| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| Other Sizes |
|
| 靶点 |
Broad spectrum anthelmintic
|
|---|---|
| 体外研究 (In Vitro) |
体外活性:硝唑尼特可减少细胞培养物中寄生虫的生长 90% 以上,几乎没有证据表明与药物相关的细胞毒性。 Nitazoxanide 是一种新型噻唑类抗寄生虫药,对多种原生动物和蠕虫表现出优异的体外活性。硝唑尼特及其代谢物替唑尼特在体外对肠杆菌、溶组织内阿米巴和阴道毛虫的活性比甲硝唑更强。 Nitazoxanide 可有效抑制 HBV 和 HCV 复制。在含有 HCV 复制子的细胞中,硝唑尼特可增强硝唑尼特加 IFN 的后续治疗效果,但不增强硝唑尼特加 2CmeC 的效果。 Nitazoxanide 可诱导 2.2.15 细胞产生的多种 HBV 蛋白(HBsAg、HBeAg、HBcAg)减少,但不影响 HBV RNA 转录。 Nitazoxanide 对溶组织内阿米巴的 IC50 和 IC90 值分别为 0.017 和 0.776 mg/mL,对肠杆菌的 IC50 和 IC90 值分别为 0.004 和 0.067 mg/mL,对阴道毛滴虫的 IC50 和 IC90 值分别为 0.034 和 2.046 mg/mL。硝唑尼特对溶组织内阿米巴的毒性比甲硝唑和阿苯达唑更强。
NTZ/硝唑尼特以剂量依赖的方式显著抑制JEV在培养细胞中的复制,50%有效浓度值为0.12±0.04μg/ml,这是培养细胞中无毒的浓度(50%细胞毒性浓度=18.59±0.31μg/ml)。计算出的化疗指数为154.92。与模拟处理的细胞相比,NTZ处理的细胞在感染后12、24、36和48小时的病毒产量显著降低。发现NTZ在病毒感染的早期中期发挥其抗JEV作用。[2] 含有溴而非硝基的NTZ/硝唑尼特衍生物(表1)对贾第鞭毛虫滋养体均无活性(IC50>50μM),但RM4820除外,其显示出中等抑制活性(IC50为18.8μM)低于RM4802和RM4805。MTZ的疗效低于NTZ和TIZ,但仍高于本研究中测试的任何其他药物。 为了观察由硝唑尼特诱导的G.lamblia滋养体的形态变化,并将其与MTZ诱导的形态变化进行比较,用50μM NTZ/Nitazoxanide或MTZ或DMSO作为对照处理融合的无菌滋养体培养物。光学显微镜观察显示,用NTZ处理3小时后,大约50%的滋养体是不动的;处理5小时后,95%以上的滋养体不动,形成大的多细胞聚集体;在NTZ处理24小时时未发现活动滋养体(数据未显示)。它们都表现出异常的液泡细胞质结构。透射电子显微镜的检查(图1)在很大程度上证实了这些发现,并表明在NTZ处理1小时后,相当多的滋养体在细胞质内已经表现出相对较小的异常细胞质内含物(图1A和B)。在处理3小时后,可以在大量寄生虫中观察到含有膜内含物或膜堆叠的较大液泡(图1C),在处理24小时后,这些寄生虫受到严重损伤,表现为细胞质组织的解离(图1D),或者在许多情况下,表现为含有膜残基的大液泡(图1E)。然而,除此之外,滋养体的细胞骨架元件,如与腹侧盘或鞭毛和基体相关的细丝,没有明显改变。在单独在DMSO中孵育的对照制剂中,未检测到寄生虫超微结构的明显变化(图1F)。[1] 在第一系列实验中,Caco2细胞在DMSO作为溶剂对照或30μM NTZ/Nitazoxanide硝唑尼特存在下与越来越多的滋养体(每孔103至106个寄生虫)一起孵育。然后通过实时PCR定量附着在Caco2细胞上的寄生虫(图4)。在没有任何药物的情况下,在每孔105个寄生虫的初始接种密度下,70%至90%的滋养体在24至48小时内保持附着在Caco2细胞上。在接种密度高出10倍(106个寄生虫/孔)时,该值降至近50%,表明与Caco2细胞表面的结合是可饱和的,并且取决于是否存在合适的结合位点和/或宿主细胞表面受体。在30μM NTZ的存在下,接种密度为105个滋养体,24小时后仍附着在Caco2细胞上的寄生虫数量降至对照值的20%以下。基于这些发现,我们研究了不同噻唑类药物与MTZ相比的效果。用新鲜的Caco2生长培养基补充汇合的Caco2细胞。向每个孔中加入滋养子(105),并加入许多噻唑类、MTZ和DMSO(图5)。24小时后收获细胞,通过实时PCR定量附着的滋养体。只有那些在无菌培养物中表现出强烈抑制作用的化合物(NTZ、TIZ、RM4802、RM4805和MTZ)会干扰Caco2共培养系统中的滋养体附着。与无菌培养相比,RM4802、RM4805和MTZ在Caco2共培养中的疗效与NTZ和TIZ相当(图5)。低于15μM的浓度对任何测试药物都没有显示出任何明显的抑制作用。[1] 对原生动物和厌氧细菌的研究表明,硝唑尼特/Nitazoxanide能够抑制丙酮酸铁氧还蛋白氧化还原酶(PFOR),这是一种对厌氧能量代谢至关重要的酶。然而,对PFOR酶依赖性电子转移反应的干扰可能不是硝唑尼特表现出抗原生动物活性的唯一途径,硝唑嗪对蠕虫的活性机制尚不清楚。 Nitazoxanide/硝唑尼特已被证明对细小隐球菌和肠杆菌具有体外活性。它已被证明可以单独抑制微小隐球菌子孢子的生长,并且还与阿奇霉素和利福平联合具有体外活性,分别抑制微小隐杆菌的生长83.9%和79.8%,而单独使用时为56.1%。同样,硝唑尼特及其衍生物替唑奈德的体外研究表明,其对肠道G.的疗效优于甲硝唑。具体而言,替唑硝胺对肠支原体甲硝唑敏感株的活性是甲硝唑的8倍,对耐药株的活性则是甲硝唑的两倍。 硝唑尼特还显示出对许多其他寄生虫和微生物病原体的广泛体外活性,包括肠杆菌、角膜弧菌、溶组织杆菌、阴道毛滴虫、人型棘球蚴、细粒棘球蚴和肝片吸虫。Nitazoxanide/硝唑尼特和替唑奈德的抗菌性能已对241种厌氧菌进行了测试,其中大部分在体外受到抑制,MIC90在0.06 mg/L至4 mg/L之间。硝唑嗪还对艰难梭菌以及甲硝唑敏感和甲硝唑耐药的幽门螺杆菌菌株显示出体外和体内抗菌活性[4]。 |
| 体内研究 (In Vivo) |
硝唑尼特以 250 mg/kg/天的剂量口服给药 11 天,可部分有效减少限生仔猪腹泻模型中的寄生虫负担,但 125 mg/kg/天的剂量则无效。硝唑尼特会引起仔猪药物相关性腹泻,这可能会影响其治疗效果。
NTZ/硝唑尼特可降低致死剂量乙脑攻击小鼠的死亡率[2] 为了评估NTZ对受致死剂量乙脑攻击的小鼠的保护作用,从感染后1天开始,每天以指定剂量灌胃给药NTZ,持续25天。感染乙脑并接受安慰剂(DMSO)治疗的小鼠(乙脑+DMSO组)从感染后5天开始出现乙脑的临床症状,包括肢体瘫痪、运动受限、竖毛、身体僵硬和全身震颤,所有小鼠(10/10只小鼠)在感染后9天内死亡。相比之下,感染JEV并接受NTZ治疗的小鼠(JEV+NTZ组,100mg/kg/天)从感染后11天开始出现JE的临床症状,在这10只小鼠中,1只在感染后12天内死亡,9只在实验期(25天)内存活(图6A)。NTZ介导的保护似乎是剂量依赖性的,因为接受50mg/kg/天、75mg/kg/天和100mg/kg/天NTZ的感染小鼠分别导致30%、70%和90%的小鼠存活(图6A)。这些数据表明,NTZ治疗降低了JEV感染小鼠的死亡率,并保护小鼠免受JEV致死剂量的攻击。模拟感染JEV并接受NTZ治疗的小鼠(mock+NTZ组)没有显示出可检测到的异常行为迹象,与模拟感染并接受DMSO治疗的小鼠相似(mock+DMSO组)(图6A)。对实验小鼠脑样本中JEV滴度的分析表明,与JEV+DMSO组相比,NTZ治疗显著降低了JEV+NTZ组脑中的病毒载量(图6B)。通过免疫组织化学检查实验小鼠的脑样本中是否存在病毒NS3蛋白。病毒NS3蛋白在神经元细胞的细胞质中被染色为棕色沉积物(附加文件1,箭头细胞)。JEV+DMSO组小鼠的脑切片显示,NS3染色阳性细胞的数量明显高于JEV+NTZ组。在Mock+NTZ或Mock+DMSO组小鼠的切片中未检测到NS3染色的阳性细胞。 对小鼠的研究。[3] 在急性隐孢子虫病的抗IFN-γ条件SCID小鼠模型中测试了NTZ/Nitazoxanide硝唑尼特单独或与PRM联合使用的疗效。虽然一项初步研究表明,Nitazoxanide/NTZ可以部分减少卵囊脱落(数据未显示),但我们无法在随后的几项实验中复制这一结果。以下是两项独立试验的合并结果,这些试验未能在该模型中显示疗效。单独使用NTZ治疗的任何组与安慰剂对照组之间的卵囊脱落对数没有差异(图1)。相比之下,所有接受PRM治疗的小鼠排出的卵囊水平明显低于单独接受NTZ或安慰剂治疗的小鼠(P<0.001)。