| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 1g |
|
||
| Other Sizes |
|
| 靶点 |
NLRP3
NOD-like receptor family pyrin domain-containing 3 (NLRP3) inflammasome (IC₅₀ = 7.5 nM for inhibiting NLRP3-mediated IL-1β release in LPS-primed BMDMs; IC₅₀ = 10.1 nM for inhibiting NLRP3 ATPase activity); no significant activity against NLRC4 (IC₅₀ > 10 μM) or AIM2 (IC₅₀ > 10 μM) inflammasomes [1] |
|---|---|
| 体外研究 (In Vitro) |
在纳摩尔剂量下,MCC950 可防止传统和非规范的 NLRP3 激活。 MCC950 不会特异性抑制 AIM2、NLRC4 和 NLRP1 的激活,而 NLRP3 则会被抑制。使用小鼠骨髓源性巨噬细胞 (BMDM) 和人单核细胞源性巨噬细胞 (HMDM),研究了 MCC950 对 NLRP3 炎性体激活的影响。 MCC950 在 BMDM 中表现出约 7.5 nM 的抑制能力,在 HMDM 中表现出约 8.1 nM 的抑制能力。此外,MCC950 以剂量依赖性方式减少 IL-1β 分泌,但不减少 TNF-α 分泌。 MCC950 首先刺激非经典途径,然后选择性抑制 caspase-11 介导的 NLRP3 激活和 IL-1β 释放。即使剂量为 10 µM,MCC950 也无法抑制鼠伤寒沙门氏菌诱导的 NLRC4 刺激的 IL-1β 和 TNF-α 产生。 MCC950 对鼠伤寒沙门氏菌响应的 IL-1β 或 caspase-1 激活过程没有影响。 MCC950 处理不会对细胞裂解物中的 pro-caspase-1 和 pro-IL-1β 产生显着影响 [1]。
在LPS预处理的小鼠骨髓来源巨噬细胞(BMDMs)中:MCC950以剂量依赖性方式抑制多种刺激物(ATP、尼日利亚菌素、尿酸单钠结晶、明矾)诱导的NLRP3炎症小体激活,IL-1β释放的IC₅₀ = 7.5 nM,IL-18释放的IC₅₀ = 8.2 nM。蛋白质印迹分析显示caspase-1(p10亚基)和gasdermin D(GSDMD)的切割减少,证实炎症小体依赖性焦亡被抑制[1] - 在人外周血单个核细胞(PBMCs)和THP-1来源巨噬细胞中:MCC950(1–100 nM)抑制尼日利亚菌素或尿酸结晶诱导的NLRP3介导IL-1β释放,PBMCs中IC₅₀ = 9.3 nM,THP-1细胞中IC₅₀ = 8.7 nM,且不影响TNF-α或IL-6的产生(LPS诱导的TLR4信号通路)[1] - NLRP3 ATP酶活性抑制:MCC950在体外直接抑制重组NLRP3 NACHT结构域的ATP酶活性,IC₅₀ = 10.1 nM,不影响NLRC4或NAIP5的ATP酶活性[1] - 选择性:浓度高达10 μM时,MCC950不抑制NLRC4(鞭毛蛋白诱导)或AIM2(poly(dA:dT)诱导)炎症小体激活,也不影响TLR2/4/9或RIG-I样受体信号通路[1] - ASC斑点形成抑制:免疫荧光染色显示,MCC950(10 nM)使LPS预处理、ATP刺激的BMDMs中ASC斑点(炎症小体组装标志物)数量较溶媒对照组减少89%[1] |
| 体内研究 (In Vivo) |
MCC950 可减轻实验性自身免疫性脑脊髓炎 (EAE)(一种多发性硬化症疾病模型)的严重程度,并减少白介素-1p (IL-1β) 的产生。 MCC950 预处理可降低 IL-1β 和 IL-6 的血清浓度,但不会显着降低 TNF-α 水平。 MCC950 治疗可减轻小鼠 EAE 的严重程度并推迟其发展。将 MCC950 处理的动物与 PBS 处理的小鼠进行比较时,第 22 天处死小鼠的脑单核细胞的细胞内细胞因子标记和 FACS 分析显示,产生 IL-17 和 IFN-γ 的 CD3+ T 细胞的频率略低。产生 IFN-γ 的 CD3+ T 细胞的 CD4+ 和 γδ+ 亚群数量减少,特别是产生 IL-17 的细胞[1]。
小鼠腹膜炎模型(尿酸结晶或明矾诱导):刺激前1小时腹腔注射MCC950(1、3、10 mg/kg),剂量依赖性降低腹腔IL-1β水平(尿酸结晶组分别降低45%、68%、82%;明矾组分别降低42%、65%、80%)和中性粒细胞浸润(尿酸结晶组降低38%、59%、75%)[1] - 小鼠痛风模型(关节内注射尿酸结晶):结晶注射前1小时或后4小时腹腔注射MCC950(3 mg/kg),显著减轻关节肿胀(分别减少63%和51%)、爪温升高(分别减少58%和49%)及滑膜IL-1β水平(分别减少72%和65%)[1] - 小鼠实验性自身免疫性脑脊髓炎(EAE,多发性硬化症模型):免疫后第0天至第21天每日口服MCC950(10 mg/kg),降低EAE临床评分(平均峰值评分1.2 vs 溶媒组3.8),减少脊髓CD4+ T细胞和巨噬细胞浸润(分别减少60%和55%),减轻脱髓鞘(减少70%)及中枢神经系统IL-1β/IL-18水平[1] - ApoE-/-小鼠动脉粥样硬化模型:每日口服MCC950(10 mg/kg),持续12周,减少主动脉动脉粥样硬化病变面积(减少48%),降低病变部位巨噬细胞聚集(减少52%),降低血浆IL-1β水平(减少65%),且不影响胆固醇水平[1] - db/db小鼠2型糖尿病模型:每日口服MCC950(10 mg/kg),持续8周,改善葡萄糖耐量(AUC减少32%),提高胰岛素敏感性(HOMA-IR减少40%),减轻胰岛炎症(IL-1β+细胞减少68%)[1] |
| 酶活实验 |
炎症小体活化测定[1]
