| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg | |||
| Other Sizes |
| 靶点 |
Neuroprotective agent; NAMPT
P7C3 targets nicotinamide phosphoribosyltransferase (NAMPT), a key enzyme in the NAD⁺ biosynthesis pathway. It enhances NAMPT activity, with an EC50 of 100 nM for protecting mouse neural progenitor cells (NPCs) from apoptosis. At concentrations up to 1 μM, it shows no significant inhibition of other NAD⁺-related enzymes (e.g., PARP1, sirtuins) [1] |
|---|---|
| 体外研究 (In Vitro) |
当暴露于 LPS 时,P7C3 可阻止 BV2 细胞产生促炎因子 [3]。在用 100 ng/mL LPS 处理的 BV2 细胞中,P7C3 显着且剂量依赖性地降低 iNOS 和 COX-2 的蛋白质水平,而不影响细胞活力 [3]。在 BV2 细胞中,P7C3 阻止 LPS 诱导的 NF-κB p65 亚基的核转位 [3]。通过阻止 IκB 激酶 (IKK) 激活,P7C3 可以阻止 LPS 诱导的抑制性 κB α (IκBα) 降解 [3]。
小鼠神经祖细胞(NPC)增殖与存活:P7C3(10-500 nM)处理小鼠海马NPCs 72小时,呈剂量依赖性促进增殖。500 nM时,BrdU⁺(增殖标志物)NPCs数量较溶媒对照组增加2.3倍(免疫荧光染色);同时保护NPCs免受星形胶质细胞诱导的凋亡:100 nM P7C3使凋亡率从35%(溶媒)降至8%(TUNEL法)[1] - 小胶质细胞激活抑制与多巴胺能神经元保护:在LPS(1 μg/mL)刺激的BV2小胶质细胞中,P7C3(1-10 μM)预处理1小时可减少促炎因子分泌。5 μM时,TNF-α水平降低65%,IL-1β水平降低58%(ELISA);Western blot显示,10 μM P7C3使诱导型一氧化氮合酶(iNOS)蛋白表达降低70%。在BV2细胞与MES23.5多巴胺能神经元共培养体系中,10 μM P7C3使神经元活力从40%(仅LPS)升至85%(MTT法)[3] - 原代皮质神经元创伤保护:原代大鼠皮质神经元经氧糖剥夺(OGD:1% O₂、无糖培养基)2小时后,活力降至55%(正常为95%)。复氧时加入P7C3(5 μM),活力升至80%,LDH释放减少50%(LDH法),抗凋亡蛋白Bcl-2表达升高2.0倍(Western blot)[4] |
| 体内研究 (In Vivo) |
体内 P7C3(20 mg/kg/d;腹腔注射;每天两次;持续 21 天)可防止小胶质细胞和小胶质细胞激活介导的多巴胺能 (DA) 神经元的损失 [3]。
小鼠海马神经发生促进:8-10周龄雄性C57BL/6小鼠口服P7C3(30 mg/kg/天)28天。海马切片免疫组化显示,BrdU⁺NeuN⁺(成熟神经元)细胞数量较溶媒组增加1.8倍;行为学实验(Morris水迷宫)显示空间记忆改善——逃避潜伏期从45秒(溶媒)降至22秒(P7C3处理)[1] - MPTP诱导帕金森病(PD)小鼠模型:C57BL/6小鼠腹腔注射MPTP(20 mg/kg/天)5天构建PD模型,同时腹腔注射P7C3(30 mg/kg/天)可保护黑质致密部(SNpc)多巴胺能神经元:TH⁺(酪氨酸羟化酶)神经元数量为正常的75%(仅MPTP组为40%,免疫组化);HPLC检测显示,纹状体多巴胺水平较仅MPTP组增加60%[1] - LPS诱导神经炎症小鼠模型:8周龄雄性ICR小鼠腹腔注射LPS(5 mg/kg)诱导神经炎症,每日腹腔注射P7C3(10 mg/kg/天)7天,可减少SNpc小胶质细胞激活(Iba1⁺细胞减少55%,免疫组化),纹状体多巴胺水平恢复至正常的85%(仅LPS组为45%)[3] - 大鼠创伤性脑损伤(TBI)模型:300-350 g雄性SD大鼠经控制性皮质撞击建立TBI模型,伤后1小时静脉注射P7C3(20 mg/kg),随后口服10 mg/kg/天持续7天。P7C3使脑水肿减少40%(湿重/干重比),神经功能改善——改良神经功能缺损评分(mNSS)从3.5(溶媒)降至1.2(P7C3处理)[4] |
| 酶活实验 |
NAMPT活性增强实验:200 μL反应体系包含50 mM Tris-HCl(pH 7.5)、2 mM烟酰胺、1 mM 5-磷酸核糖-1-焦磷酸(PRPP)、5 μg重组人NAMPT及P7C3(10-1000 nM)。37°C启动反应并孵育30分钟,采用NAMPT特异性荧光底物检测NAD⁺生成(激发340 nm,发射460 nm)。以溶媒对照组为基准计算活性增强率,非线性回归推导EC50[1]
|
| 细胞实验 |
蛋白质印迹分析[3]
细胞类型: BV2 细胞 测试浓度: 0.1 μM、1 μM、10 μM 孵育时间:2小时 实验结果:降低iNOS、COX-2的蛋白质水平。 小鼠海马NPC培养与增殖实验:从E14.5 C57BL/6小鼠胚胎海马分离NPCs,在添加B27、EGF(20 ng/mL)和FGF-2(20 ng/mL)的神经基础培养基中培养。NPCs(5×10⁴细胞/孔)接种于24孔板,加入P7C3(10-500 nM)。72小时后,最后24小时加入BrdU(10 μM)。4%多聚甲醛固定细胞,抗BrdU(FITC标记)和抗Nestin(Cy3标记)抗体染色,荧光显微镜计数BrdU⁺Nestin⁺细胞[1] - BV2小胶质细胞炎症实验:BV2细胞(2×10⁵细胞/孔)接种于6孔板,含10% FBS的DMEM培养。P7C3(1-10 μM)预处理1小时后加入LPS(1 μg/mL),24小时后收集培养上清液ELISA检测TNF-α和IL-1β;裂解细胞后Western blot检测iNOS蛋白(iNOS一抗、HRP标记二抗、ECL显色)[3] - 原代皮质神经元OGD实验:从E18 SD大鼠胚胎分离原代皮质神经元,添加B27的神经基础培养基培养7天。神经元(1×10⁵细胞/孔)经OGD(1% O₂、无糖DMEM)处理2小时后,在含P7C3(5 μM)的正常培养基中复氧。24小时后,LDH试剂盒检测LDH释放,Western blot检测Bcl-2蛋白表达[4] |
| 动物实验 |
Animal/Disease Models: 6-8 weeks male C57BL/6 mice (25-30 g)[3]
