| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| Other Sizes |
| 靶点 |
DNA Alkylator
|
|---|---|
| 体外研究 (In Vitro) |
孵育后,大鼠肝脏切片显示出硫代 TEPA 的烷基化活性。在 2、5 和 10 mM 的所有剂量下,thio-TEPA 不会在大鼠肝脏切片中积聚,并且对其活力没有影响[1]。
|
| 体内研究 (In Vivo) |
在前10周内,硫代TEPA(20 mg/kg,腹膜内)联合全身照射(TBI)增强了供体型血液嵌合性,但并不显着高于单独TBI组。在小鼠中,单独的 thio-TEPA 可以增强短期和长期的植入[2]。
|
| 酶活实验 |
使用精确切割的大鼠肝脏切片研究烷化剂N,N',N'-三乙烯硫代磷酰胺(thio-TEPA)的代谢。暴露于高浓度(1-10mM)硫代TEPA 6小时未证明对肝切片有毒性,这表明细胞中钾的泄漏微不足道。在孵育过程中,硫代TEPA(初始浓度,5.2微M)从缓冲液中消失的时间过程遵循一级动力学。N,N’N’-三乙烯基磷酰胺(TEPA)的形成显然是硫代TEPA消除的原因。苯巴比妥预处理大鼠可显著提高反应速率。相反,用细胞色素P-450抑制剂烯丙基异丙酰胺预处理显著降低了代谢率。硫代TEPA的消除和TEPA的形成与硫代TEPA浓度无关,其范围为5.2至104微M。硫TEPA的氧代类似物TEPA是唯一鉴定的代谢产物,没有进一步代谢。然而,在用硫代TEPA孵育肝切片后,观察到4-(硝基苄基)-吡啶(NBP)烷基化活性随时间显著增加,但在用TEPA孵育后没有。这可能表明存在未知的活性代谢物[1]。
|
| 动物实验 |
Thiotepa (TT) has long been considered for inclusion in clinical bone marrow transplant (BMT) conditioning regimens in an attempt to prevent allograft rejection and leukemia relapse. These studies have been encouraged by initial murine experiments showing a clear improvement in allogeneic bone marrow engraftment with addition of TT to total body irradiation (TBI) where it was assumed that TT enhances donor-type chimerism via ablation of competing stem cells in the recipient. The aim of the present study was to re-evaluate the hematological toxicity of TT among different stem cell subsets that included primitive cells capable of long-term repopulation and to assess how the combination of TT with TBI influences the development of donor engraftment in both syngeneic (B6-Gpi-1a --> B6-Gpi-1b) and H-2 compatible allogeneic (BALB.B10 --> B6) BMT models. At 24 h after TT (20 mg/kg) the femoral content of different stem cell subsets was determined from the frequency of transient repopulating, and the more primitive cobblestone area-forming, cells (CAFCs) growing in stroma-supported cultures. This assay showed a large TT-induced depletion (2% survival) of early clones developing at day 7 in culture but survival recovered towards normal for later appearing clones developing from more primitive CAFC subsets. The sparing of these primitive stem cells was reflected as undetectable levels of donor marrow repopulation in recipients given TT followed by syngeneic BMT. Addition of TT to TBI did not significantly improve long-term engraftment of syngeneic marrow while this combination had a dramatic effect in allogeneic BMT by preventing allograft rejection. In this respect TT shares similar properties with cyclophosphamide and suggests that the large improvement of allogeneic stem cell engraftment is attributable to the immune suppressive properties of TT rather than to its toxicity against host primitive stem cells[2].