NTZ和PRM的联合给药在降低卵囊脱落水平方面并不比单独使用PRM更有效。一般来说,在任何一组小鼠之间都没有观察到平均体重的显著差异(数据未显示)。 Student Newman-Keuls方差分析显示,单独使用NTZ或安慰剂治疗的小鼠的粘膜感染程度明显大于使用PRM治疗的动物(图2;P<0.001)。与单独接受PRM的小鼠相比,NTZ和PRM的联合给药没有显著改变粘膜感染的程度。 仔猪研究。[3] 仔猪模型提供了一个额外的优势,因为仔猪会因感染而腹泻。除了在治疗开始前对仔猪实施安乐死外,25只感染细小隐球菌的动物中有4只因与腹泻相关的健康状况不佳而实施安乐死,其中包括1只来自安慰剂组的仔猪(在感染后第5天),2只来自接受250mg硝唑尼特Nitazoxanide/NTZ/kg的组(在感染后第8天和第9天),1只来自PRM治疗组(在接种后第5天)。在攻击后第8天,对另外3头仔猪(1头安慰剂处理的仔猪、1头PRM处理的仔猪和1头未感染的对照仔猪)实施安乐死,以比较粘膜感染程度。对卵囊脱落水平和粘膜感染程度的分析表明,250mg/kg/天的NTZ显著降低了这些仔猪的粘膜感染程度,但不如500mg/kg/天的PRM有效(图3和图4)。 除PRM治疗组外,所有感染仔猪在攻击后56小时内均出现不同程度的腹泻。腹泻持续到实验结束,13天后(治疗开始后11天)。表2提供了每个治疗组观察到的腹泻天数的累积分析。对这些数据的卡方分析显示,治疗组之间存在非常显著的差异(总体皮尔逊卡方值为88.096,5 df;P<0.001)。以125mg/kg/天的剂量给予硝唑尼特/NTZ的未感染仔猪没有腹泻(24天观察中为0天)。相比之下,在36个观察日中的22个观察日,以250mg/kg/天的剂量给予NTZ的未感染仔猪出现了明显的药物性腹泻(Pearson卡方检验和Fisher精确检验[双尾]的P≤0.001)。在感染组中,只有PRM治疗组的腹泻频率低于感染安慰剂对照组。PRM治疗组仔猪出现腹泻的观察天数百分比明显低于其他任何感染组(卡方P<0.001,Fisher精确双尾检验P<0.001,与感染的安慰剂对照组、接受125 mg/kg/天NTZ的组和接受250 mg/kg/天NT Z的组进行比较)。 |
| 细胞实验 |
细胞系:贾第鞭毛虫滋养体在人结肠癌 Caco2 细胞中培养,数量不断增加(每孔 103–106 个寄生虫)。
浓度:30 μM 孵育时间:24 小时 结果:当硝唑尼特未添加时存在并且初始接种密度为每孔 105 个寄生虫,70-90% 的滋养体在 24-48 小时内粘附在 Caco2 细胞上。在 30 μM 硝唑尼特存在且接种密度为 105 个滋养体的情况下, 24小时后仍附着在Caco2细胞上的寄生虫数量下降至对照值的20%以下。 病毒、细胞和硝唑尼特Nitazoxanide/NTZ给药[2] JEV毒株(SH-JEV01)在3天大的BALB/c小鼠中生长,并使用BHK-21细胞通过空斑试验进行滴定,如下所述。BHK-21 细胞在37°C的Dulbecco改良Eagle培养基(DMEM)中,在含有5%CO2的气氛中,补充了10%胎牛血清(FBS)。 将NTZ/硝唑尼特(纯度≥98%)以50μg/μl的浓度溶解在培养级DMSO 中。除非另有说明,否则在1小时的吸附期后立即加入NTZ溶液,并在实验期间将其保持在培养基中。对照组接受等量的DMSO(终浓度≤0.06%),其不影响细胞活力或病毒复制。 细胞毒性试验[2] BHK-21细胞以每孔5×103个细胞的密度接种在96孔板中。孵育24小时后,在37°C下用0.1至32μg/ml的不同浓度的NTZ处理细胞48小时。单独用DMSO处理的细胞用作对照。采用MTT法评估NTZ的细胞毒性。细胞存活率以DMSO处理的对照细胞总数的百分比计算。CC50定义为抑制指数生长细胞增殖50%的浓度,按所述计算。 NTZ/硝唑尼特在BHK-21细胞中的抗病毒作用分析[2] 六孔板中的BHK-21细胞以0.001的MOI感染JEV。在1小时的吸附期后,用浓度为0.01至10μg/ml的NTZ处理细胞,并在37°C下孵育48小时或指定时间。通过空斑试验和qRT-PCR确定病毒产量。病毒滴度的降低计算如下:病毒滴度降低%=[1-(PFUJEV+NTZ/PFUJEV+DMSO)]×100。EC50定义为在细胞中抑制病毒产量50%的浓度,如所述计算。 NTZ/硝唑尼特在细胞培养中的活性。[3] 将选择性克隆的MDBK细胞接种在96孔微升平板上,以检测其对细小隐球菌感染的敏感性。为了确定NTZ的剂量反应,72小时后,当细胞融合时,将3.0×104 C.parvum卵囊与或不与药物一起添加到每个孔中。硫酸巴诺霉素(PRM)用作阳性对照药物。所有药物稀释液均在添加了5%胎牛血清、500 U青霉素、500μg链霉素/ml、1 mM丙酮酸钠、2 mM l-谷氨酰胺和0.2%二甲亚砜(DMSO)(培养基)的Dulbecco最低必需培养基中制备。将培养基添加到含有感染微小隐球菌卵囊的MDBK细胞的孔中作为阴性对照。所有药物浓度和对照品均进行了四次测试。孵育48小时(37°C,8%CO2)后,单层被甲醇固定,并在间接免疫荧光测定中反应,以确定感染强度。固定孔用含有1%正常山羊血清(NGS)的磷酸盐缓冲盐水(PBS)复水15分钟。复水后,将寄生虫反应性兔抗血清在含有1%NGS的PBS中稀释1:1000,加入孔中,在室温下孵育1小时。所有孔用PBS洗涤三次,用异硫氰酸荧光素偶联的山羊抗兔免疫球蛋白G抗体在含有1%NG的PBS中以1:100稀释检测结合抗体。在室温下温育1小时后,用PBS洗涤孔三次并干燥。在紫外光显微镜下,用专门为此目的设计的微型计算机视频成像设备定量微小念珠菌感染的程度。感染抑制百分比计算如下:1−(药物孔中的平均寄生虫数/对照孔中的寄生虫平均数)×100。所有结果的抑制分数分别为0、1、2、3和4,抑制率分别为0至30%、31至55%、56至70%、71至90%和91至100%。 细胞毒性试验。[3] 通过CellTiter 96 AQueous非放射性细胞增殖试验测定NTZ/硝唑尼特和PRM对MDBK细胞的细胞毒性。每种细胞毒性试验的对照包括(i)在培养基中孵育的未感染细胞,(ii)在培养基中孵育了感染细胞,以及(iii)暴露于培养基中含有3.0×104卵囊当量的冻融裂解物的细胞。根据光密度(OD)计算细胞毒性百分比,如下所示:[(未感染细胞的平均OD-感染细胞的均值OD)/未感染细胞平均OD]×100。所有结果的细胞毒性评分分别为0、1、2、3和4,细胞毒性百分比分别为0至5%、6至25%、26至50%、51至75%和76至100%。细胞毒性评分为0、1和2分别表示无毒性、轻度毒性和中度毒性,评分为3和4表示MDBK细胞的重度毒性。当感染细胞的OD大于未感染细胞的OD时,会产生负百分比毒性。 |
| 动物实验 |
Animal Model: JEV was injected intraperitoneally into female Chinese Kunming mice that were three weeks old and weighed between 12 and 14 grams.[2]
Dosage: 50, 75 or 100 mg/kg/day Administration: Administered intragastrically by gavage Result: 50 mg/kg/day, 75 mg/kg/day and 100 mg/kg/day led to 30%, 70% and 90% mice survival, respectively. NTZ/Nitazoxanide activity in SCID mice. [3] The anti-gamma-interferon (IFN-γ)-conditioned SCID mouse model has been described previously. Briefly, newly weaned (3- to 4-week-old) male inbred C.B-17 SCID mice were housed in microisolator cages in IACUC-approved facilities. Prior to the initiation of a drug trial, the animals were randomized into seven groups of seven mice each. Each mouse was primed with an intraperitoneal injection of 1 mg of XMG1.2, an