| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 25mg |
|
||
| 50mg |
|
||
| Other Sizes |
|
| 靶点 |
Voltage-gated sodium channels (VGSCs)
|
|---|---|
| 体外研究 (In Vitro) |
当暴露于 0.25 mM 和 1 mM 藜芦碱 24 小时时,所有细胞都会死亡 [2]。藜芦定 (0.001-100 μM) 会引发河豚毒素敏感反应 [3]。
藜芦碱/Veratridine (VTD)是一种脂溶性神经毒素,来源于百合科植物。它作为钠通道激动剂的作用已被广泛研究。然而,藜芦碱对钠通道亚型,尤其是Nav1.7的影响仍有待研究。在这里,我们研究了藜芦碱对HEK293A细胞异位表达的人Nav1.7的影响,并使用全细胞膜片钳技术记录了细胞的Nav1.7电流。我们发现藜芦碱对Nav1.7的峰值电流具有剂量依赖性的抑制作用,半数最大抑制浓度(IC50)为18.39µM。同时,藜芦碱还以剂量依赖的方式引发尾电流(线性)和持续电流[半最大浓度(EC50):9.53µM]。藜芦碱(75µM)使Nav1.7激活曲线的半最大激活电压在超极化方向上从-21.64±0.75 mV移动到-28.14±0.66 mV,并将稳态失活曲线的半失活电压从-59.39±0.39 mV移动到-73.78±0.5 mV。刺激频率的增加降低了每个脉冲的Nav1.7峰值和尾电流以及脉冲数,并增加了训练结束时的累积尾电流。这些发现揭示了藜芦碱对Nav1.7峰电流和尾电流的不同调节作用。[1] 藜芦碱/Veratridine (VTD)是一种植物神经毒素,通过阻断细胞膜的电压门控钠通道(VGSC)起作用。VTD中毒的症状包括强烈的恶心、低血压、心律失常和意识丧失。中毒的治疗主要集中在治疗症状上,这意味着没有针对VTD的特效解毒剂。在这项研究中,我们有兴趣研究VTD与环糊精(CD)的分子相互作用。CD是超分子大环,能够在疏水腔内形成主客体包合物(IC)。由于VTD是一种脂溶性生物碱,我们假设它可以与不同类型的CD形成稳定的包合物,从而改变其理化性质。在这项研究中,我们通过等温滴定量热法(ITC)和核磁共振(NMR)光谱研究了VTD与β-CD、γ-CD和磺丁基醚β-CD(SBCD)的相互作用。对接和分子动力学研究证实了包合物最稳定的构型。最后,为了了解VTD/CD分子相互作用的影响,我们对Neuro-2a细胞进行了基于细胞的检测(CBAs)。我们的研究结果表明,使用不同量的CD对细胞具有解毒剂样的浓度依赖性作用,显著提高了细胞存活率,从而为CD和VTD的应用开辟了新的研究机会。[2] 伤害感受器是背根神经节(DRG)神经元的一个亚群,用于检测伤害性刺激和发出疼痛信号藜芦碱(VTD)是一种电压门控钠通道(VGSC)调节剂,在VGSC阻断剂的功能筛选中用作“激动剂”。然而,关于DRG神经元的VTD反应特征及其与神经元亚型的关系,目前的信息很少。在这里,我们描述了培养的小鼠DRG神经元中VTD诱导的钙反应。我们的数据显示,VTD反应的异质性反映了感觉神经元的不同亚群。约70%的DRG神经元对30-100μM VTD有反应。我们根据VTD的反应形状将其分为四种类型。VTD反应谱的发生频率不同,并与神经元大小相关。此外,VTD反应谱与对痛觉标志物辣椒素、AITC和α,β-亚甲基ATP的反应相关。由于VTD反应谱整合了几类离子通道和交换器的作用,它们可以作为每个感觉神经元中表达的离子通道/交换器星座的功能“报告者”。因此,我们的发现与使用VTD激活DRG神经元的研究和筛选有关[3]。 |
| 体内研究 (In Vivo) |
本研究旨在确定藜芦碱/Veratridine (VTD)在足以诱导小鼠模型中UBXN2A表达的剂量下的安全性和有效性。一组流式细胞术实验证实,Veratridine (VTD)以剂量依赖的方式诱导早期和晚期细胞凋亡。每隔一天以0.1mg/kg的剂量(QOD)在体内腹腔内(IP)注射VTD 4周,有效地诱导了小鼠小肠和大肠中UBXN2A的表达。对VTD治疗动物的组织进行液相色谱-串联质谱(LC-MS/MS)分析,结果显示VTD浓度在低pg/mg范围内。为了解决神经和心脏毒性方面的问题,对C57BL/6NHsd小鼠进行的一套全面的行为和心血管评估表明,在接受0.1mg/kg VTD QOD 30天的动物中,VTD不会产生可检测到的神经毒性或心脏毒性。最后,在无胸腺裸鼠中进行的小鼠异种移植物实验表明,VTD可以抑制肿瘤生长。实验性肿瘤候选药物失败的主要原因是缺乏足够的安全性和有效性。本研究的结果支持VTD作为一种安全有效的抗癌分子的潜在用途[4]。
藜芦碱(VTD)在0.1 mg/kg时没有表现出向外神经毒性[4] 腹腔和皮下注射<强>藜芦碱(VTD)的LD50(致死剂量50%)分别为1.35和4.9 mg/kg。考虑到这一点,我们进行了最大耐受剂量(MTD)实验,并对C57BL/6NHsd小鼠施用0.1、0.3、0.5和1mg/kg的VTD IP。根据之前的报告,对动物进行视觉监测,以了解VTD描述的神经毒性体征和症状。正如Otoom等人所报道的那样,我们观察到随着VTD剂量的增加,神经毒性的剂量依赖性迹象。在0.1mg/kg的最低VTD剂量下,没有发现任何外部神经症状。在0.3mg/kg的剂量下,观察到持续不到一分钟的短暂冷冻状态。在0.5mg/kg的剂量下,动物表现出持续几分钟的冷冻状态,然后消失。在1mg/kg的剂量下,动物表现出严重的冷冻和呼吸窘迫,因此立即被安乐死。0.1mg/kg的剂量下没有神经毒性迹象,这与Meilman等人之前在大鼠身上报告的结果相似。 藜芦碱(VTD)诱导体内UBXN2A的表达[4] 基于MTD的结果,我们决定在动物模型中研究0.1mg/kg的VTD是否可以诱导UBXN2A的表达,这在以前只在细胞水平上显示出来。为了测试这一点,C57BL/6NHsd小鼠被给予VTD 0.1 mg/kg IP QOD或乙醇(0.01%)对照。30天后,收集小肠和大肠组织进行RNA和蛋白质研究(图2A)。图2中的结果显示,VTD治疗显著诱导了小鼠大肠组织中UBXN2A在两种RNA中的表达(图2C,平均对照 = 1, 平均VTD=2.97,N=6每次处理,P<0.05)和蛋白质(图2D,E,P<0.05,N=4/次处理)与接受乙醇载体的对照组相比。