| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg | |||
| 100mg | |||
| 250mg | |||
| Other Sizes |
| 靶点 |
5-HT1A Receptor
|
|---|---|
| 体外研究 (In Vitro) |
Vilazodone 对人 5-HT1A 受体的 IC50 为 0.2 nM,对 SERT 的 IC50 为 0.5 nM。 Vilazodone 优先与人 5-HT1A 受体的高激动剂亲和力状态结合,并且对人重组体以及大鼠、豚鼠、小鼠和狨猴天然组织 5-HT1A 受体表现出高亲和力 (pKi≥9.3)。 Vilazodone 是 5-HT1A 受体的高效部分激动剂。在表达 h5-HT1A 受体的 Sf9 细胞中的 [35S]GTPγS 结合研究中,单一浓度的维拉佐酮 (100nM) 可使基础结合增加约 70%,而基础结合是完全 5-HT1A 受体激动剂 8-OH-PIPAT 产生的。在大鼠海马膜的 [35S]GTPγS 结合研究中,Vilazodone 是一种有效的 5-HT1A 受体部分激动剂,pEC50 为 8.1,内在活性为 0.61。 Vilazodone 在大鼠和豚鼠皮层中充当有效的 5-HT 再摄取抑制剂。在表达人 SERT 的 LLCPK 细胞中,维拉佐酮抑制 [3H]5-HT 摄取,pIC50 为 8.8[1]。
|
| 体内研究 (In Vivo) |
在体内微透析研究中,维拉佐酮(腹膜内注射;3 mg/kg;单剂量)可增加大鼠额叶皮层 (FC) 和腹侧海马 (vHipp) 的细胞外 5-HT 水平。在 3 mg/kg 时观察到最大增加,FC 和 vHipp 分别达到注射前基线值的 527% 和 558%[2]。维拉佐酮(口服强饲;55 mg/kg;单剂量)在给药后 120 和 210 分钟的大鼠超声发声测试中抑制应激诱导的发声[2]。
|
| 酶活实验 |
维拉唑酮的受体结合谱由Heinrich等人报道。维拉唑酮对人5‐HT1A受体的IC50为0.2 nM,对SERT的IC50为0.5 nM。在这些研究中,其最接近的交叉亲和性是多巴胺D3受体(IC50为71 nM),其次是5‐HT4受体(IC50为252 nM)。我们使用5‐HT1A受体激动剂[3H]8‐OH‐DPAT进行的内部放射性配体结合研究表明,维拉唑酮对人重组体和大鼠、豚鼠、小鼠和狨猴的天然组织5‐HT1A受体具有高亲和力(pKi≥9.3)(未发表的数据见表1)。相比之下,维拉唑酮取代了拮抗剂放射性配体[3H]WAY100635。(在Gpp(NH)p存在的情况下)与pKi值比使用[3H]8‐OH‐DPAT获得的值低2个log单位(表2)。这些数据表明,维拉唑酮优先结合人类5‐HT1A受体的高激动剂亲和力状态,表明该分子具有部分激动剂活性。据报道,用[3H]8‐OH‐DPAT和[3H]WAY100635测定的化合物对5‐HT1A受体的亲和力差异与其内在激动剂活性成正比。因此,考虑到对[3H]8‐OH‐DPAT cf. [3H]WAY100635测定的亲和力差异与内源性激动剂5‐HT观察到的相似,这些数据表明维拉唑酮将作为5‐HT1A受体的高效部分激动剂。这一假设在表达h5‐HT1A受体的Sf9细胞中得到了[35S] gtp - γ - s结合研究的支持,其中单一浓度的维拉唑酮(100nM)使基础结合增加了约70%的5‐HT1A受体激动剂8‐OH‐PIPAT产生的基础结合。然而,由于本研究仅使用单一浓度,因此无法准确测定h5‐HT1A受体的内在活性或功能效力。此后,对表达h5‐HT1A受体的HEK细胞进行了更广泛的研究(未发表的数据)。在这些研究中,维拉唑酮作为完全激动剂,与5‐HT相比,pEC50为9.0 [1]。
相比之下,5-HT1A/B/D受体部分激动剂SB-272183((5-氯- 2,3 -二氢-6-[4-甲基哌嗪-1-酰基]-1[4-吡啶-4-酰基]napth-1-ylaminocarbonyl]- 1h -吲哚),已被报道作为啮齿动物和人类天然组织5-HT1A受体的5-HT1A受体拮抗剂,在同一研究中显示出约0.3的内在活性(图2)。在[35S]大鼠海马膜GTPγS结合研究(5-HT1A受体占主导地位的功能性制剂)中,维拉唑酮作为一种有效的5-HT1A受体部分激动剂,其pEC50为8.1,内在活性为0.61。相比而言,(±)8-OH-DPAT (pEC50 7.2)产生的部分激动剂反应的内在活性为0.45,部分激动剂丁螺环酮的pEC50= 6.5±0.35,内在活性为0.19。综上所述,这些数据表明维拉唑酮在体内可能是一种高效的5-HT1A受体部分激动剂。重组和天然组织系统内在活性的明显差异可能是受体储备程度不同的结果。事实上,据报道,体内的天然组织体树突5-HT1A自受体存在受体储备[49],但体外的天然突触后5-HT1A受体不存在受体储备,这可以解释为什么维拉唑酮在海马中表现出部分激动剂特性。因此,一个可能的结论是,维拉唑酮是一种5-HT1A受体部分激动剂,在具有高受体储备和/或提高受体- g蛋白偶联效率的系统中具有作为完全激动剂的潜力。在一些体内模型中,维拉唑酮似乎对突触前5-HT1A受体比突触后5-HT1A受体具有更高的疗效,这一观察结果支持了这一概念,但可能与一些神经化学观察结果相矛盾。[1] 生化和电生理研究表明,维拉唑酮在大鼠和豚鼠皮层中是一种有效的5-羟色胺再摄取抑制剂。我们已经在表达人SERT的LLCPK细胞中证实了这种高效能,维拉唑酮抑制[3H]5-羟色胺摄取的pIC50值为8.8±0.05(图3)。该效价值比氟西汀高约1个对数单位,但与帕罗西汀相似(未发表的观察结果)。这些数据,加上维拉唑酮是一种有效的5-HT1A受体部分激动剂的观察结果,将这种分子置于一类新的化合物中,这种化合物有可能通过5-HT1A受体激动作用直接或间接通过SERT抑制内源性5-HT的升高而迅速脱敏5-HT1A自受体。[1] |
| 动物实验 |
Efficacy in Models of Anxiety[1]
Three separate studies have evaluated the efficacy of vilazodone in various rodent models thought to be predictive of anxiolytic activity. In the rat ultrasonic vocalizations test, stress-induced vocalizations were inhibited by vilazodone (55 mg/kg po) at 120 and 210 min post dose. In comparison, 8-OH-DPAT (0.55 mg/kg sc) produced a similar, but shorter duration, activity that was reversed by WAY 100635. In contrast, the SSRI fluoxetine (100 mg/kg po) was without effect unless combined with 8-OH-DPAT. Together these data suggest that the vilazodone-mediated efficacy in this model was via its 5-HT1A receptor agonist activity. In two further rat models of anxiety, that is, the elevated plus maze and the shock-probe burying tests, vilazodone demonstrated dose related efficacy (10–40 mg/kg ip) in the shock probe test but, interestingly, was without effect in the elevated plus maze. The positive control diazepam produced efficacy in both paradigms. Finally, vilazodone was examined in a predator-induced stress paradigm, brought about