IFN-γ-neutralizing monoclonal antibody. Two hours later, each mouse in six of the seven groups received an oral inoculation of 107 oocysts. Drug treatment was initiated on day 6 of infection, coinciding with the onset of oocyst excretion in the feces. Treatment schedules were as follows: group 1, 200 mg of NTZ/kg of body weight/day; group 2, 100 mg of NTZ/kg/day; group 3, 200 mg of NTZ/kg/day combined with 2,500 mg of PRM/kg/day; group 4, 100 mg of NTZ/kg/day combined with 2,500 mg of PRM/kg/day, and group 5, 2,500 mg of PRM/kg/day. NTZ was dissolved in 100% DMSO and administered orally in two divided doses of 30 μl each per day. PRM was dissolved in the drinking water to a concentration of 10 mg/ml (16.2 mM), resulting in a dose of 2,500 mg/kg/day based on the daily water consumption. Group 6 consisted of uninfected mice treated with 200 mg of NTZ/kg/day combined with 2,500 mg of PRM/kg/day (drug toxicity control group). Group 7 consisted of seven mice treated orally with 30 μl of DMSO twice per day (the placebo control group). All mice were treated for 10 days and maintained for an additional 5 days after the end of treatment. The level of oocyst shedding was determined three times per week throughout the study by microscopic observation of 30 high-power fields of a modified acid-fast stained fecal smear from each infected animal. Results are presented as the mean log oocysts shed per group ± the 95% confidence intervals. Body weights were determined one time per week throughout the study. Results are presented as the mean body weight per group ± the 95% confidence intervals. At necropsy, sections were taken from the pyloric region of the stomach, mid-small intestine, ileum, cecum, and proximal colon for histologic analysis to determine the extent of mucosal infection. Each site was assigned a score depending on the extent of infection, as follows: 0, no infection; 1, very difficult-to-find parasite forms; 2, sparse but easily found parasite forms; 3, abundant parasite forms but focally distributed; 4, extensive presence of parasite forms covering most mucosal surfaces; and 5, extensive presence of parasite forms covering the entire mucosal surface. The data are presented as the mean total score of the five sites ± 95% confidence intervals. NTZ/Nitazoxanide activity in the piglet diarrhea model. [3] Thirty-one gnotobiotic piglets derived by cesarean section from four litters were maintained inside sterile isolators for the duration of the experiment as described previously. Twenty-six of the 31 piglets were challenged with oocysts 24 h after derivation. Because these experiments were not performed simultaneously, the infecting dose of 5 × 106 excysting oocysts was calculated based on the percent oocyst excystation in vitro (rate of excystation). The rate of in vitro excystation was determined following incubation of the oocysts in 0.75% taurocholic acid for 45 min at 37°C. Once the in vitro excystation rate was determined, the inocula were adjusted accordingly so that 13 piglets received 2 × 107 oocysts and 13 piglets received 7 × 106 oocysts. Piglets were observed two or three times daily for signs of diarrhea, depression, and anorexia and for overall appearance. Diarrhea was defined as a twofold increase in the frequency, volume, and water content of the fecal discharge of a piglet compared to those in uninfected control piglets. Body weights and fecal samples were obtained daily. Within 3 days after challenge, piglets were assigned to groups based on a combination of body weight, onset of oocyst shedding, and diarrhea status. The piglets were then started on a daily treatment schedule of either 250 mg of Nitazoxanide/NTZ/kg (five