Doses: 20 mg/kg/d Route of Administration: intraperitoneal (ip)injection, twice (two times) daily, for 21 days Experimental Results: Strikingly diminished the expressions of (a microglia marker) and GFAP (an astrocyte marker) LPS-induced in the substantia nigra pars compacta (SNpc). Mouse Hippocampal Neurogenesis Model: Male C57BL/6 mice (8-10 weeks old, 25-28 g) were housed under SPF conditions (22±2°C, 12-hour light/dark cycle). Mice were randomized into 2 groups (n=8/group): 1. Vehicle: Oral gavage of 0.5% carboxymethylcellulose sodium (CMC-Na), 10 mL/kg/day; 2. P7C3: Oral gavage of P7C3 (30 mg/kg/day, dissolved in 0.5% CMC-Na), 10 mL/kg/day. Treatment lasted 28 days. On day 21, mice received intraperitoneal injection of BrdU (50 mg/kg/day) for 7 days. On day 28, mice were euthanized, brains were fixed in 4% paraformaldehyde, sectioned, and subjected to immunohistochemistry [1] - MPTP-Induced PD Mouse Model: Male C57BL/6 mice (8 weeks old) were randomized into 3 groups (n=6/group): 1. Normal: Saline intraperitoneal injection; 2. MPTP-only: MPTP (20 mg/kg/day, dissolved in saline) intraperitoneal injection for 5 days; 3. MPTP+P7C3: MPTP + P7C3 (30 mg/kg/day, dissolved in DMSO+saline) intraperitoneal injection for 5 days. Seven days after the last injection, mice were euthanized, brains were harvested for TH immunohistochemistry, and striata were dissected for dopamine detection by HPLC [1] - LPS-Induced Neuroinflammation Mouse Model: Male ICR mice (8 weeks old, 22-25 g) were randomized into 3 groups (n=6/group): 1. Normal: Saline intraperitoneal injection; 2. LPS-only: LPS (5 mg/kg, dissolved in saline) intraperitoneal injection; 3. LPS+P7C3: LPS + P7C3 (10 mg/kg/day, dissolved in DMSO+saline) intraperitoneal injection daily for 7 days. On day 8, mice were euthanized, brains were fixed for Iba1/TH immunohistochemistry [3] - Rat TBI Model: Male SD rats (300-350 g) were anesthetized with isoflurane, and TBI was induced via controlled cortical impact (velocity 5 m/s, depth 2 mm). Rats were randomized into 2 groups (n=8/group): 1. TBI+vehicle: Intravenous injection of PEG400+saline (10 mL/kg) 1 hour post-TBI, followed by oral 0.5% CMC-Na daily for 7 days; 2. TBI+P7C3: Intravenous injection of P7C3 (20 mg/kg, dissolved in PEG400+saline) 1 hour post-TBI, followed by oral P7C3 (10 mg/kg/day, dissolved in 0.5% CMC-Na) for 7 days. Neurological function was assessed via mNSS daily. On day 8, rats were euthanized, brains were collected to measure edema [4] |
| 药代性质 (ADME/PK) |
Oral bioavailability: In male Sprague-Dawley rats, oral administration of P7C3 (50 mg/kg) showed an oral bioavailability of 65% (compared to intravenous administration) [2]
- Plasma pharmacokinetics: Rats orally administered P7C3 (50 mg/kg) had a Cmax (peak plasma concentration) of 4.2 μg/mL, Tmax (time to peak) of 2.0 hours, and elimination half-life (t1/2) of 6.8 hours [2] - Tissue distribution: P7C3 crosses the blood-brain barrier (BBB), with a brain/plasma concentration ratio of 1.2 in rats 2 hours after oral administration (50 mg/kg). It distributes to other tissues (liver, kidney, heart) but accumulates most in the brain [2] |