by unprotected exposure to a domestic cat. Predator stress increased anxiety-like behaviors in the elevated plus maze and an increased response to an acoustic startle. Vilazodone (20–40 mg/kg ip), administered acutely or prophylactically (1 week prior to behavioral testing), attenuated stress-induced potentiated startle but had no effect on stress potentiated anxiety response in the elevated plus maze. Interestingly, a lower dose of 10 mg/kg of vilazodone had the opposite effect in the startle response, indicating a somewhat unexplained bidirectional effect, and all doses produced a potentiation of the startle-induced stress response possibly suggestive of an anxiogenic-like response. Finally, the data from these studies also showed that vilazodone had neither sedation nor stimulatory effects but did produce context-dependent efficacy. Efficacy in Models of Antidepressant Activity[1] The FST is widely used to assess the potential of molecules to exhibit an antidepressant profile since all major classes of antidepressant drugs, including tricyclic antidepressants (TCA), SNRI and SSRI, monoamine oxidase inhibitors, and atypical ADs [70–74], are effective in this stress based model. Page et al.demonstrated that vilazodone produced efficacy (i.e., a reduction in immobility time) in both the rat and mouse versions of this model at a single dose (1 mg/kg ip), whilst higher doses (3 and 10 mg/kg) were without effect. The magnitude of this efficacy was approximately similar to that of fluoxetine. Efficacy in this model is generally considered to be mediated by 5-HT and blocked by receptor antagonists and genetic deletions of 5-HT1A receptors. Thus vilazodone-mediated efficacy may be via direct 5-HT1A receptor agonism or alternatively indirect through elevations in endogenous 5-HT. Perhaps the major driving force behind this mechanistic combination of these two activities is a hastened desensitization of 5-HT1A receptors leading to an enhanced onset of therapeutic activity. Therefore some evaluation of the onset of preclinical efficacy in models thought to mimic this, such as rodent social interaction or schedule induced polydipsia, would be useful but unfortunately has not been reported to date. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Vilazodone's bioavailability is 72% when taken with food. 1% of the dose is recovered unchanged in the urine and 2% of the dose is recovered unchanged in the feces. Vilazodone's volume of distribution is unknown but large Clearance of vilazodone is 19.9-25.1L/h in patients with mild to moderate renal impairment compared to 26.4-26.9L/h in healthy controls. Vilazodone concentrations peak at a median of 4-5 hours (Tmax) after administration and decline with a terminal half-life of approximately 25 hours. The absolute bioavailability of vilazodone is 72% with food. Administration of VIIBRYD with food (high fat or light meal) increases oral bioavailability (Cmax increased by approximately 147-160%, and AUC increased by approximately 64-85%). Vilazodone is widely distributed and approximately 96-99% protein-bound. Vilazodone is excreted into the milk of lactating rats. Metabolism / Metabolites Vilazodone is mainly metabolized by cytochrome P450(CYP)3A4 and also to a minor extent by CYP2C19 and CYP 2D6. Although the metabolic pathway for vilazodone has not been fully studied, a proposed mechanism for metabolism in rats was published in 2017. Viibryd is extensively metabolized through CYP and non-CYP pathways (possibly by carboxylesterase), with only 1% of the dose recovered in the urine and 2% of the dose recovered in the feces as unchanged vilazodone. CYP3A4 