| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g | |||
| Other Sizes |
| 靶点 |
HIV protease (Ki = 2.66 nM)
|
|---|---|
| 体外研究 (In Vitro) |
体外活性:Atazanavir 在病毒感染的 H9 细胞中抑制病毒 gag 前体 p55 多蛋白的蛋白水解裂解,IC50 约为 47 nM。 Atazanavir 在 RF/MT-2 菌株中表现出有效的抗病毒活性,EC50 为 3.89 nM。 Atazanavir 是一种胆红素葡萄糖醛酸化抑制剂,IC50 为 2.4 μM。 Atazanavir 抑制重组 UGT1A1,Ki 为 1.9 μM。 Atazanavir 抑制 U251、T98G 和 LN229 胶质母细胞瘤细胞系的细胞生长,并显着增加 GRP78 和 CHOP 蛋白水平。阿扎那韦导致 U251 胶质母细胞瘤细胞中各种不同大小的多泛素化蛋白显着增加。 Atazanavir 还抑制人 20S 蛋白酶体,IC50 为 26 μM。 Atazanavir (30 μM) 改变 HepG2 细胞中 ER 应激和 UPR 基因表达的程度。 Atazanavir (30 mM) 导致 LS180V 细胞中免疫反应性 P-gp 表达增加 2.5 倍,同时细胞内 Rh123 减少。激酶测定:为了确定每种 Prt 抑制剂的抑制常数 (Ki),将纯化的 HIV-1 RF 野生型 Prt (2.5 nM) 与 1 μM 至 15 μM 荧光底物在反应缓冲液(1 M NaCl, 1 mM EDTA、0.1 M 乙酸钠 [pH 5.5]、0.1% 聚乙二醇 8000),存在或不存在阿扎那韦。使用 Cytoflor 4000 在 340 nM 激发后,通过测量 490 nM 荧光发射的增加来量化底物的裂解。使用 1.36 μM、1.66 μM、2.1 μM、3.0 μM、5.0 μM 或 15 μM 底物进行反应存在五种浓度的阿扎那韦(1.25 nM 至 25 nM)。以 5 分钟的间隔监测底物裂解,持续 30 分钟。然后确定每个样品在反应早期时间点的裂解率,并根据所得米氏图的斜率确定 Ki 值。细胞测定:为了确定细胞毒性,将宿主细胞在连续稀释的阿扎那韦存在下孵育 6 天,并使用 XTT[2,3-bis(2-methoxy-4-硝基-5-磺基苯基-2H-) 定量细胞活力。 tetrazolium-5-carboxanilide] 测定计算 50% 细胞毒性浓度 (CC50s)。为了评估人血清蛋白对抗病毒活性的影响,通常用于测定的 10% 胎牛血清替换为 40% 成人血清或 1 α1-酸性糖蛋白毫克/毫升。
阿扎那韦对rCFs增殖、胶原生成和蛋白质表达的影响[3] 在无CoCl2或有CoCl2的情况下检查rCFs,以模拟缺氧条件下的促纤维化环境。CoCl2诱导缺氧后rCFs增殖较正常组增加(P<0.01),如表1所示,但与CoCl2组相比,在浓度在1至10μM之间的阿扎那韦硫酸盐处理后,以浓度依赖的方式受到显著抑制(P<0.05)。为了进一步表征这种抑制作用,硫酸阿扎那韦处理与TLR 9拮抗剂HCQ联合使用。然而,与HCQ组相比,rCFs增殖没有进一步下降(P>0.05),如表1所示。此外,在CoCl2刺激的rCFs中测量了I型胶原和III型胶原的含量。结果显示,与正常组相比,I型胶原和III型胶原含量增加(P < 0.01). 然而,与CoCl2组相比,浓度在1至10μM之间的阿扎那韦硫酸盐治疗后,I型胶原和III型胶原水平以浓度依赖的方式显著降低(P<0.05),如表1所示。与HCQ组相比,阿扎那韦3μM加HCQ 3μM组的I型胶原和III型胶原没有进一步下降(P > 0.05), 如表1所示。 为了进一步研究硫酸阿扎那韦在缺氧期间减少rCFs增殖的机制,我们研究了有或没有硫酸阿扎那韦时HMGB1、p-NF-κB、p-IκBα和总NF-κB的表达。在CoCl2诱导的缺氧后,HMGB1、p-NF-κB、p-IκBα和TLR 9的表达与正常组相比有所增加(p < 0.01), 如图1A和B所示,但与CoCl2组相比,经1-10μM硫酸阿扎那韦处理后,HMGB1、p-IκBα和p-NF-κB的表达受到显著抑制(p<0.05或p<0.01),如图1A和B所示。HCQ处理降低了HMGB1、p-NF-κB和TLR 9的表达(p<0.05或p<0.05) < 0.01). 与HCQ组相比,阿扎那韦治疗联合HCQ对HMGB1、TLR 9和p-NF-κB表达没有进一步下降(p>0.05),如图1C和D所示。这些发现表明,阿扎那韦通过调节HMGB1/TLR 9通路来减轻缺氧诱导的rCFs增殖。 |
| 体内研究 (In Vivo) |
阿扎那韦硫酸盐对心肌功能的影响[3]
我们评估了阿扎那韦对心肌梗死28天后左心室左心室收缩压和±dp/dtmax的影响。与赋形剂治疗的动物相比,用阿扎那韦治疗的大鼠LVSP明显改善+如表2所示,MI后28天的dp/dtmax和-dp/dtmax。此外,我们发现与HCQ组相比,SP、DP和HR没有进一步变化(P>0.05)。很明显,连续28天的阿扎那韦治疗为心肌梗死后的心肌功能恢复提供了长期益处。 阿扎那韦对心肌梗死28天后心肌胶原体积和心肌细胞肥大的影响[3] 为了阐明阿扎那韦长期改善心脏功能的机制,我们研究了阿扎那韦治疗对非梗死区域壁肥大和胶原体积以及梗死面积的影响。赋形剂治疗组和阿扎那韦30 mg/kg组的梗死面积没有差异(38.11±4.15%和38.80±4.62%,分别)。如图2A、C和D所示,与Sham大鼠相比,载体治疗大鼠的非梗死左心室心肌细胞的横截面积和直径以及心肌细胞的肥大显著增加,而阿扎那韦则抑制了这一现象。如图2B和E所示,阿扎那韦显著减弱了左心室边缘形态计量胶原体积分数的增加。与上述结果一致,载体治疗的大鼠与假大鼠相比心脏指数(心脏重量与体重之比)增加,如图2F所示,连续阿扎那韦治疗显著降低了心脏指数(p<0.05)。 阿扎那韦对体内α-SMA、HMGB1、p-NF-κB、TLR 9、I型胶原、III型胶原表达和Hyp含量的影响[3] Western blot分析还检测了α-SMA、HMGB1、TLR 9、p-NF-κB、I型胶原和III型胶原表达的变化,如图3-5所示。在载体处理的大鼠中,所有检测到的蛋白质表达水平和Hyp含量均相对于假手术动物增加(P < 0.01), 而与赋形剂治疗的大鼠相比,阿扎那韦治疗后这些蛋白质表达水平和Hyp含量降低(P < 0.01). 体外和体内研究结果表明,阿扎那韦可以通过调节HMGB1/TLR 9通路来减少成纤维细胞增殖和胶原沉积。 |
| 酶活实验 |
将纯化的 HIV-1 RF 野生型 Prt (2.5 nM) 与 1 μM 至 15 μM 荧光底物在反应缓冲液(1 M NaCl、1 mM EDTA、0.1 M 乙酸钠 [pH 5.5]、0.1%)中于 37 °C 孵育聚乙二醇 8000),有或没有阿扎那韦,以计算每种 Prt 抑制剂的抑制常数 (Ki)。使用 Cytoflor 4000,以 340 nM 激发后 490 nM 荧光发射的增加来测量底物的裂解。在五种不同浓度的阿扎那韦(1.25 nM 至 25 nM)中,使用 1.36 μM、1.66 μM、2.1 μM、3.0 μM、5.0 μM 或 15 μM 的底物进行反应。在半小时内,每五分钟观察一次底物裂解。然后,在反应的早期阶段,计算每个样品的裂解率,并根据随后的 Michaelis-Menten 图的斜率确定 Ki 值。
|
| 细胞实验 |
为了评估细胞毒性,将宿主细胞与连续稀释的阿扎那韦一起培养六天。然后使用 XTT[2,3-双(2-甲氧基-4-硝基-5-磺基苯基-2H-四唑鎓-5-甲酰苯胺)]测定法测量细胞活力,产生 50% 细胞毒性浓度 (CC50s)。为了评估人血清蛋白如何影响抗病毒活性,将 40% 成人血清或 1 mg α1-酸性糖蛋白/mL 添加到通常用于检测的 10% 胎牛血清中。
细胞培养和表达分析[3] 根据之前的方法(Villarreal等人,1993)分离来自新生(1至2天大)Sprague-Dawley大鼠的大鼠心脏成纤维细胞(rCFs)。细胞在含有10%胎牛血清的Dulbecco改良Eagle培养基(DMEM)中培养,在37°C、5%CO2的加湿培养箱中,添加100kU/L青霉素和100mg/L链霉素。将细胞培养至约70%融合,并在治疗前在无血清DMEM中饥饿过夜。然后用3μM阿他扎那韦硫酸酯(纯度>99.0%;CAS编号:229975-97-7)处理细胞72小时,含或不含氯化钴(CoCl2;100μM),然后提取蛋白质。 rCFs增殖测定和表达评估[3] 为了评估细胞增殖,如上所述维持rCFs。将细胞暴露于100μM的CoCl2中以模拟缺氧,并用不同浓度的阿扎那韦(0、1、3、10μM)处理72小时,可加或不加TLR 9拮抗剂3μM羟氯喹(HCQ)。通过细胞计数测定细胞增殖水平。 为了检查表达的变化,将细胞接种到6孔平底板中,并如上所述进行维护,每块板保留一孔作为未处理的对照。用含有或不含有CoCl2(100μM)的3μM阿塔扎那韦硫酸盐处理细胞72小时,然后收集上清液并提取蛋白质。ELISA试剂盒检测I型胶原和III型胶原。通过Western blot检测TLR 9、HMGB1、p-NF-κB、p-IκBα和总NF-κB的表达水平,并如上所述进行归一化和显示。为了研究rCF增殖减少的可能机制,将细胞用3μM阿扎那韦硫酸盐(含或不含3μM HCQ)处理72小时,如上所述,使用Western blot检测TLR 9和HMGB1和p-NF-κB的表达水平。 |
| 动物实验 |
Induction of myocardial infarction (MI) model and experimental assessment [3]