piglets), 125 mg of NTZ/kg (six piglets), 500 mg of PRM/kg (five piglets), or a placebo (milk; nine piglets). Five uninfected control animals served as drug toxicity controls; three piglets received NTZ at 250 mg/kg/day, and two piglets received 125 mg/kg/day. One of the 26 infected piglets was euthanized because of severe illness and was excluded from the study. All drugs were administered via the milk diet in two divided doses daily for 11 days. The number of oocysts present in an entire modified-acid-fast-stained fecal smear was determined daily for each piglet. Since piglets develop diarrhea as a consequence of C. parvum infection, determination of the number of oocysts shed must account for any variability in fecal consistency that we observe. In particular, the presence of watery diarrhea will influence the number of oocysts detected in a fecal smear due to the effective dilution of the fecal material by the increased fluid content. Because of this, we have devised a scoring system that accounts for both the qualitative nature of the fecal material and the number of oocysts detected. Scores are assigned in this system as follows: 0, no oocysts detected; 1, ≤10 oocysts; 2, ≤25 oocysts; 3, ≤50 oocysts; 4, ≤100 oocysts; and 5, >100 oocysts. Results are presented as the mean oocyst shedding score for each treatment group ± standard error of the mean. Surviving piglets were euthanized 11 days after the onset of treatment, and six gut sections (the pyloric region of the stomach, three equally spaced small intestinal sites, the cecum, and the colon) were removed for histologic analysis of the extent of mucosal infection. Each site was assigned a score depending on the extent of infection by the system described above for the anti-IFN-γ-conditioned SCID mouse. Results are presented as the total score of the six sites for individual piglets. Analysis of the antiviral effect of NTZ/Nitazoxanide in a mouse model[2] Three-week old female Chinese Kunming mice (12–14 g body weight) were randomly divided into six groups (10 mice/group). Group JEV + NTZ was infected with JEV and received NTZ treatment (50, 75 or 100 mg/kg/day). Group JEV + DMSO was infected with JEV and received a placebo (DMSO) treatment. Group Mock + NTZ was mock-infected with JEV and received NTZ treatment. Group Mock + DMSO was mock-infected with JEV and received a placebo (DMSO) treatment. For infection, mice were infected intraperitoneally with 6×104 PFU of JEV (containing 50 × LD50 of JEV). For NTZ treatment, NTZ was dissolved in DMSO and administered intragastrically by gavage, in which a feeding needle was introduced into the esophagus and NTZ was delivered directly into the stomach. NTZ was tested at a total dose of 50, 75 or 100 mg/kg/day, and was consecutively administered from 1 day post-infection, daily, for up to 25 days. The mice were monitored daily for morbidity and mortality. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
The relative bioavailability of the suspension compared to the tablet was 70%. When administered with food the AUC and Cmax increased by two-fold and 50%, respectively, for the tablet and 45 to 50% and ≤ 10%, respectively, for the oral suspension. Tizoxanide is excreted in the urine, bile and feces, and tizoxanide glucuronide is excreted in urine and bile. Approximately 2/3 of the oral dose of nitazoxanide is excreted in the faeces and 1/3 in the urine. Nitazoxanide is cleared in the urine and feces. The metabolite, tizoxanide, is also found in the urine, plasma, and breastmilk. The drug is not found unchanged in the urine. Metabolism / Metabolites The active metabolite of this drug is tizoxanide (desacetyl-nitazoxanide). The initial