|
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Urinary excretion of 14C-labeled thiotepa and metabolites in a 34-year old patient with metastatic carcinoma of the cecum who received a dose of 0.3 mg/kg intravenously was 63%. 446 +/- 63 mL/min [female patients (45 to 84 years) with advanced stage ovarian cancer receiving 60 mg and 80 mg thiotepa by intravenous infusion on subsequent courses given at 4-week intervals] In man, 50% of injection of (14)C-thiotepa either iv or locally into tumor was excreted in the first 6 hr and by 48 hr only low levels persisted. Absorption of orally administered dose of (14)C-thiotepa was variable: less than 1% of injected dose was recovered as unchanged drug in the urine. ... Five min after intravenous or intraarterial injection of labelled thiotepa in Sprague-Dawley rats, slightly higher levels of radioactivity were found in plasma, heart, kidneys and lungs, compared to other organs; 94-98% of radioactivity administered intravenously was excreted in urine within 8.5 hr. Most of the urinary radioactivity was associated with unchanged thiotepa; tris(l-azridinyl)phosphine oxide (tepa) was responsible for about 30% of the radioactivity. One hour after intraperitoneal injection of thiotepa at 9.3 mg/kg bw into Sprague-Dawley rats, radioactivity was found in plasma (5.4%), peritoneal fluid (26%), urine (1.9%), kidney (0.7%), liver (3.8%), lung (0.6%) and muscle (25.9%). In patients with normal renal function, thiotepa, triethylenephosphoramide (TEPA), and unidentified metabolites with alkylating activity are excreted in urine. Urinary excretion of thiotepa, TEPA, and unidentified metabolites with alkylating activity is about 0.1-1.5, 4, and 13-24% of the dose, respectively, within the first 24-48 hours; urinary excretion of the parent drug is complete within the first 6-8 hours. Fecal excretion of the drug and its metabolites has not been studied. Following IV administration of high doses of thiotepa, the drug apparently is excreted in sweat to an appreciable extent. For more Absorption, Distribution and Excretion (Complete) data for Thiotepa (14 total), please visit the HSDB record page. Metabolism / Metabolites The major urinary metabolite in rats, rabbits and dogs following a single intravenous injection of (32)P-thiotepa was tepa, which is also an alkylating agent. Most of the radioactivity in mouse urine, however, was rccovered as inorganic phosphate. ... Five min after intravenous or intraarterial injection of labelled thiotepa in Sprague-Dawley rats, slightly higher levels of radioactivity were found in plasma, heart, kidneys and lungs, compared to other organs; 94-98% of radioactivity administered intravenously was excreted in urine within 8.5 hr. Most of the urinary radioactivity was associated with unchanged thiotepa; tris(l-azridinyl)phosphine oxide (tepa) was responsible for about 30% of the radioactivity. In mice, thiotepa is rapidly metabolized to tris (1-aziridinyl)phosphine oxide (tepa): with 30 minutes only tepa and inorganic phosphate were detected in the urine and plasma. The mouse is exceptional in its ability to degrade the drug completely to inorganic phosphate. Thiotepa appears to be extensively metabolized in the liver by the cytochrome P-450 microsomal enzyme system, principally via oxidative desulfuration to a triethylenephosphoramide (TEPA). Although TEPA is the only metabolite detected and identified in plasma, there is evidence that other unidentified metabolites also are formed. Following rapid IV injection of thiotepa in adults with normal renal and hepatic function, plasma concentrations of the drug appear to decline in a biphasic manner with a half-life of approximately 6-12 minutes in the initial phase and 1.2-2.9 hours in the terminal phase. The plasma elimination half-life of TEPA is about 10-21 hours. The urinary excretion of N,N',N"-triethylenethiophosphoramide (thioTEPA), and its metabolites N,N',N"-triethylenephosphoramide (TEPA), N,N'-diethylene,N"-2-chloroethylphosphoramide (monochloroTEPA) and thioTEPA--mercapturate was determined in patients receiving thioTEPA as part of a high-dose combination chemotherapy regimen with cyclophosphamide and carboplatin. The thioTEPA dose was 40 or 60 mg/sq m in short infusions, twice daily, during 4 days. Urine samples were collected after each voiding on each day of drug administration until 24-48 h after the last thioTEPA infusion. ThioTEPA, TEPA and