Briefly, Rats were anesthetized with ketamine 100 mg/kg (i.m.) and xylazine 10 mg/kg (i.m.) and ventilated with room air using a rodent respirator. The chest was opened by middle thoracotomy and the left coronary artery was ligated at 2–3 mm from its origin between the left atrium and pulmonary artery conus using a 6-0 prolene suture. A successful operation was confirmed by the occurrence of ST-segment elevation in an electrocardiogram. This operation was performed by an experimenter who was blinded to the group assignments of the animals to avoid subjective bias of the experimenter on the outcome. The sham-operated group underwent thoracotomy and cardiac exposure without coronary ligation. Thirty rats were divided into three groups including (I) non-MI rats; (II) MI rats received saline alone; (III) MI rats received intragastric administration of Atazanavir sulfate (30 mg/kg) plus ritonavir (10 mg/kg). Atazanavir is a low oral bioavailability compound and, clinically, is generally coadministrated with Ritonavir, which boosts the oral bioavailability of atazanavir by inhibiting cytochrome P450 (CYP) 3A4, and P-glycoprotein via the same metabolic pathway (Le Tiec et al., 2005, 021567s026lbl). The rats were administered daily via intragastric administration of corresponding drug for continuous 28 days after MI 24 h. Treatment was orally administered on a daily basis for atazanavir-treated animals, while animals in the vehicle-treated and sham groups were given an equal volume of saline. At day 29, determine hemodynamics and analyze histopathological change. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Atazanavir is rapidly absorbed with a Tmax of approximately 2.5 hours. Atazanavir demonstrates nonlinear pharmacokinetics with greater than dose-proportional increases in AUC and Cmax values over the dose range of 200 to 800 mg once daily. A steady state is achieved between Days 4 and 8, with an accumulation of approximately 2.3-fold. Administration of atazanavir with food enhances bioavailability and reduces pharmacokinetic variability. Administration of a single 400-mg dose of atazanavir with a light meal (357 kcal, 8.2 g fat, 10.6 g protein) resulted in a 70% increase in AUC and 57% increase in Cmax relative to the fasting state. Administration of a single 400-mg dose of atazanavir with a high-fat meal (721 kcal, 37.3 g fat, 29.4 g protein) resulted in a mean increase in AUC of 35% with no change in Cmax relative to the fasting state. Administration of atazanavir with either a light or high-fat meal decreased the coefficient of variation of AUC and Cmax by approximately one-half compared to the fasting state. Coadministration of a single 300-mg dose of atazanavir and a 100-mg dose of ritonavir with a light meal (336 kcal, 5.1 g fat, 9.3 g protein) resulted in a 33% increase in the AUC and a 40% increase in both the Cmax and the 24-hour concentration of atazanavir relative to the fasting state. Coadministration with a high-fat meal (951 kcal, 54.7 g fat, 35.9 g protein) did not affect the AUC of atazanavir relative to fasting conditions and the Cmax was within 11% of fasting values. The 24-hour concentration following a high-fat meal was increased by approximately 33% due to delayed absorption; the median Tmax increased from 2.0 to 5.0 hours. Coadministration of atazanavir with ritonavir with either a light or a high-fat meal decreased the coefficient of variation of AUC and Cmax by approximately 25% compared to the fasting state. Following a single 400-mg dose of 14C-atazanavir, 79% and 13% of the total radioactivity was recovered in the feces and urine, respectively. Unchanged drugs accounted for approximately 20% and 7% of the administered dose in the feces and urine, respectively. In patients with HIV infection, the volume of distribution of atazanavir was estimated to be 88.3 L. In patients with HIV infection, the clearance of atazanavir was estimated to be 12.9 L/hr. Atazanavir is rapidly absorbed with a Tmax of approximately 2.5 hours. Atazanavir demonstrates nonlinear pharmacokinetics with greater than dose-proportional increases in AUC and Cmax values over the dose range of 200-800 mg once daily. Steady-state is achieved between Days 4 and 8, with an accumulation of approximately 2.3-fold. Administration of /atazanavir/ with food enhances bioavailability and reduces pharmacokinetic variability. Administration of a single dose of /atazanavir/ with a light meal (357 kcal, 8.2 g fat, 10.6 g protein) resulted in a 70% increase in AUC and 57% increase in Cmax relative to the fasting state. Administration of a single dose of /atazanavir/ with a high-fat meal (721 kcal, 37.3 g fat, 29.4 g protein) resulted in a mean increase in AUC of 35% with no change in Cmax relative to the fasting state. Administration of /atazanavir/ with either a light meal or high-fat meal decreased the coefficient of variation of AUC and Cmax by approximately one half compared to the fasting state. Peak plasma concentration: Healthy subjects: 5199 ng/mL on day 29 following a 400 mg daily dose with a light meal. HIV-infected patients: 2298 ng/mL on day 29 following a 400 mg daily dose with a light meal. Time to peak concentration: HIV-infected patients: 2 hours. For more Absorption, Distribution and Excretion (Complete) data for ATAZANAVIR (8 total), please visit the HSDB record page. Metabolism / Metabolites