qRT-PCR显示,VTD增加了小肠中UBXN2A的RNA水平,但未达到统计学意义(图2B,平均对照 = 1, 平均VTD=11.77,有趣的是,qRT-PCR显示,包括小鼠结肠降段在内的大肠部分对VTD的反应更为均匀。因此,蛋白质印迹(WB)实验证实了UBXN2A RNA在VTD反应中显著翻译为蛋白质(图2E和表2,补充材料)。我们观察到小鼠对VTD治疗的反应存在差异,这可能是由于每只动物的药物输送/代谢存在差异。此外,结肠组织的形态异质性和样本间WB信号的非线性性质可能是这些差异的另外两个原因。我们使用GAPDH对UBXN2A信号进行归一化,以显示每只小鼠的UBXN2A水平。结果清楚地显示了单个小鼠远端结肠的异质性。进一步的研究和替代技术可以确定这些差异背后的原因。在动物模型中测试低剂量VTD证实,0.1mg/kg VTD可以有效提高小鼠结肠组织中UBXN2A的水平。 组织生物分析显示,在动物模型中没有出现严重的藜芦碱(VTD)积聚[4] 通过LC-MS/MS在1、1.5、2、4、8、12、24、48和72小时测定VTD的血浆和组织浓度。所有测试样本的血浆浓度都可以忽略不计(<0.20 ng/ml),这表明小鼠低剂量给药后VTD的系统性存在很小。组织浓度总体较低,所有研究组织中只有pg/mg浓度。脑组织中VTD浓度在8小时达到峰值,但迅速消除(图3A)。心脏浓度立即达到峰值,并在12小时内消除(图3B),所有其他样本在72小时内显示药物消除(图3C-E)。48小时时VTD浓度低(如果不是无法检测到的话)表明,除肺外,所有组织中慢性给药的药物积聚风险可以忽略不计。众所周知,肺对所有小分子药物都是天然可渗透的。未来将对肺部进行进一步的研究。本研究中VTD的清除与大鼠肝微粒体中的体外代谢测定相匹配 急性和反复接触藜芦碱(VTD)不会影响小鼠的行为[4] 行为队列的时间线如图4A所示。在任何行为测量中,藜芦碱(VTD)与对照组之间均未发现显著差异(表1,补充材料)。机车测试显示,在行驶距离(图4B)或速度(图4C)内,VTD没有影响。在行进的距离(F[3,84]=6.429;P=0.001)和速度(F[3,44]=6.403;P=0.000)方面,性别和时间点之间存在显著的相互作用,与男性相比,女性表现出更大的探索行为。这种效果是意料之中的,因为在所有形式的基于运动的测试中,女性传统上比男性表现出更多的运动探索。事后分析显示,所有组的基线和其他时间点之间以及雌性在4周时间点的行进距离和速度都有所减少。VTD对运动协调(图4D)、力量(图4E)或伤害感受(图4F)的测量没有影响。旋转杆测试发现时间点有显著影响(F(1.609,45.055)=45.378;P<0.001),事后分析显示,从基线到其他3个时间点,训练有所改善。网格悬挂测试也显示了训练效果(F[3,84]=6.046;P=0.004),在所有组中,小鼠在4周的时间点从网格中跳跃;采用Von Frey检验(F[3,84]=11.619;P<0.001),与基线相比,所有小鼠在2周和4周的时间点都习惯了刺激。在新的物体识别测试中,没有发现任何测量值有显著差异(图4G)。 藜芦碱(VTD)对心脏功能没有影响,并显示出轻微的降压作用[4] 心血管评估的时间线如图5A所示。超声的射血分数(EF)表明,VTD和对照组动物在任何时间点都没有差异(图5B)。此外,在任何时间点,心输出量(CO,图5C)、心率(HR,图5D)或每搏输出量(SV,图5E)均未检测到差异。经过4周的药物治疗后,通过t检验,任何回声参数都没有显著差异(图5F–I),通过双向方差分析,性别对HR或EF没有影响(数据未显示)。通过双向方差分析,CO(F[1,12]=9.906;P=0.008)和SV(F[1.12]=11.95;P=0.005)存在性别差异,但治疗没有效果。由于性别之间的体型差异,C57BL/6NHsd小鼠中CO和SV的性别差异很常见。 藜芦碱(VTD)可减小肿瘤大小[4] 图7显示了体内小鼠异种移植物模型的数据。将Foxn1nu小鼠皮下植入iRFP-标记的HCT-116结直肠癌癌症细胞(表3,补充材料),随后在肿瘤植入后一天开始用0.1mg/kg VTD-IP QOD或对照治疗(图7A)。在5周内每周进行3D超声以计算精确的肿瘤体积,然后进行LI-COR近红外成像以可视化VTD对原发性肿瘤生长的影响(图7B-E和补充图S1)。5周后,VTD治疗导致iRFP信号显著降低,VTD组的平均总LI-COR信号为1.68E7 a.u,对照组为4.37E7 a.u.,P=0.035(图7F)。肿瘤体积也显著减少,VTD组的平均总肿瘤体积为409.3 mm3,对照组为1117 mm3,P=0.028(图7G)。如之前在细胞水平上所示,VTD的存在导致了凋亡和坏死肿瘤的诱导。提取的异种移植物肿瘤的TUNEL染色表明,在用VTD治疗的小鼠中,VTD诱导肿瘤组织中细胞死亡,其中凋亡/坏死组织区域较大(图7H,I)。一组WB实验(补充图S2)证实,VTD处理增加了UBXN2A的蛋白质水平,同时降低了mortalin的水平,表明UBXN2A对mortalin具有负调控作用。这些数据表明,0.1mg/kg VTD QOD可以有效地起到抗生长剂的作用。 |
| 酶活实验 |
等温滴定量热法[1]
ITC使用Microcal VP-ITC等温滴定量热计在298.2 K和大气压下进行。该仪器已通过电子方式校准。这些数据是用量热科学公司提供的计算机软件获取的,并使用单点模型进行分析。通过将10µL等分试样注射到含有VTD溶液(200μM)的样品池中,将CD溶液(4 mM)分离240秒,进行VTD/CD结合实验。所有实验均在由与等温滴定量热计连接的步进电机驱动的恒定搅拌(200rpm)下进行。使用20mM pH 6 tris缓冲液制备溶液,并在滴定实验前对所有溶液进行脱气。选择实验的CD浓度是为了在每个CD的临界聚集浓度(cac)以下工作,以确保测量的焓变代表复合物的形成,而不会受到CD聚集体同时溶解的影响。在对照实验中,将10µL等分CD溶液(4 mM)注射到含有tris缓冲液的样品池中,不含VTD毒素。 核磁共振波谱[1] 1H-NMR和2D 1H-1H ROESY光谱在Varian NMR System 400中以298 K的温度在400 MHz的含DC1 0.1%(v/v)的D2O中记录,使用每种环糊精(β-CD、γ-CD或SBCD)的1:1 VTD:CD摩尔比。所有信号均参考内部HDO(4.79 ppm)。在400 ms的混合时间和1.8 s的弛豫延迟下获得了ROESY光谱。借助标准COSY和HSQC实验,在相同溶液上分配了VTD、纯CD和包合物的质子共振。 |