将BMDM以5×0 105/ml或1×0 6/ml接种,HMDM以5倍10 5/ml接种,PBMC以2×10 6/ml或5×0 6 g/ml接种于96孔板中。第二天,更换过夜培养基,并用来自大肠杆菌血清型EH100(ra)TLRgrade™的10 ng/ml LPS刺激细胞3小时。取出培养基,用含有二甲基亚砜(1:1000)、MCC950(0.001-10µM)、格列本脲(200µM),孤雌内酯(10µM)或拜耳半胱氨酰白三烯受体拮抗剂1-(5-羧基-2{3-[4-(3-环己基丙氧基)苯基]丙氧基}苯甲酰基)哌啶-4-羧酸(40µM)的无血清培养基(SFM)代替。然后用炎症小体激活剂刺激细胞30分钟:5 mM腺苷5’-三磷酸二钠盐水合物(ATP)(1小时)、用Lipofectamine 2000™(Invitrogen)转染的1µg/ml聚脱氧腺苷酸胸苷酸钠盐(Poly dA:dT)(3-4小时)、200µg/ml MSU(过夜)和10µM尼格瑞金(1小时。细胞也用25µg/ml聚腺苷酸-多ridylic acid刺激(4小时)。对于非典型炎症小体激活细胞,用100 ng/ml Pam3CSK4引发4小时,移除培养基并用含有DMSO或MCC950的SFM代替,并使用0.25%FuGENE®转染2µg/ml LPS 16小时。根据制造商的说明,移除上清液并使用ELISA试剂盒分析。使用Cytox96®非放射性细胞毒性测定法测量LDH释放。[1] 飞行时间炎症小体评估(TOFIE)测定[1] 使用Lipofectamine 2000™在24孔板中用以下质粒转染HEK293T细胞(4×105/ml):pEF6人ASC-GFP、pEF6人类C-mCherry或空载体对照。转染后1小时,用DMSO或MCC950(0.1–50µM)处理细胞。将转染后15小时的细胞移除并悬浮在含有1%FCS和2mM EDTA的DPBS中。使用Gallios™流式细胞仪和FlowJo软件对细胞进行分析。在GFP和Cherry表达上对活细胞进行门控(当共转染时)。通过分析GFP脉冲区域的高度和宽度(低宽度:区域和高高度:区域)来确定含有ASC斑点的细胞的百分比。Sester et al。 NLRP3 ATP酶活性检测:将重组人NLRP3 NACHT结构域在检测缓冲液(三羟甲基氨基甲烷-盐酸、氯化镁、二硫苏糖醇)中稀释至2 μM。将系列稀释(0.001–100 nM)的MCC950与NACHT结构域混合,37°C孵育30分钟后加入1 mM ATP启动反应,继续孵育60分钟。采用比色法测量无机磷(Pi)生成量,在620 nm处检测吸光度,通过剂量-反应曲线的非线性回归计算IC₅₀值[1] - NLRC4/NAIP5 ATP酶活性检测:按NLRP3的制备方法制备重组NLRC4或NAIP5蛋白,MCC950测试浓度最高达10 μM,测量ATP酶活性以评估选择性[1] |
| 细胞实验 |
蛋白质印迹[1]
通过在50µl 5中直接裂解制备细胞裂解物ィ 莱姆利样品缓冲液。根据制造商的说明,使用StrataClean™树脂浓缩上清液的蛋白质含量。将蛋白质样品在15%SDS-PAGE凝胶上解析,并使用湿转移系统转移到聚偏二氟乙烯(PVDF)膜上。在室温(RT)下,将膜封闭在TBS-T(50mM Tris/HCL,pH 7.6,150mM NaCl和0.1%(v/v)Tween-20)中的5%(w/v)奶粉中1小时。将膜与稀释在TBS-T中的5%(w/v)奶粉中的一级抗体一起孵育,然后与适当的辣根过氧化物酶(HRP)偶联的二级抗体在TBS-T中稀释在5%(w/v)奶粉中孵育1小时。使用20ィ LumiGLO®化学发光试剂。在重新处理之前,使用Restore™PLUS蛋白质印迹剥离缓冲液剥离膜。[1] 将患有CAPS的个体的PBMC以2×0 106/ml的剂量接种在12孔板中,然后用1µg/ml LPS预处理3小时。用含有MCC950(5–1000 nM)的SFM代替培养基。45分钟后,收集细胞培养上清液和细胞裂解物。使用Novex®Tris-Glycine凝胶系统解析样品。[1] 荧光成像平板阅读器(FLIPR)Ca2+分析[1] 将BMDM(3×104/孔)在37°C下用不洗涤的钙染料(Molecular Devices)在含有0.1%BSA的生理盐水溶液(PSS;成分NaCl 140 mM,葡萄糖11.5 mM,KCl 5.9 mM,MgCl2 1.4 mM,NaH2PO4 1.2 mM,NaHCO3 5 mM,CaCl2 1.8 mM,HEPES 10 mM)中加载30分钟。然后将细胞转移到FLIPRETTRA荧光板读取器上,并使用冷却的CCD相机测量Ca2+响应,激发为470–495 nM,发射为515–575 nM。调节每个板的相机增益和强度,以产生至少1000个任意荧光单位(AFU)的基线荧光。在添加MCC950之前,采集10个基线荧光读数,然后在添加样品后300秒内每秒读取荧光读数,并在添加PSS或ATP(500µM)后再读取300秒。 BMDM NLRP3炎症小体激活检测:小鼠骨髓细胞在培养基中分化为巨噬细胞,持续7天。将BMDMs以1×10⁶个细胞/孔接种到24孔板,用LPS(100 ng/mL)预处理3小时。MCC950(0.001–100 nM)在ATP(5 mM)、尼日利亚菌素(10 μM)、尿酸结晶(200 μg/mL)或明矾(200 μg/mL)刺激前1小时加入。刺激后6小时收集上清液,通过ELISA检测IL-1β/IL-18水平;裂解细胞进行蛋白质印迹分析,检测caspase-1、GSDMD及β-肌动蛋白(内参)[1] - ASC斑点形成检测:将LPS预处理的BMDMs接种到盖玻片上,用MCC950(10 nM)处理1小时后,用ATP(5 mM)刺激1小时。细胞经多聚甲醛固定、曲拉通X-100透化后,用抗ASC抗体和DAPI染色。共聚焦显微镜下计数ASC斑点,斑点定义为离散的点状ASC信号[1] - 人PBMC检测:分离人PBMCs,以5×10⁵个细胞/孔接种到24孔板,用LPS(100 ng/mL)预处理3小时,MCC950(0.01–100 nM)处理1小时后,用尼日利亚菌素(10 μM)刺激6小时。收集上清液,通过ELISA检测IL-1β、TNF-α和IL-6水平[1] |
| 动物实验 |
In vivo LPS challenge[1]