Atazanavir is extensively metabolized in humans. The major biotransformation pathways of atazanavir in humans consisted of monooxygenation and dioxygenation. Other minor biotransformation pathways for atazanavir or its metabolites consisted of glucuronidation, N-dealkylation, hydrolysis, and oxygenation with dehydrogenation. Two minor metabolites of atazanavir in plasma have been characterized. Neither metabolite demonstrated in vitro antiviral activity. In vitro studies using human liver microsomes suggested that atazanavir is metabolized by CYP3A. Atazanavir is extensively metabolized in humans. The major biotransformation pathways of atazanavir in humans consisted of monooxygenation and (atazanavir sulfate) dioxygenation. Other minor biotransformation pathways for atazanavir or its metabolites consisted of glucuronidation, N-dealkylation, hydrolysis, and oxygenation with dehydrogenation. Two minor metabolites of atazanavir in plasma have been characterized. Neither metabolite demonstrated in vitro antiviral activity. In vitro studies using human liver microsomes suggested that atazanavir is metabolized by CYP3A. Biological Half-Life The mean elimination half-life of atazanavir in healthy subjects (n=214) and adult subjects with HIV-1 infection (n=13) was approximately 7 hours at steady state following a dose of 400 mg daily with a light meal. Elimination half-life in hepatically impaired is 12.1 hours (following a single 400 mg dose). The mean half-life of atazanavir in hepatically impaired subjects was 12.1 hours compared with 6.4 hours in healthy volunteers. ... The mean elimination half-life of atazanavir in healthy volunteers (n=214) and HIV-infected adult patients (n=13) was approximately 7 hours at steady state following a dose of 400 mg daily with a light meal. Pharmacokinetics & metabolism [2] Atazanavir is rapidly absorbed after oral administration (Tmax 2.5 h) and demonstrates nonlinear pharmacokinetics, resulting in greater than dose-proportional increases in bioavailability (AUC and Cmax) over a dose range of 200–800 mg daily. Administration of atazanavir with food enhances bioavailability and reduces pharmacokinetic variability. Once absorbed, atazanavir is highly bound to plasma proteins α1-acid glycoprotein and albumin to similar extents (89 and 86%, respectively). Atazanavir is extensively metabolized by the hepatic cytochrome P450 (CYP) system to form two main inactive metabolites and is both a substrate and inhibitor of the CYP3A4 isoenzyme. In vitro studies have also demonstrated that atazanavir is both an inhibitor and inducer of the P-glycoprotein ATP-dependent efflux pump, which has a wide cellular distribution and a broad substrate specificity, further increasing its potential for drug-drug interactions and variable pharmacokinetics in vivo [17]. Atazanavir should therefore be used with caution in patients taking strong CYP3A4 inhibitors, moderate or strong CYP3A4 inducers and major CYP3A4 substrates. Coadministration with drugs that induce CYP3A4, such as rifampicin, may decrease atazanavir plasma concentrations and reduce clinical effect, while drugs that inhibit CYP3A4 may elevate atazanavir levels and increase toxicity. The mean elimination half-life of atazanavir 400 mg taken with food is approximately 7–8 h at steady state with 20 and 7% of active drug eliminated in feces and urine, respectively. In vitro studies have indicated that a direct inhibition of UGT1A1-mediated bilirubin glucuronidation by free, nonproteinbound atazanavir gives a mechanistic rationale for dose-related hyperbilirubinemia. Indinavir may similarly inhibit UGT1A and coadministration with atazanavir is not recommended. Large inter- and intrapatient variability in atazanavir plasma concentrations have been demonstrated in population pharmacokinetic studies, yet the same dose of atazanavir is currently administered regardless to differences in systemic blood and tissue disposition. The therapeutic range of atazanavir lies between 150 and 850 ng/ml [21,102]; however, plasma levels in the absence of RTV have been reported to be frequently lower than the target Cmin of 150 ng/ml in both patients and substance. The wide interpersonal variability in atazanavir exposure has been considered an indication for twice daily dosing or therapeutic drug monitoring. However, no significant relationship has been established between atazanavir plasma trough concentration (Cmin) and antiviral response in patients starting atazanavir without PI mutations. The wide variability in atazanavir exposure strongly supports the preferable use of RTV-boosted atazanavir in PI-experienced individuals. |