| 毒性/毒理 (Toxicokinetics/TK) |
Chronic in vivo toxicity: Male C57BL/6 mice orally administered P7C3 (100 mg/kg/day) for 90 days showed no significant weight loss (<5% of baseline), abnormal serum ALT/AST/BUN/creatinine levels, or histopathological changes in liver, kidney, spleen, or brain [1]
- Acute in vivo toxicity: Rats orally administered P7C3 at doses up to 200 mg/kg showed no mortality or acute toxicity (e.g., lethargy, diarrhea), indicating an LD50 > 200 mg/kg [2] - Acute neurotoxicity: Mice intraperitoneally administered P7C3 (10 mg/kg/day) for 7 days (LPS model) had no changes in motor function (rotarod test) or brain tissue damage (H&E staining) [3] - TBI-related toxicity: Rats treated with P7C3 (20 mg/kg IV + 10 mg/kg oral) for 7 days post-TBI showed no significant changes in serum creatinine or brain oxidative stress markers (MDA, SOD) [4] |
| 参考文献 | |
| 其他信息 |
An in vivo screen was performed in search of chemicals capable of enhancing neuron formation in the hippocampus of adult mice. Eight of 1000 small molecules tested enhanced neuron formation in the subgranular zone of the dentate gyrus. Among these was an aminopropyl carbazole, designated P7C3, endowed with favorable pharmacological properties. In vivo studies gave evidence that P7C3 exerts its proneurogenic activity by protecting newborn neurons from apoptosis. Mice missing the gene encoding neuronal PAS domain protein 3 (NPAS3) are devoid of hippocampal neurogenesis and display malformation and electrophysiological dysfunction of the dentate gyrus. Prolonged administration of P7C3 to npas3(-/-) mice corrected these deficits by normalizing levels of apoptosis of newborn hippocampal neurons. Prolonged administration of P7C3 to aged rats also enhanced neurogenesis in the dentate gyrus, impeded neuron death, and preserved cognitive capacity as a function of terminal aging.[1]
A novel neuroprotective small molecule was discovered using a target-agnostic in vivo screen in living mice. This aminopropyl carbazole, named P7C3, is orally bioavailable, crosses the blood-brain barrier, and is non-toxic at doses several fold higher than the efficacious dose. The potency and drug-like properties of P7C3 were optimized through a medicinal chemistry campaign, providing analogues for detailed examination. Improved versions, such as (-)-P7C3-S243 and P7C3-A20, displayed neuroprotective properties in rodent models of Parkinson's disease, amyotrophic lateral sclerosis, traumatic brain injury and age-related cognitive decline. Derivatives appended with immobilizing moieties may reveal the protein targets of the P7C3 class of neuroprotective compounds. Our results indicate that unbiased, in vivo screens might provide starting points for the development of treatments for neurodegenerative diseases as well as tools to study the biology underlying these disorders.