is primarily responsible for its metabolism among CYP pathways, with minor contributions from CYP2C19 and CYP2D6. In vitro studies with human microsomes and human hepatocytes indicate that vilazodone is unlikely to inhibit or induce the metabolism of other CYP (except for CYP2C8) substrates; and an in vivo study with probe substrates for CYP2C19, 2D6 and 3A4 showed vilazodone did not alter the pharmacokinetics of the probe substrates. However, an in vivo study with probe substrate for CYP2C19 demonstrated a minor induction of CYP2C19. Strong inhibitors of CYP3A4 (e.g., ketoconazole) can reduce the metabolism of vilazodone in vivo and increase exposure. Conversely, strong inducers of CYP3A4 (e.g., carbamazepine) can decrease vilazodone exposure. Biological Half-Life 25 hours. Other studies show a half life of 24±5.2h with a single 40mg dose and 28.9±3.2h with repeated doses. Vilazodone /has/ a terminal half-life of approximately 25 hours. |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
IDENTIFICATION AND USE: Vilazodone is a white to off-white solid that is formulated into film-coated tablets. Vilazodone is a combined selective serotonin-reuptake inhibitor and serotonin type 1-A (5-hydroxytryptamine (5-HT1A) receptor partial agonist. It is used for the treatment of major depressive disorder in adults. HUMAN EXPOSURE AND TOXICITY: In clinical trials toxic effects of vilazodone at 200-280 mg included serotonin syndrome, lethargy, restlessness, hallucinations, and disorientation. Serotonin syndrome, a potentially life-threatening toxicity has also been reported at therapeutic doses. Serotonin syndrome symptoms may include mental status changes (agitation, hallucinations, delirium, and coma), autonomic instability (tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and/or gastrointestinal symptoms (nausea, vomiting, diarrhea). While serotonin syndrome has been reported during vilazodone monotherapy, it is a particular concern when used with other serotonergic drugs and with drugs that impair metabolism of serotonin (in particular, monamine oxidase inhibitors (MAOIs). The concomitant use of vilazdone with MAOIs intended to treat psychiatric disorders is contraindicated. Vilazodone is also not approved for use in pediatric patients. Pooled analyses of short-term placebo-controlled studies of antidepressant drugs (selective serotonin reuptake inhibitors and others) showed that these drugs increase the risk of suicidal thinking and behavior in children, adolescents, and young adults with major depressive disorder and other psychiatric disorders. Also, some neonates exposed to serotonegic antidepressants (including vilazodone) late in the third trimester of pregnancy have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding. Such complications can arise immediately upon delivery. Reported clinical findings have included respiratory distress, cyanosis, apnea, seizures, temperature instability, feeding difficulty, vomiting, hypoglycemia, hypotonia, hypertonia, hyperreflexia, tremor, jitteriness, irritability, and constant crying. In some cases, the clinical picture is consistent with serotonin syndrome. Infants exposed to vilazodone in pregnancy may also have an increased risk for persistent pulmonary hypertension of the newborn, a rare heart and lung condition associated with substantial neonatal morbidity and mortality. ANIMAL STUDIES: Vilazodone caused some developmental toxicity in rats, but was not teratogenic in rats or rabbits. When vilazodone was administered to pregnant rats at an oral dose of 30 times the maximum recommended human dose during the period of organogenesis