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation Amounts of atazanavir in milk appear to be low based on limited data. The combination product, which also contains the CYP3A inhibitor cobicistat, has not been studied during breastfeeding, but would be expected to have similar or greater levels of atazanavir in milk. Achieving and maintaining viral suppression with antiretroviral therapy decreases breastfeeding transmission risk to less than 1%, but not zero. Individuals with HIV who are on antiretroviral therapy with a sustained undetectable viral load and who choose to breastfeed should be supported in this decision. If a viral load is not suppressed, banked pasteurized donor milk or formula is recommended. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Gynecomastia has been reported among men receiving highly active antiretroviral therapy. Gynecomastia is unilateral initially, but progresses to bilateral in about half of cases. No alterations in serum prolactin were noted and spontaneous resolution usually occurred within one year, even with continuation of the regimen. Some case reports and in vitro studies have suggested that protease inhibitors might cause hyperprolactinemia and galactorrhea in some male patients, although this has been disputed. The relevance of these findings to nursing mothers is not known. The prolactin level in a mother with established lactation may not affect her ability to breastfeed. Interactions Pharmacologic interaction with bepridil (potential for serious and/or life-threatening adverse effects). Concomitant use of bepridil and atazanavir not recommended. Pharmacokinetic interaction with antiarrhythmic agents (i.e., amiodarone, systemic lidocaine, quinidine). Potential for serious and/or life-threatening adverse effects. Monitor plasma concentrations of these antiarrhythmic agents if used concomitantly with atazanavir. Potential pharmacokinetic interaction (increased plasma concentration of the tricyclic antidepressant). Potential for serious and/or life-threatening adverse effects. Monitor plasma concentrations of these tricyclic antidepressants agents if used concomitantly with atazanavir. Pharmacokinetic interaction with rifampin (substantial decrease (90%) in the peak plasma concentration and area under the concentration-time curve (AUC) of HIV protease inhibitors). Concomitant use of atazanavir and rifampin not recommended. For more Interactions (Complete) data for ATAZANAVIR (34 total), please visit the HSDB record page. Toxicity Summary Currently, no specific antidote exists for atazanavir toxicity. Patients should receive symptomatic and supportive care from healthcare staff while regularly monitoring their vital signs and looking for signs of respiratory distress. Electrocardiogram monitoring of the patient is recommended, as atazanavir may exacerbate AV block due to PR interval prolongation. In cases where a simultaneous overdose with nucleoside reverse transcriptase inhibitors is suspected, clinicians should carefully monitor patients for symptoms of lactic acidosis. Hepatotoxicity Atazanavir can cause several forms of liver injury including transient serum enzyme elevations, indirect hyperbilirubinemia, idiosyncratic acute liver injury and exacerbation of underlying chronic viral hepatitis. Some degree of serum aminotransferase elevations occurs in a high proportion of patients taking atazanavir containing antiretroviral regimens. Moderate-to severe elevations in serum aminotransferase levels (>5 times the upper limit of normal) are found in 3% to 10% of patients, although rates may be higher in patients with HIV-HCV coinfection. These elevations are usually asymptomatic and self-limited and can resolve even with continuation of the medication. Atazanavir therapy (similar to indinavir) also causes increases in unconjugated (indirect) and total serum bilirubin that can manifest as jaundice in up to 10% of patients. These elevations are due to the inhibition of UDP glucuronyl transferase, the hepatic enzyme responsible for conjugation of bilirubin that is deficient in Gilbert syndrome. The hyperbilirubinemia is usually mild, the increases averaging 0.3-0.5 mg/dL, but can be more marked in patients with Gilbert syndrome with increases of 1.5 mg/dL or more and clinical jaundice. The jaundice, however, is not indicative of hepatic injury. Clinically apparent acute liver injury due to atazanavir is rare and the clinical pattern of liver injury, latency and recovery have not been well defined. The liver injury is idiosyncratic and rare and probably similar to the injury that is caused by other HIV protease inhibitors. The liver injury typically arises 1 to 8 weeks after starting the protease inhibitor and has variable patterns of liver enzyme elevation, from hepatocellular to cholestatic. Signs of hypersensitivity (fever, rash, eosinophilia) are rare, as is autoantibody formation. The acute liver injury is usually self-limited and resolves within a few weeks of stopping the antiretroviral agent (Case 1). In addition, initiation of atazanavir based antiretroviral therapy can lead to exacerbation of an underlying chronic hepatitis B or C in coinfected individuals, typically arising 2 to 12 months after starting therapy, and associated with a hepatocellular pattern of serum enzyme elevations and increases in serum levels of hepatitis B virus (HBV) DNA or hepatitis C virus (HCV) RNA. Atazanavir therapy has not been clearly linked to lactic acidosis and acute fatty liver that is reported in association with several nucleoside analogue reverse transcriptase inhibitors. Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Amounts of atazanavir in milk appear to be low based on limited data. The combination product, which also contains the CYP3A inhibitor cobicistat, has not been studied during breastfeeding, but would be expected to have similar or greater levels of atazanavir in milk. Achieving and maintaining viral suppression with antiretroviral therapy decreases breastfeeding transmission risk to less than 1%, but not zero. Individuals with HIV who are on antiretroviral therapy with a sustained undetectable viral load and who choose to breastfeed should be supported in this decision. If a viral load is not suppressed, banked pasteurized donor milk or formula is recommended. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Gynecomastia has been reported among men receiving highly active antiretroviral therapy. Gynecomastia is unilateral initially, but progresses to bilateral in about half of cases. No alterations in serum prolactin were noted and spontaneous resolution usually occurred within one year, even with continuation of the regimen. Some case reports and in vitro studies have suggested that protease inhibitors might cause hyperprolactinemia and galactorrhea in some male patients, although this has been disputed. The relevance of these findings to nursing mothers is not known. The prolactin level in a mother with established lactation may not affect her ability to breastfeed. Adverse Effects Common adverse effects of atazanavir include hyperbilirubinemia (35% to 49% in adults and 16% in children), rash (up to 21%), hypercholesterolemia (6% to 25%), hyperamylasemia (14% to 33%), jaundice (5% to 9% in adults and 13% to 15% in children), nausea (3% to 14%), cough (21% in children), and fever (2% in adults and 18% to 19% in children). Severe adverse effects include Stevens-Johnson syndrome, toxic skin eruptions, erythema multiforme, angioedema, cholecystitis, pancreatitis, interstitial nephritis, diabetic ketoacidosis, and AV block. Additional potential adverse effects include nephrolithiasis, cholelithiasis, hyperlipidemia, hypertriglyceridemia, bleeding, pancreatitis, exacerbation of diabetes mellitus or hyperglycemia, and lactic acidosis when used in combination with nucleoside analogs. Although immune reconstitution inflammatory syndrome (IRIS) is not a direct adverse effect of atazanavir, it is noteworthy that a pathological inflammatory response may occur after initiating antiretroviral treatment for HIV infection. There have been reports of up to a 75% mortality rate in IRIS cases associated with tuberculosis in the central nervous system. Although there have been suggestions that successful treatment with antiretroviral drugs enables the recovery of immune function, it may also exacerbate existing opportunistic infections (paradoxical IRIS) or reveal previously undetected opportunistic infections (unmasking IRIS). Clinical symptoms may vary based on the type of opportunistic infections, but a common feature includes acute generalized or local inflammatory responses, such as fever or localized tissue edema. Therefore, the timing of initiating antiretroviral therapy is crucial to prevent IRIS. Drug-Drug Interactions Atazanavir is metabolized through the CYP3A4 pathway and has inhibitory effects on CYP3A4, CYP1A2, and CYP2C9 enzymes. Therefore, patients taking medications that inhibit or are substrates of these enzymes, especially those with a narrow therapeutic index, should avoid atazanavir. Significant drug interactions may arise with warfarin, irinotecan, diltiazem, simvastatin, lovastatin, phosphodiesterase inhibitors, St John's wort, and tenofovir. Protein Binding Atazanavir is 86% bound to human serum proteins and protein binding is independent of concentration. Atazanavir binds to both alpha-1-acid glycoprotein (AAG) and albumin to a similar extent (89% and 86%, respectively). |
| 参考文献 | |
| 其他信息 |
Atazanavir (brand name: Reyataz) is a prescription medicine approved by the U.S. Food and Drug Administration (FDA) for the treatment of HIV infection in adults and children. Atazanavir comes in two different dosage forms: capsules and oral powder.