| 细胞实验 |
细胞毒性测定[2]
细胞类型: Neuro-2a 细胞 测试浓度: 0.25 mM 和 1 mM 孵育时间: 24 小时 实验结果:导致大约 100% 细胞死亡(0% 细胞活力)。 细胞活力测定 [3] 细胞类型:培养的小鼠 DRG 神经元 测试浓度: 0.001、0.1、1、10、 30 和 100 μM 孵育时间: 实验结果: 从阈值 1 μM 开始,响应神经元的数量以浓度依赖性方式增加。 神经-2a细胞活力实验[1] 神经-2a细胞(ATCC,CCL131)在310 K的10%胎牛血清(FBS)RPMI培养基中,在5%CO2加湿的气氛中维持。在实验中,细胞在96孔微孔板中以每孔约34000个细胞的密度在5%FBS RPMI培养基中培养24小时。在MilliQ®水中制备VTD储备溶液(1 mM),并将其调节至pH 2以溶解。在PBS中制备CD储备溶液(50 mMβ-CD、200 mMγ-CD和200 mM SBCD)。在暴露于VTD和CD之前,用0.4 mM哇巴因处理一半的微孔板。然后,将不同浓度的10μL VTD和10μL CD加入到有和没有OB处理的孔中(作为评估CD毒性的对照),并孵育24小时。每个孔的最终pH值为6。使用比色[3-(4,5-二甲基噻唑-2-基)-2,5-二苯基四唑]MTT法在三次实验中评估细胞存活率。使用自动多孔扫描分光光度计在570nm处读取吸光度值。细胞存活率值相对于未经OB处理的对照的存活率进行了归一化。 电生理学[1] 如前所述,在室温下使用EPC/10放大器和Pulse软件进行全细胞膜片钳记录,并稍作修改。细胞浸泡在由以下成分(单位为mM)组成的细胞外溶液中:150 NaCl、5 KCl、10 HEPES、2.5 CaCl2和1葡萄糖(用NaOH将pH值调节至7.4)。使用P-97拉拔器制造贴片移液管,以在填充细胞内溶液时实现2-3MΩ的电阻,细胞内溶液由以下成分组成(单位为mM):107 CsF、10 NaCl、2 MgCl2、1 CaCl2、10 HEPES、10 EGTA和10 TEACl(用CsOH将pH值调节至7.2)。电流在2.9 kHz下滤波,在10 kHz下数字化。在整个细胞记录过程中,严重的耐药性得到了70-80%的补偿。TTX以1 mM的浓度储存在水中,使用时用细胞外溶液稀释至0.5µM,藜芦碱(VTD)以75 mM的浓度存放在乙醇中,使用时使用细胞外溶液将其稀释至1-75µM。 |
| 动物实验 |
Animals and Veratridine (VTD) treatment [4]
Five different in vivo assessments were performed: maximum tolerated dose (MTD), behavioral, cardiovascular, blood/tissue concentration, and xenograft. C57BL/6NHsd mice were used for the MTD, behavioral, cardiovascular, and blood/tissue cohorts, and Foxn1nu athymic nude mice were used for the xenograft cohort. For each type of assessment, separate cohorts of mice were utilized; however, when possible and appropriate, animal data from cohorts were combined to reduce animal numbers needed. Animal numbers utilized for each set of experiments are included with their associated figure legends. All mice used in this study were housed with 3–4 animals per cage, kept at 22 °C on a standard light cycle (lights on from 10:00 to 22:00 h), and provided free access to water and standard rodent chow. All animal treatments and group assignments were randomized. Institutionally supported core facilities performed comprehensive assessments of the impact of Veratridine (VTD) on live animals. All data were collected, measured, and statistically analyzed by individuals within each facility who were blinded to animal treatment. Details about statistical methods used for each of the behavioral, cardiovascular, xenograft, and laboratory assessments can be found in Supplemental Materials. In the behavioral, cardiovascular, and xenograft cohorts, drug concentration was given to match the dose required to induce UBXN2A