and throughout pregnancy and lactation, the number of live born pups was decreased. There was an increase in early postnatal pup mortality, and among surviving pups there was decreased body weight, delayed maturation, and decreased fertility in adulthood. There was some maternal toxicity at this dose. Interactions Concomitant administration of vilazodone and moderate CYP3A4 inhibitors (e.g., erythromycin) can result in increased plasma vilazodone concentrations. During concurrent administration with moderate inhibitors of CYP3A4 (e.g., erythromycin), the dosage of vilazodone should be reduced to 20 mg once daily in patients experiencing intolerable adverse effects. Concomitant administration of vilazodone and potent CYP3A4 inhibitors (e.g., clarithromycin, ketoconazole) can increase plasma vilazodone concentrations by approximately 50%. The manufacturer states that the dosage of vilazodone should be reduced to 20 mg once daily if administered concomitantly with a potent CYP3A4 inhibitor. Potentially serious, sometimes fatal adverse reactions may occur in patients who are receiving or have recently received a monoamine oxidase (MAO) inhibitor and then initiate therapy with antidepressant(s) that are pharmacologically similar to vilazodone (e.g., SSRIs), or in those who received SSRI therapy shortly before initiation of an MAO inhibitor. Concomitant use of MAO inhibitors with vilazodone is contraindicated. In addition, at least 2 weeks should elapse between discontinuance of an MAO inhibitor and initiation of vilazodone and vice versa. Linezolid, an anti-infective agent that is also a reversible MAO inhibitor, has been associated with drug interactions resulting in serotonin syndrome, including some associated with SSRIs. Because of this potential risk, linezolid generally should not be used in patients receiving vilazodone. While the US Food and Drug Administration (FDA) has not received reports of serotonin syndrome with concomitant use of linezolid and vilazodone to date, the risk is considered comparable to that with SSRIs. However, the FDA states that certain life-threatening or urgent situations may necessitate immediate linezolid treatment in a patient receiving a serotonergic drug. In such emergency situations, the availability of alternative anti-infectives should be considered and the benefits of linezolid should be weighed against the risk of serotonin syndrome. If linezolid is indicated in such emergency situations, vilazodone must be immediately discontinued and the patient monitored for symptoms of CNS toxicity for 2 weeks or until 24 hours after the last linezolid dose, whichever comes first. Treatment with vilazodone may be resumed 24 hours after the last linezolid dose. If nonemergency use of linezolid is being planned for a patient receiving vilazodone, vilazodone should be withheld for at least 2 weeks prior to initiating linezolid. Treatment with vilazodone should not be initiated in a patient receiving linezolid; when necessary, vilazodone may be started 24 hours after the last linezolid dose. For more Interactions (Complete) data for Vilazodone (13 total), please visit the HSDB record page. |
| 参考文献 |
|
| 其他信息 |
Therapeutic Uses