monochloroTEPA concentrations were determined with gas chromatography and thioTEPA--mercapturate with liquid chromatography-mass spectrometry with direct sample injection. ThioTEPA was present in urine 30 min after infusion and was still excreted 18 hr after the last infusion. All metabolites were detected in urine 1 hr after infusion. Patients with a creatinine clearance above 140 ml/minl showed higher excretion of TEPA than patients with a creatinine clearance below 140 mL/min (12.8 versus 4.9%, p=0.01). The excretion of monochloroTEPA relative to the excreted amount of TEPA increased at lower pH values of the urine. The excretion of thioTEPA--mercapturate relative to the dose was higher in patients treated with 60 mg/sq m. Excretion of thioTEPA and monochloroTEPA both accounted for only 0.5% of the dose, while TEPA and thioTEPA--mercapturate both accounted for 11.1%. Route of Elimination: Urinary excretion of 14C-labeled thiotepa and metabolites in a 34-year old patient with metastatic carcinoma of the cecum who received a dose of 0.3 mg/kg intravenously was 63%. Half Life: 1.5 to 4.1 hours Biological Half-Life 1.5 to 4.1 hours A total of 15 patients with residual ovarian cancer confined to the peritoneal cavity after first-line systemic chemotherapy were treated with thio-tepa in a phase I study. A total of 50 courses of thio-tepa were given ip in doses ranging from 30 to 80 mg/sq m. ... Peritoneal fluid concentrations declined rapidly in a first-order fashion, with a half-life of 0.96 + or - 0.1 hr. ... A biexponential decline in thiotepa concentration in plasma was seen during the first hours after intravenous injection of thiotepa at 5 mg/kg bw in Swiss-Webster mice. The half-time was 0.21 min for the first phase and 9.62 min for the second. Following rapid IV injection of thiotepa in adults with normal renal and hepatic function, plasma concentrations of the drug appear to decline in a biphasic manner with a half-life of approximately 6-12 minutes in the initial phase and 1.2-2.9 hours in the terminal phase. The plasma elimination half-life of triethylenephosphoramide (TEPA) is about 10-21 hours. |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
IDENTIFICATION AND USE: Thiotepa forms crystals or fine, white, crystalline flakes. Thiotepa is widely used in high-dose chemotherapy. HUMAN EXPOSURE AND TOXICITY: Thiotepa is known to be a human carcinogen based on sufficient evidence from studies in humans. The major adverse effect of thiotepa is hematologic toxicity, which is usually dose related and cumulative. Adverse hematopoietic effects include leukopenia, anemia, thrombocytopenia, and pancytopenia which is sometimes fatal. Hematologic status must be carefully monitored in patients receiving thiotepa. Although the leukocyte nadir may occur at 10-14 days when thiotepa is given once weekly IV, initial effects on bone marrow may not be evident for up to 30 days. Because of absorption through serous membranes, intracavitary and intravesical instillation of thiotepa can produce systemic adverse effects of varying severity; and deaths resulting from bone marrow depression secondary to systemic absorption of the drug, have occurred following intravesical instillation of the drug. ln high-dose therapy with autologous bone marrow transplantation, central nervous system disturbances, hepatic damage, infections, nausea, vomiting, diarrhea, mucositis, skin rashes, hemorrhagic cystitis and cardiomyopathy may be severe. Hematopoietic toxicity can occur following overdose, manifested by a decrease in the white cell count and/or platelets. Red blood cell count is a less accurate indicator of thiotepa toxicity. Bleeding manifestations may develop. The patient may become more vulnerable to infection, and less able to combat such infection. Dosages within and minimally above the recommended therapeutic doses have been associated with potentially life-threatening hematopoietic toxicity. Thiotepa has a toxic effect on the hematopoietic system that is dose related. Treatment with thiotepa of cultured human lymphocytes resulted in significant increase in frequency of chromosome aberrations. Thiotepa can cause fetal harm when administered to a pregnant woman. ANIMAL STUDIES: Intravitreal injection of thiotepa in rabbits at a concentration of 8 mg/mL has been reported to be tolerated without excessive inflammation or alteration of the electroretinogram. Weanling rats treated with 1:445 