[2] Parkinson's disease (PD) is the second most common neurodegenerative disorder. Although its pathogenesis remains unclear, growing evidencce suggests that microglia-mediated neuroinflammation contributes greatly to the progression of PD. P7C3, an aminopropyl carbazole, possesses significant neuroprotective effects in several neurodegenerative disease animal models, including PD. In this study, we designed to investigate the effects of P7C3 on neuroinflammation. We showed that P7C3 specially suppressed the expression of lipopolysaccharide (LPS)-induced pro-inflammatory factors but not influenced the anti-inflammatory factors in microglia. The inhibition of the nuclear factor κB (NF-κB) signaling pathway was involved in the mechanisms of the anti-inflammatory effects by P7C3. LPS-induced activation of IκB kinase (IKK), degradation of the inhibitory κB alpha (IκBα) and nuclear translocation of NF-κB can be attenuated by the pretreatment of P7C3 in microglia. Furthermore, in LPS-treated microglia, P7C3-pretreatment decreased the toxicity of conditioned media to MES23.5 cells (a dopaminergic (DA) cell line). Most importantly, the anti-inflammatory effects of P7C3 were observed in LPS-stimulated mouse model. In general, our study demonstrates that P7C3 inhibits LPS-induced microglial activation through repressing the NF-κB pathway both in vivo and in vitro, providing a theoretical basis for P7C3 in anti-inflammation.[3] Traumatic brain injury (TBI) is a significant public health problem around the world. A promising area of research is the characterization of small, drug-like molecules that have potent clinical properties. One pharmacotherapeutic agent in particular, an aminopropyl carbazole called P7C3, was discovered using an in vivo screen to identify new agents that augmented the net magnitude of adult hippocampal neurogenesis. P7C3 greatly enhanced neurogenesis by virtue of increasing survival rates of immature neurons. The potent neuroprotective efficacy of P7C3 is likely due to enhanced nicotinamide phosphoribosyltransferase (NAMPT) activity, which supports critical cellular processes. The scaffold of P7C3 was found to have favorable pharmacokinetic properties, good bioavailability, and was nontoxic. Preclinical studies have shown that administration of the P7C3-series of neuroprotective compounds after TBI can rescue and reverse detrimental cellular events leading to improved functional recovery. In several TBI models and across multiple species, P7C3 and its analogues have produced significant neuroprotection, axonal preservation, robust increases in the net magnitude of adult neurogenesis, protection from injury-induced LTP deficits, and improvement in neurological functioning. This review will elucidate the exciting and diverse therapeutic findings of P7C3 administration in the presence of a complex and multifactorial set of cellular and molecular challenges brought forth by experimental TBI. The clinical potential and broad therapeutic applicability of P7C3 warrants much needed investigation into whether these remedial effects can be replicated in the clinic. P7C3 may serve as an important step forward in the design, understanding, and implementation of pharmacotherapies for treating patients with TBI. This article is part of the Special Issue entitled \"Novel Treatments for Traumatic Brain Injury\".