Antidepressant Viibryd is indicated for the treatment of major depressive disorder (MDD). The efficacy of Viibryd was established in two 8-week, randomized, double-blind, placebo-controlled trials in adult patients with a diagnosis of MDD. Major depressive disorder consists of one or more major depressive episodes. A major depressive episode (DSM-IV-TR) implies a prominent and relatively persistent (nearly every day for at least 2 weeks) depressed or dysphoric mood that usually interferes with daily functioning, and includes at least 5 of the following 9 symptoms: depressed mood, loss of interest in usual activities, significant change in weight and/or appetite, insomnia or hypersomnia, psychomotor agitation or retardation, increased fatigue, feelings of guilt or worthlessness, slowed thinking or impaired concentration, or a suicide attempt or suicidal ideation. /Included in US product label/ EXPL THER Sexual dysfunction is common in major depressive disorder (MDD), and many serotonergic antidepressants adversely affect sexual function. Vilazodone, a novel serotonin (5-HT) reuptake inhibitor and 5-HT1A partial agonist approved for MDD, exerts its effects at the 5-HT transporter and at both presynaptic and postsynaptic 5-HT1A receptors. This mechanism may limit sexual dysfunction. AIM: To summarize effects of vilazodone (40 mg/day, with food) on sexual function in adults with MDD, /data was used from/ three Phase III studies: two 8-week, placebo-controlled studies and a 52-week open-label study . Sexual function was assessed by analyzing changes from baseline to end of treatment (EOT) using validated measures. Population included 869 patients (vilazodone, 436; placebo, 433) from placebo-controlled studies and 599 patients from the open-label study. Sexual dysfunction prevalence was high (50%, men; 68%, women) before treatment and declined during treatment in vilazodone and placebo groups, indicating improvement on average. At EOT, stable/improved sexual function was observed in > or = 91% of patients in placebo-controlled studies; treatment group differences in sexual dysfunction at EOT were not statistically significant for either sex. Differences vs. placebo in changes from baseline of sexual function scores were small and were generally not statistically significant; effect sizes (Cohen's D) were generally of low magnitude. In the placebo-controlled studies, 8.0% of vilazodone-treated patients and 0.9% of placebo-treated patients reported > or = 1 sexual-function-related treatment-emergent adverse event (P<0.001). Half of men and two thirds of women with MDD had sexual dysfunction at baseline; sexual function improved on average in both vilazodone and placebo groups. Results suggest that vilazodone may have a small adverse impact on sexual function in adults with MDD relative to the high prevalence of sexual dysfunction at baseline. Drug Warnings /BOXED WARNING/ WARNING: SUICIDAL THOUGHTS AND BEHAVIORS. Antidepressants increased the risk of suicidal thoughts and behavior in children, adolescents, and young adults in short-term studies. These studies did not show an increase in the risk of suicidal thoughts and behavior with antidepressant use in patients over age 24; there was a reduction in risk with antidepressant use in patients aged 65 and older. In patients of all ages who are started on antidepressant therapy, monitor closely for clinical worsening and for emergence of suicidal thoughts and behaviors. Advise families and caregivers of the need for close observation and communication with the prescriber. Viibryd is not approved for use in pediatric patients. Worsening of depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior may occur in both adult and pediatric patients with major depressive disorder or other psychiatric disorders, whether or not they are taking antidepressants. This risk may persist until clinically important remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. However, there has been a long-standing concern that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term, placebo-controlled