C57BL/6 mice were injected intraperitoneally (i.p.) with 50 mg/kg MCC950 or vehicle control (DMSO/PBS) 1 h h before i.p. injection of 10 mg/kg LPS Escherichia coli 055:B5 or PBS. After for 2 h mice were sacrificed and serum levels of IL-1β, TNF-α and IL-6 were measured by ELISA.[1] Induction and Assessment of EAE[1] C57BL/6 mice were immunized subcutaneously with 150 µg of MOG peptide 35–55 (GenScript) emulsified in CFA containing 4 mg/ml (0.4.mg/mouse) of heat-killed MTB (Chondrex). Mice were injected i.p. with 500 ng pertussis toxin (PT: kaketsuken) on days 0 and 2. MCC950 was administered i.p. to mice (10 mg/kg) at induction of the disease, day 0, 1 and 2 and every 2 days thereafter. Control mice were administered vehicle (PBS) at the same time points. Mice were observed for clinical signs of disease daily (unblinded). Disease severity was scored as follows: no clinical signs, 0; limp tail, 1; ataxic gait, 2; hind limb weakness, 3; hind limb paralysis, 4; and tetra paralysis, 5., Experiments were performed under license (BI00/2412) from The Irish Medicine Board and with approval from the Trinity College Dublin BioResources Ethics Committee.[1] FACS analysis of EAE[1] On day 22 post immunization mononuclear cells were isolated from whole brains of perfused mice with EAE, following homogenisation and centrifugation on a Percoll gradient. Mononuclear cells (MNC) (2 × 106/ml) were stimulated for 4 h with PMA (10 ng/ml) and ionomycin (1 µg/ml) in the presence of brefeldin A (5 µg/ml). Cells were washed in PBS and re-suspended in 50 µL PBS with 1:1,000 LIVE/DEAD® Fixable Aqua Dead Cell Stain kit for 20 min. Surface stains for CD3 (145-2c11) (0.5 µl/106 cells), CD4 (RM4-5) (0.5 µl/106 cells) and γδ TCR (GL3) (1 µl/106 cells) (eBioscience) were added and cells were incubated for a further 20 mins. Cells were then fixed with 2% paraformaldehyde and washed in PBS twice, before being intracellularly stained for IL-17 or IFN-γ in permeabilization buffer (0.2% saponin in PBS + 1% FBS). Flow cytometric analysis of MNC was performed using a BD LSRFortessa™ and analysed with FlowJo software. MNC were first gated on live CD3+ T cells followed by CD4 expression, γδ TCR expression or cytokine production.[1] NLRP3 and NLRP1 activating mutation mice[1] Mice were backcrossed to C57BL/6 at least ten times. Nlrp3A350VneoR mice were provided by Hal M. Hoffman, The University of California, San Diego, U.S.A. and crossed with LysMCre mice (B6.129P2-Lyz2tm1(cre)Ifo/J. MCC950 was administered i.p. (20 mg/kg) every second day starting at day 4 after birth. Mice with an activating mutation in NLRP1, Nlrp1aQ593P were generated on a C57BL/6 background as described previously and administered MCC950 i.p. (20 mg/kg) every second day for 9 days. Blood was collected at the timepoints indicated for analysis of plasma cytokines by ELISA. IL-18 ELISA was performed as described by Westwell-Roper et al. Experiments were performed under AEC Project 2013.011 and were approved by the Animal Ethics Committee of The Walter and Eliza Hall Institute of Medical Research. Peritonitis model: C57BL/6 mice (6–8 weeks old, n=6 per group) were administered MCC950 (1, 3, 10 mg/kg) or vehicle (0.5% methylcellulose) via