|---|---|
| 分子量 |
309.36
|
| 精确质量 |
309.14
|
| CAS号 |
128196-01-0
|
| 相关CAS号 |
Escitalopram oxalate;219861-08-2
|
| PubChem CID |
146570
|
| 外观&性状 |
Colorless to light yellow ointment
|
| 密度 |
1.2±0.1 g/cm3
|
| 沸点 |
428.3±45.0 °C at 760 mmHg
|
| 熔点 |
147-152C
|
| 闪点 |
212.8±28.7 °C
|
| 蒸汽压 |
0.0±1.0 mmHg at 25°C
|
| 折射率 |
1.591
|
| LogP |
2.51
|
| tPSA |
110.86
|
| 氢键供体(HBD)数目 |
0
|
| 氢键受体(HBA)数目 |
4
|
| 可旋转键数目(RBC) |
5
|
| 重原子数目 |
24
|
| 分子复杂度/Complexity |
466
|
| 定义原子立体中心数目 |
1
|
| SMILES |
FC1=CC=C([C@@]2(CCCN(C)C)C(C=CC(C#N)=C3)=C3CO2)C=C1
|
| InChi Key |
WSEQXVZVJXJVFP-FQEVSTJZSA-N
|
| InChi Code |
InChI=1S/C20H21FN2O/c1-23(2)11-3-10-20(17-5-7-18(21)8-6-17)19-9-4-15(13-22)12-16(19)14-24-20/h4-9,12H,3,10-11,14H2,1-2H3/t20-/m0/s1
|
| 化学名 |
(1S)-1-[3-(dimethylamino)propyl]-1-(4-fluorophenyl)-3H-2-benzofuran-5-carbonitrile
|
| 别名 |
Seroplex Escitalopram
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ~100 mg/mL (~308.27 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (7.71 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (7.71 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (7.71 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 3.2325 mL | 16.1624 mL | 32.3248 mL | |
| 5 mM | 0.6465 mL | 3.2325 mL | 6.4650 mL | |
| 10 mM | 0.3232 mL | 1.6162 mL | 3.2325 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。