expression from previous experiments and the timeline/frequency of typical cancer treatment paradigms. The dose of Veratridine (VTD) was given based on mean weekly body weight (BW) by sex, and vehicle control was matched by volume. In the cardiovascular and behavioral cohorts, the mean BW of males was 26.7 ± 4.5 g and of females was 20.9 ± 2.3 g at the 4-week endpoint. In the xenograft cohort at the 5-week endpoint, the mean BW of males and females was 31.3 ± 2.6 and 26.2 ± 1.9 g, respectively. All animals were weighed at weekly intervals and monitored carefully for health. In the cardiovascular and behavioral cohorts, none of the mice exhibited weight loss at any weighing interval, and all were alive and healthy at the ~4-week endpoint. Some of the xenograft animals exhibited minor weight loss once tumors became large during the 5th week. However, all animals were active and hydrated and remained in the study until endpoint. Maximum tolerated dose (MTD) cohort [4] In the MTD cohort, we conducted a MTD experiment and administered Veratridine (VTD) IP at 0.1, 0.3, 0.5, and 1 mg/kg to C57BL/6NHsd mice. Animals were visually monitored for any signs or symptoms of neurotoxicity. Blood/tissue cohort [4] In the blood/tissue cohort, Veratridine (VTD) at 0.1 mg/kg was given by the IP route. One male and one female C57BL/6NHsd mouse aged 12–16 weeks was sacrificed at each timepoint for later bioanalysis. The timepoints were 1, 1.5, 2, 4, 8, 12, 24, 48, and 72 h after IP injection of 0.1 mg/kg Veratridine (VTD). Animals were anesthetized with isoflurane to effect and administered 10 µl of 1000IU heparin via retro-orbital intravenous injection just before euthanasia to enable the collection of unclotted blood by cardiac stick. Blood was collected and spun at 1000×g for 3 min. Plasma and tissues were collected and frozen for later bioanalysis. Tissues collected included brain, heart, kidney, spleen, and lung. Details about the bioanalyses performed can be found in Supplemental Materials. Behavioral and cardiovascular cohorts [4] Mice in the behavioral and cardiovascular cohorts received Veratridine (VTD) 0.1 mg/kg IP QOD for a total of 30 days. For the cardiovascular and behavioral cohorts, both male and female C57BL/6NHsd mice at 8–12 weeks of age were randomized into Veratridine (VTD) and control groups. For the behavioral cohort, N = 16 mice were randomized to each of the treatment groups, with equal numbers of mice for each sex. Behavioral assessments encompassed a comprehensive battery of tests to evaluate motor coordination and balance, limb strength, sensory and pain threshold, and working memory in mice during Veratridine (VTD) treatment. For the cardiovascular