intraperitoneal injection 1 hour before intraperitoneal injection of urate crystals (1 mg/mouse) or alum (2 mg/mouse). Six hours later, mice were euthanized, and peritoneal lavage fluid was collected to count neutrophils and measure IL-1β levels by ELISA [1] - Gout model: C57BL/6 mice (n=6 per group) received intra-articular injection of urate crystals (1 mg) into the right hind paw. MCC950 (3 mg/kg) or vehicle was administered intraperitoneally 1 hour before or 4 hours after crystal injection. Paw swelling was measured using a caliper, and paw temperature was recorded with an infrared thermometer. Mice were euthanized 24 hours post-crystal injection, and synovial tissue was collected for IL-1β measurement [1] - EAE model: C57BL/6 mice (n=8 per group) were immunized subcutaneously with MOG₃₅₋₅₅ peptide emulsified in complete Freund's adjuvant, plus intraperitoneal injection of pertussis toxin on day 0 and day 2. MCC950 (10 mg/kg) or vehicle was administered orally once daily from day 0 to day 21. Clinical EAE scores (0–5 scale) were assessed daily. On day 21, mice were euthanized, and spinal cords were collected for histopathological analysis (Luxol fast blue staining for demyelination) and flow cytometry (immune cell infiltration) [1] - Atherosclerosis model: ApoE-/- mice (8-week-old, n=7 per group) were fed a high-fat diet for 12 weeks. MCC950 (10 mg/kg) or vehicle was administered orally once daily during the diet period. At the end of the study, mice were euthanized, and the aorta was isolated to measure atherosclerotic lesion area by Oil Red O staining. Plasma cholesterol and IL-1β levels were measured [1] - Type 2 diabetes model: db/db mice (8-week-old, n=7 per group) were administered MCC950 (10 mg/kg) or vehicle orally once daily for 8 weeks. Glucose tolerance tests were performed at baseline and week 8, and insulin sensitivity was assessed by HOMA-IR. Pancreatic islets were isolated for immunohistochemical staining of IL-1β [1] |
| 药代性质 (ADME/PK) |
In C57BL/6 mice: Oral administration of MCC950 (10 mg/kg) resulted in peak plasma concentration (Cₘₐₓ) of 0.8 μg/mL, time to Cₘₐₓ (Tₘₐₓ) of 1.5 hours, terminal half-life (t₁/₂) of 3.8 hours, and oral bioavailability of 52% [1]
- Tissue distribution: After oral administration (10 mg/kg), MCC950 distributed to major organs (liver, spleen, kidney, lung) with tissue-to-plasma ratios of 2.3 (liver), 1.9 (spleen), 1.7 (kidney), 1.5 (lung), and 0.9 (brain) at 2 hours post-dosing [1] - In vitro metabolism: Human liver microsome studies showed MCC950 had moderate metabolic stability, with intrinsic clearance (CLint) of 35 μL/min/mg protein [1] |
| 毒性/毒理 (Toxicokinetics/TK) |
Acute toxicity: In C57BL/6 mice, oral LD₅₀ of MCC950 was >200 mg/kg, with no overt toxicity (convulsions, respiratory depression, weight loss) observed at doses up to 100 mg/kg [1]