or 1:1000 thiotepa eyedrops during six weeks have developed corneal vascularization and cataract. Thiotepa was administered to rats at 1 mg/kg bw once weekly for 52 weeks. Malignant tumors developed in 30% treated animals; in controls, malignant tumors were found in 6% animals. Thiotepa was teratogenic in pregnant mice injected intraperitoneally with single doses of 0.5-30 mg/kg bw on various days of gestation. The minimum teratogenic dose was 1 mg/kg bw; after administration of 10 mg/kg bw all fetuses were malformed. After rats were given 5 mg/kg bw thiotepa, gross developmental abnormalities and skeletal defects were observed in fetuses. Thiotepa interfered with spermatogenesis in hamsters and mice. Thiotepa induced dominant lethal mutations, chromosomal aberrations, micronuclei and sister chromatid exchanges in rodents treated in vivo. It induced sister chromatid exchanges and chromosomal aberrations in rodent cells in vitro. It was mutagenic to Chinese hamster cells in vitro and to mouse lymphoma cells in a host-mediated assay. Thiotepa induced sex-linked recessive lethal mutations in Drosophila, caused sister chromatid exchanges and chromosomal aberrations in plant cells and was mutagenic to fungi and to bacteria in vitro and in host-mediated assays. The alkyl group is attached to the guanine base of DNA, at the number 7 nitrogen atom of the imidazole ring. They stop tumor growth by crosslinking guanine nucleobases in DNA double-helix strands, directly attacking DNA. This makes the strands unable to uncoil and separate. As this is necessary in DNA replication, the cells can no longer divide. These drugs act nonspecifically. Hepatotoxicity Thiotepa is associated with an appreciable rate of serum enzyme elevations during therapy, but these are generally mild and self-limited, not requiring dose adjustment. Rare instances of clinically apparent acute liver injury attributed to thiotepa have been reported, particularly with high doses. In most instances, thiotepa was administered in combination with other agents known to cause liver injury and the specific role of thiotepa was not clear. Thiotepa is often used in combination with other alkylating agents in conditioning regimens for bone marrow ablation in preparation for hematopoietic cell transplantation and as such has been linked to instances of sinusoidal obstruction syndrome. Onset of sinusoidal obstruction syndrome is usually within 1 to 3 weeks of myeloablative or high dose therapy and is characterized by the sudden development of abdominal pain, hepatomegaly, weight gain and ascites followed by jaundice. The pattern of serum enzyme elevations is usually hepatocellular, with marked increases in serum aminotransferase and lactic dehydrogenase levels and minimal increase in alkaline phosphatase. In severe instances, there are elevations in prothrombin time and progressive hepatic failure. Immunoallergic and autoimmune features are uncommon. The fatality rate is high. Liver biopsy shows centrolobular necrosis and congestion with occlusion of small veins and red cells in sinusoids. Likelihood score: D (possible, rare cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Most sources consider breastfeeding to be contraindicated during maternal antineoplastic drug therapy, especially alkylating agents such as thiotepa. Labeling suggests that mothers should not breastfeed during therapy and for 1 week after the last dose of thiotepa. Chemotherapy may adversely affect the normal microbiome and chemical makeup of breastmilk. Women who receive chemotherapy during pregnancy are more likely to have difficulty nursing their infant. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Interactions Methylxanthines enhance lethality of alkylating agents in human cancer cells, a phenomenon attributed to the prevention of DNA repair. Pentoxifylline is a nontoxic methylxanthine, used clinically for claudication. Using human cancer cells in culture or in a mouse xenograft model, combination treatments with alkylating agents and pentoxifylline or other methylxanthines /was examined/ With human bladder cancer cells in culture, cytotoxicity of thiotepa was increased up to ten fold (p< 0.01) by posttreatment with pentoxifylline, with a major clinical metabolite of pentoxifylline, or with caffeine; the pentoxifylline concentrations required (0.4-1.0 mM) are clinically achievable in the bladder after nontoxic po doses. With human bladder