reaction in the metabolic pathway of Nitazoxanide is hydrolysis to tizoxanide, followed by conjugation, primarily by glucuronidation to tizoxanide glucuronide. The oral suspension bioavailability of this drug is not equivalent to that of the oral tablets. Compared to the to the tablet, the bioavailability of the suspension was 70%. When administered with food, the AUCt of tizoxanide and tizoxanide glucuronide in plasma is increased to almost two-fold and the maximum concentration is increased by almost 50% compared to when ingested without food. When the oral suspension was ingested with food, the AUC of tizoxanide and tizoxanide glucuronide increased by approximately 50% and the Cmax increased by less than 10%. Biological Half-Life 7.3h |
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
Nitazoxanide therapy has not been associated with elevations in serum aminotransferase levels nor with clinically apparent acute liver injury. However, there have been few studies of long term therapy with nitazoxanide and most controlled trials of this agent used short term courses without serum aminotransferase monitoring. Nitazoxanide has been used as adjunctive therapy for chronic hepatitis C, usually in combination with peginterferon with or without ribavirin; in these studies, most patients had improvements in serum aminotransferase levels, and no instances of acute exacerbation of hepatitis or jaundice were reported. Likelihood score: E (unlikely cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Limited information indicates that a maternal dose of 500 mg of nitazoxanide produces low levels of an active metabolite, tizoxanide, in breastmilk and would not be expected to cause any adverse effects in breastfed infants, especially if the infant is older than 2 months. But until more data become available, an alternate drug may be preferred, especially while nursing a newborn or preterm infant. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding Very High (greater than 99%), bound to proteins in the plasma. Drug Interactions [4] At this time, no drug-drug interaction studies have been conducted with nitazoxanide in vivo. Because >99% of tizoxanide is bound to plasma proteins, caution should be used when administering nitazoxanide concurrently with other highly plasma protein—bound drugs with narrow therapeutic indices. It is recommended to monitor the prothrombin time for patients who are concurrently taking warfarin and nitazoxanide. Side Effects [4] Nitazoxanide is generally well tolerated, and no significant adverse events have been noted in human trials. Adverse events have been mild and transient and principally related to the gastrointestinal tract, such as abdominal pain, diarrhea, and nausea. Adverse events occurring in <1% of more than 2000 HIV-uninfected patients participating in clinical trials included anorexia, flatulence, increased appetite, enlarged salivary glands, fever, infection, malaise, elevated creatinine levels, elevated levels of alanine aminotransferase in serum, pruritus, sweat, pale yellow sclerae, rhinitis, dizziness, and discolored urine. In addition, there have been no significant changes in results of electrocardiography, vital signs, or hematologic, clinical chemistry, or urinalysis parameters in patients treated with nitazoxanide. Nitazoxanide has been well tolerated up to the maximum dose of 4 g when taken with or without food, but the frequency of gastrointestinal side effects increases significantly with the dose level. |
| 参考文献 | |
| 其他信息 |
Pharmacodynamics
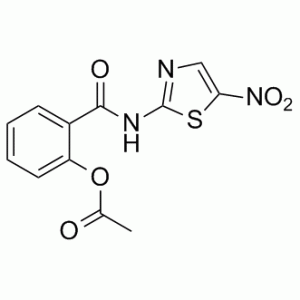