- Subchronic toxicity: In a 12-week repeated oral dose study in ApoE-/- mice (10 mg/kg/day), MCC950 did not cause significant changes in body weight, food intake, hematological parameters (red blood cells, white blood cells, platelets), or liver/kidney function (ALT, AST, creatinine, BUN). No histopathological abnormalities were observed in major organs [1] - Plasma protein binding: MCC950 had a plasma protein binding rate of 91% in mouse plasma and 93% in human plasma, as measured by ultrafiltration [1] - Drug-drug interaction: In vitro studies showed no inhibition of cytochrome P450 enzymes (CYP1A2, CYP2C9, CYP2C19, CYP2D6, CYP3A4) at concentrations up to 10 μM [1] |
| 参考文献 | |
| 其他信息 |
The NOD-like receptor (NLR) family, pyrin domain-containing protein 3 (NLRP3) inflammasome is a component of the inflammatory process, and its aberrant activation is pathogenic in inherited disorders such as cryopyrin-associated periodic syndrome (CAPS) and complex diseases such as multiple sclerosis, type 2 diabetes, Alzheimer's disease and atherosclerosis. We describe the development of MCC950, a potent, selective, small-molecule inhibitor of NLRP3. MCC950 blocked canonical and noncanonical NLRP3 activation at nanomolar concentrations. MCC950 specifically inhibited activation of NLRP3 but not the AIM2, NLRC4 or NLRP1 inflammasomes. MCC950 reduced interleukin-1β (IL-1β) production in vivo and attenuated the severity of experimental autoimmune encephalomyelitis (EAE), a disease model of multiple sclerosis. Furthermore, MCC950 treatment rescued neonatal lethality in a mouse model of CAPS and was active in ex vivo samples from individuals with Muckle-Wells syndrome. MCC950 is thus a potential therapeutic for NLRP3-associated syndromes, including autoinflammatory and autoimmune diseases, and a tool for further study of the NLRP3 inflammasome in human health and disease.[1]
Diabetes is associated with a high risk of developing cognitive dysfunction and neuropsychiatric disabilities, and these disease symptomsare termed diabetic encephalopathy (DEP). Inflammation is involved in the development of DEP. The cleavage and maturation of the proinflammatory cytokine interleukin (IL)-1β is regulated by the NLRP3 inflammasome. Obese and type 2 diabetic db/db mice show anxiety- and depression-like behaviors and cognitive disorders associated with hippocampal inflammation. The purpose of this study was to explore the role of NLRP3 inflammasome in DEP. Results showed that expression levels of inflammasome components including NLRP3, apoptosis-associated speck-like protein (ASC), and caspase-1, as well as IL-1β in the hippocampus of diabetic db/db mice were higher than those of non-diabetic db/m mice. Treatment of db/db mice with NLRP3 inflammasome inhibitor MCC950 ameliorated anxiety- and depression-like behaviors as well as cognitive dysfunction, and reversed increased NLRP3, ASC, and IL-1βexpression levels and caspase-1 activity in hippocampus. Moreover, MCC950 treatment significantly improved insulin sensitivity in db/db mice. These results demonstrate that inhibition of NLRP3 inflammasome activation may prove to be a potential therapeutic approach for DEP treatment.