or breast cancer xenografts in a modified subrenal capsule assay, enhancement of thiotepa was also observed by in vivo posttreatment with pentoxifylline. In contrast, these combinations produce no increased toxicity to normal tissues in these animals, measured by weight, lethality, or histological changes of the normal bladder urothelium. ... Vitamin C at 2 mM enhanced sister chromatid exchange frequencies induced by thiotepa or L-ethionine in cultured human lymphocytes. However, when vitamin C was tested at 0.02 mM and 0.2 mM a rather protective effect on sister chromatid exchange rates induced by thiotepa or L-ethionine was identified. Vitamin C (2 mM) caused a cell division delay in cultures treated with thiotepa or L-ethionine. Division delays caused by thiotepa or L-ethionine were reversed in the presence of 0.02 mM or 0.2 mM vitamin C. Mitotic indices in cultures treated with thiotepa or L-ethionine continued to be suppressed in the presence of 2 mM vitamin C. However, vitamin C at 0.02 mM reversed suppression of mitotic indices caused by L-ethionine or thiotepa. These findings illustrate the complexity of the interactions of vitamin C in biological systems and indicate that with different concentrations vitamin C can cause or prevent genetic toxicity. The food components chlorophyllin, beta-carotene and alpha-linolenic acid (in its methyl ester form) were tested in Chinese hamsters for antimutagenic activity on the powerful mutagen thio-tepa. Each of these natural protective compounds inhibited by 70-85% the clastogenic effects induced by the mutagen. When 2 or 3 of these antimutagens were administered sumultaneously no additive effects were observed. alpha-Linolenic acid methyl ester was the most effective antimutagen under the experimental conditions. After receiving N,N',N"-triethylenethiophosphoramide (thiotepa) and cyclophosphamide iv, five women with metastatic adenocarcinoma of the breast developed a pattern hyperpigmentation confined to skin occluded by adhesive-containing materials. Determinations of thiotepa concentrations in occluded and nonoccluded skin, plasma, bandage with adhesive, and guaze containing sweat were performed. The results suggest that this alkylating agent is excreted onto the skin surface in sweat, accumulated beneath adhesive-containing bandages and electrocardiogram pads, and exerts a local toxic effect resulting in hyperpigmentation. Non-Human Toxicity Values LD50 Mouse iv 14,500 ug/kg LD50 Mouse sc 19,500 ug/kg LD50 Mouse oral 38 mg/kg LD50 Rat iv 9400 ug/kg LD50 Rat ip 8 mg/kg |
| 参考文献 | |
| 其他信息 |
Therapeutic Uses
Antineoplastic Agents, Alkylating; Myeloablative Agonists /CLINICAL TRIALS/ ClinicalTrials.gov is a registry and results database of publicly and privately supported clinical studies of human participants conducted around the world. The Web site is maintained by the National Library of Medicine (NLM) and the National Institutes of Health (NIH). Each ClinicalTrials.gov record presents summary information about a study protocol and includes the following: Disease or condition; Intervention (for example, the medical product, behavior, or procedure being studied); Title, description, and design of the study; Requirements for participation (eligibility criteria); Locations where the study is being conducted; Contact information for the study locations; and Links to relevant information on other health Web sites, such as NLM's MedlinePlus for patient health information and PubMed for citations and abstracts for scholarly articles in the field of medicine. Thio-tepa is included in the database. Thiotepa for Injection, USP has been tried with varying results in the palliation of a wide variety of neoplastic diseases. However, the most consistent results have been seen in the following tumors: 1. Adenocarcinoma of the breast. 2. Adenocarcinoma of the ovary. 3. For controlling intracavitary effusions secondary to diffuse or localized neoplastic diseases of various serosal cavities. 