cohort, N = 8 mice were randomized to each of the Veratridine (VTD) and control groups, with equal numbers of each sex. Cardiovascular assessments involved weekly evaluation of cardiac function using echocardiogram followed by endpoint evaluation of arterial and intracardiac hemodynamics. A timeline of the behavioral and cardiovascular assessments can be found with their respective results figures. Detailed descriptions of the evaluations performed can be found in Supplemental Materials. Xenograft cohort [4] For the xenograft cohort, N = 12 male and female athymic nude-Foxn1nu mice at 7–8 weeks of age were randomized into each of the Veratridine (VTD) and control groups. Mice received bilateral injections of 1 × 106 iRFP-tagged HCT-116 colorectal cancer cells suspended in 200 μl Hanks’ buffer free-FBS in the subcutaneous space over each hindquarter to induce tumors. Mice were treated with Veratridine (VTD) 0.1 mg/kg IP QOD for a total of 37 days beginning the day after tumor induction. The formation and progression of tumors were monitored weekly with near-infrared fluorescent imaging using a LI-COR Classic Imager with MousePOD accessory and 3D ultrasound volume reconstructions using high-frequency ultrasound weekly beginning at 2 weeks. Tissues were collected at endpoint for downstream immunohistochemistry and biological experiments. A detailed description of the performed methods including biological and histological techniques can be found in Supplemental Materials. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
DATA GIVEN FOR LIPID SOLUBILITY, BINDING TO HUMAN ALBUMIN, & URINARY EXCRETION AFTER ORAL ADMIN TO HUMANS. STRUCTURE-ACTIVITY CORRELATIONS ARE DISCUSSED WITH RESPECT TO LIPID SOLUBILITY & PHARMACOLOGICAL PROPERTIES. |
| 毒性/毒理 (Toxicokinetics/TK) |
Interactions
THE ACTION OF VERATRIDINE ON THE RESTING MEMBRANE POTENTIAL OF INTACT CRAYFISH (PROCAMBARUS CLARKI) AXONS IN THE PRESENCE OF DIFFERENT EXTRACELLULAR ALKALINE-EARTH CATIONS WERE STUDIED USING INTRACELLULAR MICROELECTRODES. AT EXTRACELLULAR PH VALUES OF 7, 6, & 5, THE APPARENT BINDING SEQUENCE WAS CA2+ GREATER THAN OR EQUAL TO SR2+ MORE THAN MG2+ APPROX BA2+. 6280 rat LD50 intraperitoneal 3500 ug/kg LUNGS, THORAX, OR RESPIRATION: CYANOSIS; LUNGS, THORAX, OR RESPIRATION: RESPIRATORY DEPRESSION; GASTROINTESTINAL: CHANGES IN STRUCTURE OR FUNCTION OF SALIVARY GLANDS Journal of Pharmacology and Experimental Therapeutics., 78(238), 1943 6280 mouse LD50 intraperitoneal 1350 ug/kg Proceedings of the Society for Experimental Biology and Medicine., 76(847), 1951 [PMID:14844368] 6280 mouse LD50 subcutaneous 6300 ug/kg BEHAVIORAL: CONVULSIONS OR EFFECT ON SEIZURE THRESHOLD; BEHAVIORAL: ATAXIA; LUNGS, THORAX, OR RESPIRATION: CYANOSIS Journal of Pharmacology and Experimental Therapeutics., 113(89), 1955 [PMID:13234031] 6280 dog LDLo intravenous 19 mg/kg CARDIAC: ARRHYTHMIAS (INCLUDING CHANGES IN CONDUCTION) Journal of Pharmacology and Experimental Therapeutics., 120(412), 1957 [PMID:13476366] Non-Human Toxicity Excerpts Eleven alkaloids obtained from Veratrum have been compared for their effects on the membrane potential and conductances of squid and crayfish giant axons. They can be classed in three groups. 1) Veratridine, cevadine and protoveratrines A and B cause the membrane to depolarize. The potency decreases in that order, and the concentrations of veratridine and cevadine required for 50% maximum depolarization are estimated to be 3.3 x 10-5 M and 3.7 x 10-3 M, respectively. The depolarization by veratridine is due primarily to a selective increase in resting sodium permeability of time membrane and is antagonized by tetrodotoxin. All of them are effective in augmenting and prolonging the negative (depolarizing) afterpotential. 2) Veratramin, eisorubijervine, muldaimine (5-veratranine 3-beta, 11-alpha-diol-11-acetate) and 5-veratranine-3alpha-11alpha-diol (1x10-4) re capable of blocking the action potential with little or no depolarization. 5-Veratranine-3-beta, 11-alpha-diol blocks both sodium and potassium conductance increases. 3) Cyclopamine, jervine, rubijervine and veratrosine have no effect on the resting and action potentials. Possible structure-activity relationships for these effects are discussed. 1X10-4 MOLAR VERATRIDINE APPLIED EXTERNALLY TO SQUID AXON CAUSED DEPOLARIZATION OF MEMBRANE. DURING INITIAL DEPOLARIZATION, REPETITIVE AFTERDISCHARGES INITIATED BY SINGLE STIMULUS SUBSIDED AS MEMBRANE FURTHER DEPOLARIZED & ACTION POTENTIAL BLOCKED. DEPOLARIZATION IS DUE PRIMARILY TO INCR IN RESTING SODIUM PERMEABILITY OF MEMBRANE. VERATRIDINE CAUSED DEPOLARIZATION OF EXCITABLE CELLS & PRODUCED MARKED ELEVATION OF ADENOSINE 3',5'-MONOPHOSPHATE (CYCLIC AMP) & GUANOSINE 3',5'-MONOPHOSPHATE (CYCLIC GMP) LEVELS IN INCUBATED SLICES OF MOUSE CEREBRAL CORTEX. SIGNS OF POISONING WITH VERATRINE AND RELATED ALKALOIDS ARE SALIVATION, PURGATION, VOMITING (EVEN IN THE COW), DIURESIS, EXCITABILITY FOLLOWED BY PROSTRATION, WEAK AND IRREGULAR PULSE, DEEP AND SLOW RESPIRATIONS, AND DEATH IN CONVULSIONS OR CONSEQUENTLY UPON PARALYSIS. THE LETHAL DOSE OF THE FRESH ROOT IS 1 G/KG IN THE HORSE AND 2 G/KG IN THE COW. |
| 参考文献 |
|
| 其他信息 |
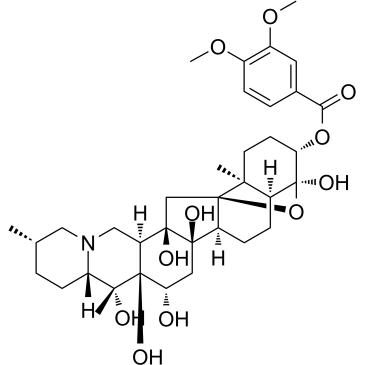
Veratridine is a steroid. It has a role as a sodium channel modulator. It is functionally related to a cevane.