The general effect of this medication is the prevention of microbe activity through disruption of important energy pathways for survival and proliferation. Nitazoxanide exhibits antiprotozoal activity by interfering with the pyruvate ferredoxin/flavodoxin oxidoreductase dependent electron transfer reaction, an essential reaction need for anaerobic energy metabolism of various microorganisms. Sporozoites of Cryptosporidium parvum and trophozoites of Giardia lamblia are therefore inhibited, relieving symptoms of diahrrea. Interference with the PFOR enzyme-dependent electron transfer reaction may only be one of the many pathways by which nitazoxanide exhibits antiprotozoal activity. Acetic acid [2-[[(5-nitro-2-thiazolyl)amino]-oxomethyl]phenyl] ester is a carboxylic ester and a member of benzamides. It is functionally related to a salicylamide. Nitazoxanide belongs to the class of drugs known as thiazolides. Nitazoxanide (NTZ) is a broad-spectrum anti-infective drug that markedly modulates the survival, growth, and proliferation of a range of extracellular and intracellular protozoa, helminths, anaerobic and microaerophilic bacteria, in addition to viruses. This drug is effective in the treatment of gastrointestinal infections including Cryptosporidium parvum or Giardia lamblia in healthy subjects. It is generally well tolerated. Nitazoxanide is a first-line, standard treatment for illness caused by C. parvum or G. lamblia infection in healthy (not immunosuppressed) adults and children and may also be considered in the treatment of illnesses caused by other protozoa or helminths. Recently, this drug has been studied as a broad-spectrum antiviral agent due to its ability to inhibit the replication of several RNA and DNA viruses. Nitazoxanide is an Antiprotozoal. Nitazoxanide is an antimicrobial with activity against several parasitic worms and protozoa that is used predominantly in the United States in treatment of giardiasis and cryptosporidiosis. Nitazoxanide therapy has not been reported to cause serum aminotransferase elevations during therapy or clinically apparent liver injury. Nitazoxanide is a synthetic benzamide with antiprotozoal activity. Nitazoxanide exerts its antiprotozoal activity by interfering with the pyruvate ferredoxin/flavodoxin oxidoreductase dependent electron transfer reaction, which is essential to anaerobic energy metabolism. PFOR enzyme reduces nitazoxanide, thereby impairing the energy metabolism. However, interference with the PFOR enzyme-dependent electron transfer reaction may not be the only pathway by which nitazoxanide exhibits antiprotozoal activity. Nitazoxanide is active against Giardia lamblia and Cryptosporidium parvum. NITAZOXANIDE is a small molecule drug with a maximum clinical trial phase of IV (across all indications) that was first approved in 2002 and is indicated for amebiasis and diarrhea and has 26 investigational indications. The thiazolides represent a novel class of anti-infective drugs, with the nitrothiazole nitazoxanide [2-acetolyloxy-N-(5-nitro 2-thiazolyl) benzamide] (NTZ) as the parent compound. NTZ exhibits a broad spectrum of activities against a wide variety of helminths, protozoa, and enteric bacteria infecting animals and humans. In vivo, NTZ is rapidly deacetylated to tizoxanide (TIZ), which exhibits similar activities. We have here comparatively investigated the in vitro effects of NTZ, TIZ, a number of other modified thiazolides, and metronidazole (MTZ) on Giardia lamblia trophozoites grown under axenic culture conditions and in coculture with the human cancer colon cell line Caco2. The modifications of the thiazolides included, on one hand, the replacement of the nitro group on the thiazole ring with a bromide, and, on the other hand, the differential positioning of methyl