[2] MCC950 is a potent, selective, orally active small-molecule inhibitor of the NLRP3 inflammasome, identified through high-throughput screening of chemical libraries [1] - Its core mechanism of action involves binding to the NACHT domain of NLRP3, inhibiting its ATPase activity, and preventing NLRP3 inflammasome assembly (ASC speck formation) and downstream activation of caspase-1, GSDMD cleavage, and release of IL-1β/IL-18 [1] - Preclinical data support its potential therapeutic utility in a broad range of NLRP3-driven inflammatory diseases, including gout, multiple sclerosis, atherosclerosis, and type 2 diabetes [1] - MCC950 exhibits high selectivity for NLRP3 over other inflammasomes (NLRC4, AIM2) and innate immune signaling pathways, minimizing off-target inflammatory suppression [1] - The favorable oral bioavailability, tissue distribution (including central nervous system penetration), and low toxicity of MCC950 make it a promising clinical candidate for inflammatory disease treatment [1] |
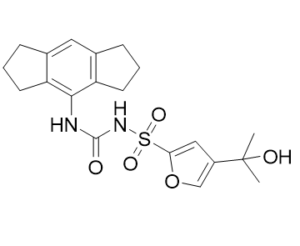
| 分子式 |
C20H24N2O5S
|
|
|---|---|---|
| 分子量 |
404.48
|
|
| 精确质量 |
404.14
|
|
| CAS号 |
210826-40-7
|
|
| 相关CAS号 |
MCC950 sodium;256373-96-3
|
|
| PubChem CID |
9910393
|
|
| 外观&性状 |
White to light yellow solid
|
|
| 密度 |
1.4±0.1 g/cm3
|
|
| 熔点 |
239 ºC
|
|
| 折射率 |
1.637
|
|
| LogP |
3.2
|
|
| tPSA |
106Ų
|
|
| 氢键供体(HBD)数目 |
3
|
|
| 氢键受体(HBA)数目 |
5
|
|
| 可旋转键数目(RBC) |
4
|
|
| 重原子数目 |
28
|
|
| 分子复杂度/Complexity |
684
|
|
| 定义原子立体中心数目 |
0
|
|
| SMILES |
S(C1=C([H])C(=C([H])O1)C(C([H])([H])[H])(C([H])([H])[H])O[H])(N([H])C(N([H])C1=C2C([H])([H])C([H])([H])C([H])([H])C2=C([H])C2C([H])([H])C([H])([H])C([H])([H])C=21)=O)(=O)=O
|
|
| InChi Key |
LFQQNXFKPNZRFT-UHFFFAOYSA-M
|
|
| InChi Code |
InChI=1S/C20H24N2O5S.Na/c1-20(2,24)14-10-17(27-11-14)28(25,26)22-19(23)21-18-15-7-3-5-12(15)9-13-6-4-8-16(13)18;/h9-11,24H,3-8H2,1-2H3,(H2,21,22,23);/q;+1/p-1
|
|
| 化学名 |
sodium;1,2,3,5,6,7-hexahydro-s-indacen-4-ylcarbamoyl-[4-(2-hydroxypropan-2-yl)furan-2-yl]sulfonylazanide
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (6.18 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (6.18 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (6.18 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.4723 mL | 12.3616 mL | 24.7231 mL | |
| 5 mM | 0.4945 mL | 2.4723 mL | 4.9446 mL | |
| 10 mM | 0.2472 mL | 1.2362 mL | 2.4723 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。