A benzoate-cevane found in VERATRUM and Schoenocaulon. It activates SODIUM CHANNELS to stay open longer than normal. Mechanism of Action THE EFFECTS OF VERATRIDINE ON EXCITABLE TISSUES ARE PREDICTABLE, BASED ON ITS ABILITY TO ENHANCE SODIUM PERMEABILITY. EFFECTS INCLUDE, AMONG OTHERS, RELEASE OF NEUROTRANSMITTERS, HORMONES, DRUGS TAKEN UP BY NERVE ENDINGS, ETC. Therapeutic Uses HAS BEEN TESTED IN MYASTHENIA GRAVIS TO INCREASE MUSCLE RESPONSE TO GIVEN MOTOR NEURON STIMULATION. USED EXPERIMENTALLY TO ALTER SODIUM CHANNEL KINETICS /PRC: IN EXCITABLE MEMBRANES/ In conclusion, our study showed that Veratridine (VTD) exhibited a dose-dependent and use-dependent inhibitory effect on the peak current of Nav1.7 and shifted the activation curve and steady-state inactivation curve of Nav1.7 in the hyperpolarized direction, while enhancing the sustained current and tail current, which could contribute to the associated Na+ influx. Our study reveals a new mechanism for the modification of Nav1.7 gating by veratridine.[1] We have successfully proven the formation of inclusion complexes between the alkaloid neurotoxin Veratridine (VTD) and native β-CD and γ-CD as well as the anionic β-CD derivative SBCD. The equilibrium constants were estimated to be 1500 M−1, 7200 M−1 and 8200 M−1 for β-CD, γ-CD and SBCD, respectively, making the γ-CD and the anionic SBCD the most stable hosts. The 1H-NMR and 1H-1H ROESY experiments confirmed the incorporation of VTD in each of the CDs’ cavities and the most stable orientation of the molecule inside the CDs was elucidated by performing docking and molecular dynamics simulations. In vitro studies showed that the three studied CDs have antidote-like effects against the VTD toxicity, protecting Neuro-2a cell viability to different extent, depending on the CD type as well as the CD and VTD concentrations. To the best of our knowledge, this is the first study of the interactions between the VTD neurotoxin and CDs and opens the door to further studying of the role of CDs with other lipid toxins.[2] In conclusion, the present study shows that Veratridine (VTD) induces calcium responses with heterogeneous profiles in TTX-S rich sensory neurons. VTD response profiles reflect distinct subpopulations of sensory neurons. These subpopulations overlap but are not identical to the subpopulations identified by classical functional nociceptive markers, Fig. 7. The OS and RD profiles are particularly enriched in nociceptors (neurons sensitive to at least one of the three agonists), while the SD profile is enriched in non-nociceptors (neurons insensitive to any of the three agonists). Our findings provide a detailed characterisation of VTD action on the different subsets of DRG neurons. Our work is relevant to studies and screens using VTD to activate DRG neurons.