groups on the benzene ring. Of seven compounds with a bromo instead of a nitro group, only one, RM4820, showed moderate inhibition of Giardia proliferation in axenic culture, but not in coculture with Caco2 cells, with a 50% inhibitory concentration (IC50) of 18.8 microM; in comparison, NTZ and tizoxanide had IC50s of 2.4 microM, and MTZ had an IC50 of 7.8 microM. Moreover, the methylation or carboxylation of the benzene ring at position 3 resulted in a significant decrease of activity, and methylation at position 5 completely abrogated the antiparasitic effect of the nitrothiazole compound. Trophozoites treated with NTZ showed distinct lesions on the ventral disk as soon as 2 to 3 h after treatment, whereas treatment with metronidazole resulted in severe damage to the dorsal surface membrane at later time points. [1] Background: Japanese encephalitis virus (JEV) has a significant impact on public health. An estimated three billion people in 'at-risk' regions remain unvaccinated and the number of unvaccinated individuals in certain Asian countries is increasing. Consequently, there is an urgent need for the development of novel therapeutic agents against Japanese encephalitis. Nitazoxanide (NTZ) is a thiazolide anti-infective licensed for the treatment of parasitic gastroenteritis. Recently, NTZ has been demonstrated to have antiviral properties. In this study, the anti-JEV activity of NTZ was evaluated in cultured cells and in a mouse model. Methods: JEV-infected cells were treated with NTZ at different concentrations. The replication of JEV in the mock- and NTZ-treated cells was examined by virus titration. NTZ was administered at different time points of JEV infection to determine the stage at which NTZ affected JEV replication. Mice were infected with a lethal dose of JEV and intragastrically administered with NTZ from 1 day post-infection. The protective effect of NTZ on the JEV-infected mice was evaluated. Findings: NTZ significantly inhibited the replication of JEV in cultured cells in a dose dependent manner with 50% effective concentration value of 0.12 ± 0.04 μg/ml, a non-toxic concentration in cultured cells (50% cytotoxic concentration = 18.59 ± 0.31 μg/ml). The chemotherapeutic index calculated was 154.92. The viral yields of the NTZ-treated cells were significantly reduced at 12, 24, 36 and 48 h post-infection compared with the mock-treated cells. NTZ was found to exert its anti-JEV effect at the early-mid stage of viral infection. The anti-JEV effect of NTZ was also demonstrated in vivo, where 90% of mice that were treated by daily intragastric administration of 100 mg/kg/day of NTZ were protected from a lethal challenge dose of JEV. Conclusions: Both in vitro and in vivo data indicated that NTZ has anti-JEV activity, suggesting the potential application of NTZ in the treatment of Japanese encephalitis. [2] Nitazoxanide (NTZ), a drug currently being tested in human clinical trials for efficacy against chronic cryptosporidiosis, was assessed in cell culture and in two animal models. The inhibitory activity of NTZ was compared with that of paromomycin (PRM), a drug that is partially effective against Cryptosporidium parvum. A concentration of 10 microg of NTZ/ml (32 microM) consistently reduced parasite growth in cell culture by more than 90% with little evidence of drug-associated cytotoxicity, in contrast to an 80% reduction produced by PRM at 2,000 microg/ml (3.2 mM). In contrast to its efficacy in vitro, NTZ at either 100 or 200 mg/kg of body weight/day for 10 days was ineffective at reducing the parasite burden in C. parvum-infected, anti-gamma-interferon-conditioned SCID mice. Combined treatment with NTZ and PRM was