Atazanavir capsules are approved for use in adults and children 6 years of age and older who weigh at least 33 lb (15 kg). Atazanavir capsules may be used with a pharmacokinetic enhancer (boosting agent) – either ritonavir (brand name: Norvir) or cobicistat (brand name: Tybost). (A fixed-dose combination tablet containing atazanavir and cobicistat [brand name: Evotaz] is also available.) Atazanavir oral powder is approved for use in children 3 months of age and older who weigh at least 11 lb (5 kg) and must be used with the boosting agent ritonavir. Atazanavir is always used in combination with other HIV medicines. Atazanavir Sulfate is a sulfate salt form of atazanavir, an aza-dipeptide analogue with a bis-aryl substituent on the (hydroxethyl)hydrazine moiety with activity against both wild type and mutant forms of HIV protease. Atazanavir does not elevate serum lipids, a common problem with other protease inhibitors. An azapeptide and HIV-PROTEASE INHIBITOR that is used in the treatment of HIV INFECTIONS and AIDS in combination with other ANTI-HIV AGENTS. See also: Atazanavir (has active moiety); Atazanavir sulfate; ritonavir (component of); Atazanavir sulfate; cobicistat (component of) ... View More ... Drug Indication Reyataz capsules, co-administered with low dose ritonavir, are indicated for the treatment of HIV-1 infected adults and paediatric patients 6 years of age and older in combination with other antiretroviral medicinal products (see section 4. 2). Based on available virological and clinical data from adult patients, no benefit is expected in patients with strains resistant to multiple protease inhibitors (⥠4 PI mutations). The choice of Reyataz in treatment experienced adult and paediatric patients should be based on individual viral resistance testing and the patient's treatment history (see sections 4. 4 and 5. 1). Reyataz oral powder, co-administered with low dose ritonavir, is indicated in combination with other antiretroviral medicinal products for the treatment of HIV-1 infected paediatric patients at least 3 months of age and weighing at least 5 kg (see section 4. 2). Based on available virological and clinical data from adult patients, no benefit is expected in patients with strains resistant to multiple protease inhibitors (ï³ 4 PI mutations). The choice of Reyataz in treatment experienced adult and paediatric patients should be based on individual viral resistance testing and the patient's treatment history (see sections 4. 4 and 5. 1). Treatment of human immunodeficiency virus (HIV-1) infection. Therapeutic Uses Atazanavir sulfate is indicated in combination with other antiretroviral agents for the treatment of HIV-1 infection. The use of atazanavir sulfate may be considered in antiretroviral-treatment experienced adults with HIV strains that are expected to be susceptible to atazanavir sulfate by genotypic and phenotypic testing. /Included in US product labeling/ Drug Warnings Lactic acidosis syndrome, sometimes fatal, and symptomatic hyperlactatemia have been reported in patients receiving atazanavir in conjunction with nucleoside reverse transcriptase inhibitors (NRTIs). Therapy with NRTIs is known to be associated with an increased risk of lactic acidosis syndrome; female gender and obesity also are known risk factors for this syndrome. Whether atazanavir contributes to the risk of lactic acidosis syndrome remains to be established. Hyperglycemia (potentially persistent), new-onset diabetes mellitus, or exacerbation of preexisting diabetes mellitus has been reported in patients receiving HIV protease inhibitors. May require initiation of antidiabetic therapy (e.g., insulin, oral antidiabetic agents) or dosage adjustment for existing diabetes; diabetic ketoacidosis can occur. Abnormalities in AV conduction, including prolongation of the PR interval, have occurred in individuals receiving atazanavir. Cardiac conduction abnormalities generally are limited to first-degree AV block; prolongation of the QTc interval observed in HIV-infected patients receiving atazanavir have not been directly attributed to the drug. Asymptomatic first-degree AV block was observed in 5.9 or 3-10.4% of patients in clinical trials receiving regimens that included atazanavir or comparator antiretrovirals (lopinavir/ritonavir, nelfinavir, efavirenz), respectively; second- or third-degree block was not observed. Atazanavir should be used with caution in patients with cardiac conduction abnormalities (e.g., marked first-degree AV block; second- or third-degree AV block) because of lack of clinical experience. Because atazanavir is a competitive inhibitor of uridine diphosphate-glucuronosyltransferase (UGT) 1A1 (an enzyme that catalyzes the glucuronidation of bilirubin), reversible asymptomatic elevations in indirect (unconjugated) bilirubin occur in most patients receiving the drug. Total bilirubin concentrations at least 2.6 times the upper limit of normal have been reported in 35-47% of patients receiving the drug in clinical trials; long-term safety data are not available for patients experiencing persistent