studies of antidepressants (i.e., selective serotonin-reuptake inhibitors (SSRIs) and other antidepressants) have shown an increased risk of suicidality in children, adolescents, and young adults (18-24 years of age) with major depressive disorder and other psychiatric disorders. An increased suicidality risk was not demonstrated with antidepressants compared with placebo in adults older than 24 years of age, and a reduced risk was observed in adults 65 years of age or older. The US Food and Drug Administration (FDA) recommends that all patients being treated with antidepressants for any indication be appropriately monitored and closely observed for clinical worsening, suicidality, and unusual changes in behavior, particularly during initiation of therapy (i.e., the first few months) and during periods of dosage adjustments. Families and caregivers of patients being treated with antidepressants for major depressive disorder or other indications, both psychiatric and nonpsychiatric, also should be advised to monitor patients on a daily basis for the emergence of agitation, irritability, or unusual changes in behavior as well as the emergence of suicidality, and to report such symptoms immediately to a health-care provider. Although a causal relationship between the emergence of symptoms such as anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia, hypomania, and/or mania and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality. Consequently, consideration should be given to changing the therapeutic regimen or discontinuing therapy in patients whose depression is persistently worse or in patients experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, particularly if such manifestations are severe, abrupt in onset, or were not part of the patient's presenting symptoms. If a decision is made to discontinue therapy, vilazodone dosage should be tapered as rapidly as is feasible but consideration should be given to the risks of abrupt discontinuance. FDA also recommends that the drugs be prescribed in the smallest quantity consistent with good patient management, in order to reduce the risk of overdosage. Potentially life-threatening serotonin syndrome or neuroleptic malignant syndrome (NMS)-like reactions have been reported with antidepressants alone, but particularly with concurrent use of other serotonergic drugs (including serotonin (5-hydroxytryptamine; 5-HT) type 1 receptor agonists (triptans)), drugs that impair the metabolism of serotonin (e.g., MAO inhibitors), or antipsychotics or other dopamine antagonists. Manifestations of serotonin syndrome may include mental status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile blood pressure, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination), and/or GI symptoms (e.g., nausea, vomiting, diarrhea). In its most severe form, serotonin syndrome may resemble NMS, which is characterized by hyperthermia, muscle rigidity, autonomic instability with possible rapid fluctuation in vital signs, and mental status changes. Patients receiving vilazodone should be monitored for the development of serotonin syndrome or NMS-like signs and symptoms. Concurrent or recent (i.e., within 2 weeks) therapy with MAO inhibitors intended to treat depression is contraindicated. If concurrent therapy with vilazodone and a 5-HT1 receptor agonist (triptan) is clinically warranted, the patient should be observed carefully, particularly during initiation of therapy, when dosage is increased, or when another serotonergic agent is initiated. Concomitant use of vilazodone and serotonin precursors (e.g., tryptophan) is not