[3] A high-throughput drug screen revealed that veratridine (VTD), a natural plant alkaloid, induces expression of the anti-cancer protein UBXN2A in colon cancer cells. UBXN2A suppresses mortalin, a heat shock protein, with dominant roles in cancer development including epithelial-mesenchymal transition (EMT), cancer cell stemness, drug resistance, and apoptosis. VTD-dependent expression of UBXN2A leads to the deactivation of mortalin in colon cancer cells, making VTD a potential targeted therapy in malignant tumors with high levels of mortalin. VTD was used clinically for the treatment of hypertension in decades past. However, the discovery of newer antihypertensive drugs and concerns over potential neuro- and cardiotoxicity ended the use of VTD for this purpose. [4] |
| 分子式 |
C36H51NO11
|
|---|---|
| 分子量 |
673.79024
|
| 精确质量 |
673.346
|
| 元素分析 |
C, 64.17; H, 7.63; N, 2.08; O, 26.12
|
| CAS号 |
71-62-5
|
| PubChem CID |
6280
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
1.45 g/cm3
|
| 沸点 |
814.5ºC at 760 mmHg
|
| 熔点 |
180ºC
|
| 闪点 |
446.4ºC
|
| 折射率 |
1.663
|
| LogP |
1.293
|
| tPSA |
178.61
|
| 氢键供体(HBD)数目 |
6
|
| 氢键受体(HBA)数目 |
12
|
| 可旋转键数目(RBC) |
5
|
| 重原子数目 |
48
|
| 分子复杂度/Complexity |
1340
|
| 定义原子立体中心数目 |
14
|
| SMILES |
C[C@H]1CC[C@H]2[C@](C)([C@@]3([C@@H](CN2C1)[C@@]4(C[C@]56[C@@H](CC[C@H]7[C@]6(C)CC[C@@H]([C@@]7(O)O5)OC(=O)C8=CC(=C(C=C8)OC)OC)[C@@]4(C[C@@H]3O)O)O)O)O
|
| InChi Key |
FVECELJHCSPHKY-YFUMOZOISA-N
|
| InChi Code |
InChI=1S/C36H51NO11/c1-19-6-11-26-31(3,40)35(43)25(17-37(26)16-19)33(42)18-34-24(32(33,41)15-27(35)38)10-9-23-30(34,2)13-12-28(36(23,44)48-34)47-29(39)20-7-8-21(45-4)22(14-20)46-5/h7-8,14,19,23-28,38,40-44H,6,9-13,15-18H2,1-5H3/t19-,23-,24-,25-,26-,27-,28-,30-,31+,32+,33+,34+,35-,36-/m0/s1
|
| 化学名 |
[(1R,2S,6S,9S,10R,11S,12S,14R,15S,18S,19S,22S,23S,25R)-1,10,11,12,14,23-hexahydroxy-6,10,19-trimethyl-24-oxa-4-azaheptacyclo[12.12.0.02,11.04,9.015,25.018,23.019,25]hexacosan-22-yl] 3,4-dimethoxybenzoate
|
| 别名 |
NSC-7524; veratridine; 71-62-5; veratridin; 3-Veratroylveracevine; Veratrine (amorphous); Veratrine (amorphous) (VAN); CHEBI:28051; HSDB 4078; NSC7524; NSC 7524; Veratridine
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ~100 mg/mL (~148.41 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (3.71 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (3.71 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (3.71 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.4841 mL | 7.4207 mL | 14.8414 mL | |
| 5 mM | 0.2968 mL | 1.4841 mL | 2.9683 mL | |
| 10 mM | 0.1484 mL | 0.7421 mL | 1.4841 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。