elevations in total bilirubin exceeding 5 times the upper limit of normal. Increases in serum AST (SGOT) and/or ALT (SGPT) concentrations that occur with hyperbilirubinemia should be evaluated for etiologies other than hyperbilirubinemia. If jaundice or scleral icterus that result from bilirubin elevations cause cosmetic concerns, alternative antiretroviral therapy can be considered; reduction of atazanavir dosage not recommended (efficacy data not available for reduced dosages). For more Drug Warnings (Complete) data for ATAZANAVIR (17 total), please visit the HSDB record page. Pharmacodynamics Atazanavir (ATV) is an azapeptide HIV-1 protease inhibitor (PI) with activity against Human Immunodeficiency Virus Type 1 (HIV-1). HIV-1 protease is an enzyme required for the proteolytic cleavage of the viral polyprotein precursors into the individual functional proteins found in infectious HIV-1. Atazanavir binds to the protease active site and inhibits the activity of the enzyme. This inhibition prevents cleavage of the viral polyproteins resulting in the formation of immature non-infectious viral particles. Protease inhibitors are almost always used in combination with at least two other anti-HIV drugs. Atazanivir is pharmacologically related but structurally different from other protease inhibitors and other currently available antiretrovirals. Atazanavir exhibits anti-HIV-1 activity with a mean 50% effective concentration (EC50) in the absence of human serum of 2 to 5 nM against a variety of laboratory and clinical HIV-1 isolates grown in peripheral blood mononuclear cells, macrophages, CEM-SS cells, and MT-2 cells. Atazanavir has activity against HIV-1 Group M subtype viruses A, B, C, D, AE, AG, F, G, and J isolates in cell culture. Atazanavir has variable activity against HIV-2 isolates (1.9-32 nM), with EC50 values above the EC50 values of failure isolates. Two-drug combination antiviral activity studies with atazanavir showed no antagonism in cell culture with PIs (amprenavir, indinavir, lopinavir, nelfinavir, ritonavir, and saquinavir), NNRTIs (delavirdine, efavirenz, and nevirapine), NRTIs (abacavir, didanosine, emtricitabine, lamivudine, stavudine, tenofovir DF, and zidovudine), the HIV-1 fusion inhibitor enfuvirtide, and two compounds used in the treatment of viral hepatitis, adefovir and ribavirin, without enhanced cytotoxicity. HIV-1 isolates with a decreased susceptibility to atazanavir have been selected in cell culture and obtained from patients treated with atazanavir or atazanavir with ritonavir. HIV-1 isolates with 93- to 183-fold reduced susceptibility to atazanavir from three different viral strains were selected in cell culture for 5 months. The substitutions in these HIV-1 viruses that contributed to atazanavir resistance include I50L, N88S, I84V, A71V, and M46I. Changes were also observed at the protease cleavage sites following drug selection. Recombinant viruses containing the I50L substitution without other major PI substitutions were growth impaired and displayed increased susceptibility in cell culture to other PIs (amprenavir, indinavir, lopinavir, nelfinavir, ritonavir, and saquinavir). The I50L and I50V substitutions yielded selective resistance to atazanavir and amprenavir, respectively, and did not appear to be cross-resistant. Concentration- and dose-dependent prolongation of the PR interval in the electrocardiogram has been observed in healthy subjects receiving atazanavir. In placebo-controlled Study AI424-076, the mean (±SD) maximum change in PR interval from the predose value was 24 (±15) msec following oral dosing with 400 mg of atazanavir (n=65) compared to 13 (±11) msec following dosing with placebo (n=67). The PR interval prolongations in this study were asymptomatic. There is limited information on the potential for a pharmacodynamic interaction in humans between atazanavir and other drugs that prolong the PR interval of the electrocardiogram. Electrocardiographic effects of atazanavir were determined in a clinical pharmacology study of 72 healthy subjects. Oral doses of 400 mg (maximum recommended dosage) and 800 mg (twice the maximum recommended dosage) were compared with placebo; there was no concentration-dependent effect of atazanavir on the QTc interval (using Fridericia’s correction). In 1793 subjects with HIV-1 infection, receiving antiretroviral regimens, QTc prolongation was comparable in the atazanavir and comparator regimens. No atazanavir-treated healthy subject or subject with HIV-1 infection in clinical trials had a QTc interval >500 msec Azatanavir is a protease inhibitor (PI) approved for the treatment of HIV-1 infection. Atazanavir is a substrate and inhibitor of cytochrome P450 isozyme 3A and an inhibitor and inducer of P-glycoprotein. It has similar virologic efficacy as efavirenz and ritonavir-boosted lopinavir in antiretroviral-naive individuals. Its impact on lipids is less than other PIs and it is suitable for those in whom hyperlipidemia is undesirable. Ritonavir boosting of atazanavir enhances the bioavailability of atazanavir but may result in some elevation of lipids and is recommended for treatment-experienced patients and those receiving efavirenz or tenofovir. Ritonavir-boosted atazanavir has similar antiviral activity as ritonavir-boosted lopinavir in both antiretroviral therapy-naive and -experienced patients. Atazanavir causes unconjugated bilirubinemia in over 40% of patients but results in less than 2% discontinuations. Atazanavir is licensed for once-daily use and atazanavir/ritonavir competes with lopinavir/ritonavir as the most commonly prescribed PI.