recommended. If signs and symptoms of serotonin syndrome or NMS occur, treatment with vilazodone and any concurrently administered serotonergic or antidopaminergic agents, including antipsychotic agents, should be immediately discontinued and supportive and symptomatic treatment initiated. Infants exposed to selective serotonin-reuptake inhibitors (SSRIs) in pregnancy may have an increased risk for persistent pulmonary hypertension of the newborn (PPHN). PPHN occurs in 1-2 per 1,000 live births in the general population and is associated with substantial neonatal morbidity and mortality. Several recent epidemiologic studies suggest a positive statistical association between SSRI use (including Viibryd) in pregnancy and PPHN. Other studies do not show a significant statistical association. For more Drug Warnings (Complete) data for Vilazodone (16 total), please visit the HSDB record page. Pharmacodynamics Vilazodone increases serotonin levels in the brain by inhibiting the reuptake of serotonin while acting as a partial agonist on serotonin-1A receptors. Due to this activity vilazodone has sometimes been referred to as a selective partial agonist and reuptake inhibitor (SPARI). |
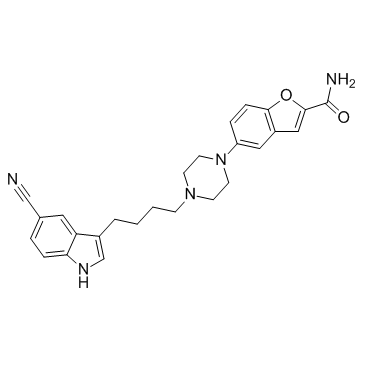
| 分子式 |
C₂₆H₂₇N₅O₂
|
|---|---|
| 分子量 |
441.52
|
| 精确质量 |
441.22
|
| CAS号 |
163521-12-8
|
| 相关CAS号 |
Vilazodone Hydrochloride; 163521-08-2; Vilazodone-d8; 1794789-93-7; Vilazodone carboxylic acid; 163521-19-5
|
| PubChem CID |
6918314
|
| 外观&性状 |
White to light yellow solid powder
|
| 密度 |
1.34 g/cm3
|
| 沸点 |
745.1ºC at 760 mmHg
|
| 熔点 |
203-205ºC
|
| LogP |
5.534
|
| tPSA |
102.29
|
| 氢键供体(HBD)数目 |
2
|
| 氢键受体(HBA)数目 |
5
|
| 可旋转键数目(RBC) |
7
|
| 重原子数目 |
33
|
| 分子复杂度/Complexity |
729
|
| 定义原子立体中心数目 |
0
|
| InChi Key |
SGEGOXDYSFKCPT-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C26H27N5O2/c27-16-18-4-6-23-22(13-18)19(17-29-23)3-1-2-8-30-9-11-31(12-10-30)21-5-7-24-20(14-21)15-25(33-24)26(28)32/h4-7,13-15,17,29H,1-3,8-12H2,(H2,28,32)
|
| 化学名 |
5-[4-[4-(5-cyano-1H-indol-3-yl)butyl]piperazin-1-yl]-1-benzofuran-2-carboxamide
|
| 别名 |
EMD 68843; SB659746A; 5-(4-(4-(5-Cyano-1H-indol-3-yl)butyl)piperazin-1-yl)benzofuran-2-carboxamide; Viibryd; EMD 515259; vilazodona; vilazodonum; UNII-S239O2OOV3; Vilazodone; EMD68843; EMD-68843
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO: 75~88 mg/mL (199.3~169.9 mM)
Ethanol: ~14 mg/mL |
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (5.66 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (5.66 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL 澄清 DMSO 储备液加入到 900 μL 玉米油中并混合均匀。 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.2649 mL | 11.3245 mL | 22.6490 mL | |
| 5 mM | 0.4530 mL | 2.2649 mL | 4.5298 mL | |
| 10 mM | 0.2265 mL | 1.1325 mL | 2.2649 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT05948579 | Not yet recruiting | Drug: Intervention B Vilazodone Hydrochloride (HCl) Drug: Intervention B Placebo |
Post Traumatic Stress Disorder | U.S. Army Medical Research and Development Command |
August 2023 | Phase 2 |
| NCT05422612 | Recruiting | Drug: Intervention A Placebo Drug: Intervention B Placebo |
Post Traumatic Stress Disorder | U.S. Army Medical Research and Development Command |
November 2, 2023 | Phase 2 |
| NCT02015546 | Completed | Drug: Vilazodone | Major Depressive Disorder (MDD) |
Duke University | December 2012 | Phase 3 |
| NCT02436239 | Completed | Drug: Vilazodone | Major Depressive Disorder | Forest Laboratories | May 2, 2015 | Phase 3 |
| NCT01828515 | Completed | Drug: Vilazodone Drug: Placebo |
Memory Impairment | University of Texas Southwestern Medical Center |
December 2012 | Phase 2 |