4. For the treatment of superficial papillary carcinoma of the urinary bladder. While now largely superseded by other treatments, thiotepa has been effective against other lymphomas, such as lymphosarcoma and Hodgkin's disease. /Included in US product label/ Thiotepa has been used as an ophthalmic instillation to prevent the recurrence of pterygium following surgical excision; however, postoperative beta-irradiation is generally preferred as preventive therapy because it results in a low incidence of recurrence and is relatively easy to administer. Many clinicians recommend that the use of thiotepa be limited to the management of pterygium which recurs following postoperative beta-irradiation. /NOT included in US product label/ For more Therapeutic Uses (Complete) data for Thiotepa (6 total), please visit the HSDB record page. Drug Warnings Ophthalmic instillation of thiotepa may occasionally produce irritation or periorbital skin depigmentation; the depigmentation usually occurs 6 months or longer after cessation of treatment. Intrathecal administration of thiotepa has been associated with lower extremity weakness and pain and demyelination within the spinal cord in some patients; transient paresthesia of the lower extremities also has occurred following intrathecal administration of hypertonic solutions of the drug. Other reported adverse effects of thiotepa include pain at the injection site, headache, dizziness, blurred vision, conjunctivitis, dysuria, urinary retention, amenorrhea, and tightness of the throat. Some symptoms such as hyperuricemia or febrile reactions and exudation from subcutaneous lesions may be due to breakdown of tumor tissue. In some patients, intravesical administration of thiotepa has been reported to produce lower abdominal pain, vesical irritability, hematuria, and rarely hemorrhagic chemical cystitis. Hypersensitivity reactions, including allergic reactions, rash, urticaria, laryngeal edema, asthma, anaphylactic shock, and wheezing have occurred in patients receiving thiotepa. Contact dermatitis and alopecia also have been reported. Skin depigmentation has been reported following topical use of the drug. Nausea, vomiting, abdominal pain, and anorexia occur infrequently after administration of thiotepa. Stomatitis and ulceration of the intestinal mucosa also have been reported. For more Drug Warnings (Complete) data for Thiotepa (15 total), please visit the HSDB record page. Pharmacodynamics The unstable nitrogen-carbon groups alkylate with DNA causing irrepairable DNA damage. They stop tumor growth by crosslinking guanine nucleobases in DNA double-helix strands, directly attacking DNA. This makes the strands unable to uncoil and separate. As this is necessary in DNA replication, the cells can no longer divide. These drugs act nonspecifically. |
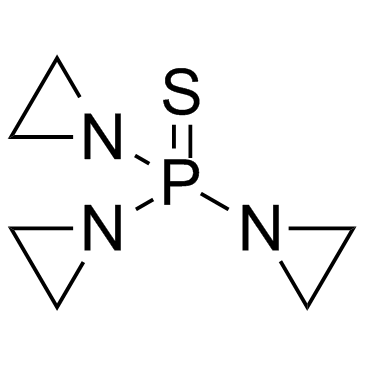
| 分子式 |
C6H12N3PS
|
|---|---|
| 分子量 |
189.2183
|
| 精确质量 |
189.048
|
| 元素分析 |
C, 38.09; H, 6.39; N, 22.21; P, 16.37; S, 16.95
|
| CAS号 |
52-24-4
|
| 相关CAS号 |
55-98-1 (Busulfan); 299-75-2 (Treosulfan)
|
| PubChem CID |
5453
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
1.5±0.1 g/cm3
|
| 沸点 |
270.2±23.0 °C at 760 mmHg
|
| 熔点 |
54-57 °C
|
| 闪点 |
117.2±22.6 °C
|
| 蒸汽压 |
0.0±0.6 mmHg at 25°C
|
| 折射率 |
1.709
|
| LogP |
0.52
|
| tPSA |
50.93
|
| 氢键供体(HBD)数目 |
0
|
| 氢键受体(HBA)数目 |
4
|
| 可旋转键数目(RBC) |
3
|
| 重原子数目 |
11
|
| 分子复杂度/Complexity |
194
|
| 定义原子立体中心数目 |
0
|
| SMILES |
S=P(N1C([H])([H])C1([H])[H])(N1C([H])([H])C1([H])[H])N1C([H])([H])C1([H])[H]
|
| InChi Key |
FOCVUCIESVLUNU-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C6H12N3PS/c11-10(7-1-2-7,8-3-4-8)9-5-6-9/h1-6H2
|
| 化学名 |
tri(aziridin-1-yl)phosphine sulfide
|
| 别名 |
NSC-6396; AI3 24916; WR45312; NSC 6396; AI324916; WR 45312; NSC6396; AI3-24916; Girostan; thiophosphoramide; thiophosphamide; THIO-TEPA; Triethylenethiophosphoramide; Thiophosphamide; Thiofozil; Tiofosfamid; triethylene thiophosphoramide. trade names: Girostan; STEPA; TESPA; Thiofozil; Thioplex; Tifosyl. Foreign brand names: Ledertepa; Oncotiotepa; Onco Tiotepa; Tespamin; Tespamine; Thiotef; TioTEF; TSPA; WR45312.
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 本产品在运输和储存过程中需避光。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : 50~100 mg/mL ( 264.24 ~528.48 mM )
Water : ~100 mg/mL Ethanol : ~100 mg/mL |
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 2.5 mg/mL (13.21 mM) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 悬浮液;超声助溶。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: 2.5 mg/mL (13.21 mM) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 悬浊液; 超声助溶。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (13.21 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 5.2849 mL | 26.4243 mL | 52.8485 mL | |
| 5 mM | 1.0570 mL | 5.2849 mL | 10.5697 mL | |
| 10 mM | 0.5285 mL | 2.6424 mL | 5.2849 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。