[2] Atazanavir is a recently approved human immunodeficiency virus (HIV) protease inhibitor that has an important role in the treatment of both antiretroviral-naive and antiretroviral-experienced individuals. Atazanavir (400 mg) can be administered once per day and requires only 2 capsules. Drug exposure can be safely increased with coadministration of a once-daily regimen of atazanavir (300 mg) and ritonavir (100 mg). Atazanavir is not associated with elevations in serum levels of total cholesterol, low-density lipoprotein cholesterol, or triglycerides, potentially reducing the need for lipid-lowering agents. Atazanavir is associated with elevations in unconjugated bilirubin levels, which are usually not dose limiting. For treatment-naive patients receiving atazanavir who experience virologic rebound, the I50L mutation in HIV protease arises, which does not confer cross-resistance to other protease inhibitors. In treatment-experienced patients with high-level resistance to other protease inhibitors, susceptibility to atazanavir is usually reduced, and optimal effects of atazanavir are seen when it is administered with ritonavir. Similar to other protease inhibitors, careful attention must be paid to drug interactions when administering atazanavir with concomitant medications. [1] |
| 分子式 |
C38H54N6O11S
|
|---|---|
| 分子量 |
802.93
|
| 精确质量 |
802.357
|
| 元素分析 |
C, 56.84; H, 6.78; N, 10.47; O, 21.92; S, 3.99
|
| CAS号 |
229975-97-7
|
| 相关CAS号 |
Atazanavir;198904-31-3
|
| PubChem CID |
158550
|
| 外观&性状 |
White to light yellow solid powder
|
| 密度 |
1.164g/cm3
|
| 沸点 |
995.5ºC at 760 mmHg
|
| 熔点 |
195.0°, or acetone; mp 198-199° (dec)
|
| 闪点 |
555.8ºC
|
| 蒸汽压 |
0mmHg at 25°C
|
| LogP |
6.203
|
| tPSA |
254.2
|
| 氢键供体(HBD)数目 |
7
|
| 氢键受体(HBA)数目 |
13
|
| 可旋转键数目(RBC) |
18
|
| 重原子数目 |
56
|
| 分子复杂度/Complexity |
1190
|
| 定义原子立体中心数目 |
4
|
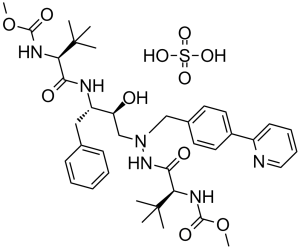
| SMILES |
S(=O)(=O)(O[H])O[H].O([H])[C@@]([H])(C([H])([H])N(C([H])([H])C1C([H])=C([H])C(C2=C([H])C([H])=C([H])C([H])=N2)=C([H])C=1[H])N([H])C([C@]([H])(C(C([H])([H])[H])(C([H])([H])[H])C([H])([H])[H])N([H])C(=O)OC([H])([H])[H])=O)[C@]([H])(C([H])([H])C1C([H])=C([H])C([H])=C([H])C=1[H])N([H])C([C@]([H])(C(C([H])([H])[H])(C([H])([H])[H])C([H])([H])[H])N([H])C(=O)OC([H])([H])[H])=O
|
| InChi Key |
DQSGVVGOPRWTKI-QVFAWCHISA-N
|
| InChi Code |
InChI=1S/C38H52N6O7.H2O4S/c1-37(2,3)31(41-35(48)50-7)33(46)40-29(22-25-14-10-9-11-15-25)30(45)24-44(43-34(47)32(38(4,5)6)42-36(49)51-8)23-26-17-19-27(20-18-26)28-16-12-13-21-39-28;1-5(2,3)4/h9-21,29-32,45H,22-24H2,1-8H3,(H,40,46)(H,41,48)(H,42,49)(H,43,47);(H2,1,2,3,4)/t29-,30-,31+,32+;/m0./s1
|
| 化学名 |
methyl N-[(2S)-1-[2-[(2S,3S)-2-hydroxy-3-[[(2S)-2-(methoxycarbonylamino)-3,3-dimethylbutanoyl]amino]-4-phenylbutyl]-2-[(4-pyridin-2-ylphenyl)methyl]hydrazinyl]-3,3-dimethyl-1-oxobutan-2-yl]carbamate;sulfuric acid
|
| 别名 |
Atazanavir sulfate; BMS-232632; 229975-97-7; Reyataz; Atazanavir sulphate; Atazanavir (sulfate); BMS 232632; BMS232632
|
| HS Tariff Code |
2934.99.03.00
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (3.11 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (3.11 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (3.11 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: ≥ 2.5 mg/mL (3.11 mM) (饱和度未知) in 5% DMSO + 40% PEG300 + 5% Tween80 + 50% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 5 中的溶解度: ≥ 2.5 mg/mL (3.11 mM) (饱和度未知) in 5% DMSO + 95% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 配方 6 中的溶解度: 30% PEG400+0.5% Tween80+5% propylene glycol: 30 mg/mL 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.2454 mL | 6.2272 mL | 12.4544 mL | |
| 5 mM | 0.2491 mL | 1.2454 mL | 2.4909 mL | |
| 10 mM | 0.1245 mL | 0.6227 mL | 1.2454 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT04468087 | Active Recruiting |
Drug: Atazanavir Drug: Daclatasvir 60 mg |
COVID-19 | Hospital do Coracao | February 15, 2021 | Phase 2 Phase 3 |
| NCT04121195 | Active Recruiting |
Drug: Dose escalation | HIV/AIDS Tuberculosis |
University of Liverpool | October 30, 2020 | Phase 2 Phase 3 |
| NCT02016924 | Recruiting | Drug: ATV Drug: DRV |
Acquired Immune Deficiency Syndrome (AIDS) HIV Infections |
Gilead Sciences | January 16, 2014 | Phase 2 Phase 3 |
| NCT04452565 | Recruiting | Drug: Drug: NA-831 Combination Product: NA-831 and Atazanavir |
Coronavirus Infection Severe Acute Respiratory Infection |
NeuroActiva, Inc. | June 15, 2022 | Phase 2 Phase 3 |
| NCT01837719 | Completed | Drug: Atazanavir Drug: Cobicistat |
HIV-1 | Bristol-Myers Squibb | April 2013 | Phase 1 |