[4] Mechanism of action: P7C3 exerts neuroprotective and proneurogenic effects by activating NAMPT, the rate-limiting enzyme in the salvage pathway of NAD⁺ biosynthesis. Enhanced NAMPT activity increases intracellular NAD⁺ levels, which supports ATP production, inhibits neuronal apoptosis (via SIRT1 activation), and reduces neuroinflammation (via suppressing microglial activation) [1,3] - Research applications: P7C3 is a preclinical tool compound for studying neurodegenerative diseases (Parkinson’s disease, Alzheimer’s disease), neuroinflammation, and traumatic brain injury (TBI). It has shown therapeutic potential in preclinical models by preserving neurons, promoting neurogenesis, and alleviating neurological deficits [1,3,4] - Development status: P7C3 is in preclinical research and has not been evaluated in clinical trials or approved by the FDA for therapeutic use. Its favorable oral bioavailability and BBB penetration make it a promising lead for central nervous system (CNS) disorders [2] - Chemical properties: P7C3 is a small-molecule compound with good chemical stability (stable in aqueous solution for 72 hours at 37°C) and solubility in common solvents (DMSO, PEG400, 0.5% CMC-Na) [2] |
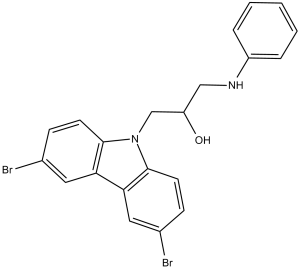
| 分子式 |
C21H18BR2N2O
|
|
|---|---|---|
| 分子量 |
474.19
|
|
| 精确质量 |
471.978
|
|
| 元素分析 |
C, 53.19; H, 3.83; Br, 33.70; N, 5.91; O, 3.37
|
|
| CAS号 |
301353-96-8
|
|
| 相关CAS号 |
P7C3-A20;1235481-90-9
|
|
| PubChem CID |
2836187
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 密度 |
1.6±0.1 g/cm3
|
|
| 沸点 |
656.4±55.0 °C at 760 mmHg
|
|
| 闪点 |
350.8±31.5 °C
|
|
| 蒸汽压 |
0.0±2.1 mmHg at 25°C
|
|
| 折射率 |
1.687
|
|
| LogP |
6.6
|
|
| tPSA |
37.19
|
|
| 氢键供体(HBD)数目 |
2
|
|
| 氢键受体(HBA)数目 |
2
|
|
| 可旋转键数目(RBC) |
5
|
|
| 重原子数目 |
26
|
|
| 分子复杂度/Complexity |
433
|
|
| 定义原子立体中心数目 |
0
|
|
| SMILES |
BrC1C([H])=C([H])C2=C(C=1[H])C1C([H])=C(C([H])=C([H])C=1N2C([H])([H])C([H])(C([H])([H])N([H])C1C([H])=C([H])C([H])=C([H])C=1[H])O[H])Br
|
|
| InChi Key |
FZHHRERIIVOATI-UHFFFAOYSA-N
|
|
| InChi Code |
InChI=1S/C21H18Br2N2O/c22-14-6-8-20-18(10-14)19-11-15(23)7-9-21(19)25(20)13-17(26)12-24-16-4-2-1-3-5-16/h1-11,17,24,26H,12-13H2
|
|
| 化学名 |
1-anilino-3-(3,6-dibromocarbazol-9-yl)propan-2-ol
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.08 mg/mL (4.39 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 20.8 mg/mL澄清DMSO储备液加入400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.08 mg/mL (4.39 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 20.8 mg/mL 澄清 DMSO 储备液加入到 900 μL 玉米油中并混合均匀。 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.1089 mL | 10.5443 mL | 21.0886 mL | |
| 5 mM | 0.4218 mL | 2.1089 mL | 4.2177 mL | |
| 10 mM | 0.2109 mL | 1.0544 mL | 2.1089 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。