no more effective than treatment with PRM alone. Finally, NTZ was partially effective at reducing the parasite burden in a gnotobiotic piglet diarrhea model when given orally for 11 days at 250 mg/kg/day but not at 125 mg/kg/day. However, the higher dose of NTZ induced a drug-related diarrhea in piglets that might have influenced its therapeutic efficacy. As we have previously reported, PRM was effective at markedly reducing the parasite burden in piglets at a dosage of 500 mg/kg/day. Our results indicate that of all of the models tested, the piglet diarrhea model most closely mimics the partial response to NTZ treatment reported to occur in patients with chronic cryptosporidiosis.[3] Nitazoxanide is a new thiazolide antiparasitic agent that shows excellent in vitro activity against a wide variety of protozoa and helminths. It is given by the oral route with good bioavailability and is well tolerated, with primarily mild gastrointestinal side effects. At present, there are no documented drug-drug interactions. Nitazoxanide has been licensed for the treatment of Giardia intestinalis-induced diarrhea in patients >or=1 year of age and Cryptosporidum-induced diarrhea in children aged 1-11 years. At present, it is pending licensure for treatment of infection due to Cryptosporidium species in adults and for use in treating immunocompromised hosts. It represents an important addition to the antiparasitic arsenal.[4] |
| 分子式 |
C12H9N3O5S
|
|---|---|
| 分子量 |
307.28
|
| 精确质量 |
307.026
|
| 元素分析 |
C, 46.90; H, 2.95; N, 13.67; O, 26.03; S, 10.44
|
| CAS号 |
55981-09-4
|
| 相关CAS号 |
Nitazoxanide-d4;1246819-17-9
|
| PubChem CID |
41684
|
| 外观&性状 |
Light yellow to yellow solid powder
|
| 密度 |
1.5±0.1 g/cm3
|
| 熔点 |
202ºC
|
| 折射率 |
1.673
|
| LogP |
1.79
|
| tPSA |
142.35
|
| 氢键供体(HBD)数目 |
1
|
| 氢键受体(HBA)数目 |
7
|
| 可旋转键数目(RBC) |
4
|
| 重原子数目 |
21
|
| 分子复杂度/Complexity |
428
|
| 定义原子立体中心数目 |
0
|
| SMILES |
S1C(=C([H])N=C1N([H])C(C1=C([H])C([H])=C([H])C([H])=C1OC(C([H])([H])[H])=O)=O)[N+](=O)[O-]
|
| InChi Key |
YQNQNVDNTFHQSW-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C12H9N3O5S/c1-7(16)20-9-5-3-2-4-8(9)11(17)14-12-13-6-10(21-12)15(18)19/h2-6H,1H3,(H,13,14,17)
|
| 化学名 |
[2-[(5-nitro-1,3-thiazol-2-yl)carbamoyl]phenyl] acetate
|
| 别名 |
NSC-697855; NTZ; NSC 697855;NSC697855; NITAZOXANIDE; 55981-09-4; Alinia; Nitazoxanida; 2-((5-nitrothiazol-2-yl)carbamoyl)phenyl acetate; Nitazoxamide; Nitazoxanidum; Daxon; Alinia, Colufase, Daxon, Nitazoxamide
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : 61~100 mg/mL ( 198.51~325.44 mM )
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 3.25 mg/mL (10.58 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 32.5 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: 10% DMSO+40% PEG300+5% Tween-80+45% Saline: ≥ 3.25 mg/mL (10.58 mM) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 3.2544 mL | 16.2718 mL | 32.5436 mL | |
| 5 mM | 0.6509 mL | 3.2544 mL | 6.5087 mL | |
| 10 mM | 0.3254 mL | 1.6272 mL | 3.2544 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
 Forward genetic screen for identification of NTZ resistant worm mutants.Mol Biochem Parasitol.2014 Jan;193(1):1-8. |
|---|
Dose response curves ofC. elegansmutants resistant to other classes of drugs to NTZ in a six day lethality assay.Mol Biochem Parasitol.2014 Jan;193(1):1-8. |
Combination of NTZ with albendazole (ALB) and pyrantel (PYR).Mol Biochem Parasitol.2014 Jan;193(1):1-8. |
 Ivermectin (IVM) susceptibility of the two NTZ resistant mutants identified in forward genetic screens at 44–45 hours.Mol Biochem Parasitol.2014 Jan;193(1):1-8. |
|---|
Effect of NTZ onC. elegansN2 wild-type nematodes.Mol Biochem Parasitol.2014 Jan;193(1):1-8. |