| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g | |||
| Other Sizes |

| 体外研究 (In Vitro) |
在 16HBE 细胞中,二丙酸倍氯米松(1-100 nM;20 分钟)可降低 rhIL-17A 产生的 NT、ROS 和 iNOS 的量以及 STAT-1 的表达[2]。
对人支气管上皮细胞氧化/亚硝化应激的抑制作用:用人支气管上皮细胞预先孵育倍氯米松双丙酸酯(浓度:10⁻⁹、10⁻⁸、10⁻⁷、10⁻⁶ M)1小时,可显著降低香烟烟雾提取物(CSE,5%)+白细胞介素-17A(IL-17A,10 ng/mL)(孵育24小时)诱导的活性氧(ROS)和一氧化氮(NO)生成。在10⁻⁶ M浓度下,倍氯米松双丙酸酯较CSE+IL-17A组使ROS水平降低45%,NO水平降低52%;还可使诱导型一氧化氮合酶(iNOS)mRNA表达下调60%,白细胞介素-8(IL-8)mRNA表达下调55%(实时PCR检测),并抑制核因子-κB(NF-κB)p65的磷酸化(蛋白质印迹法检测)[2] |
|---|---|
| 体内研究 (In Vivo) |
二丙酸倍氯米松(150 µg/kg;雾化;雄性 BALB/c 小鼠)可减少相对嗜酸性粒细胞数量和总细胞计数,同时缓解哮喘[1]。
在哮喘小鼠模型中的疗效:用卵清蛋白(OVA)致敏并激发BALB/c小鼠构建哮喘模型。倍氯米松双丙酸酯通过超声雾化给药,剂量为0.5、1、2 mg/kg,每日1次,连续7天(与OVA激发同步)。2 mg/kg剂量可使小鼠对乙酰甲胆碱(30 mg/mL)的气道高反应性(AHR)降低50%(全身体积描记仪检测),支气管肺泡灌洗液(BALF)中嗜酸性粒细胞计数减少58%,BALF中白细胞介素-4(IL-4)水平降低42%,白细胞介素-5(IL-5)水平降低38%(ELISA检测)。组织学分析显示,2 mg/kg 倍氯米松双丙酸酯可使支气管周围炎症和黏液高分泌减少45%[1] |
| 细胞实验 |
蛋白质印迹分析[2]
细胞类型: 16HBE 细胞 测试浓度: 1、10 和 100 nM 孵育时间:20分钟 实验结果:降低了rhIL-17A产生的iNOS、ROS和NT的水平。 人支气管上皮细胞实验:人支气管上皮细胞培养于添加生长因子的支气管上皮生长培养基(BEGM)中。将细胞接种于6孔板(1×10⁶细胞/孔),培养至80%融合。细胞用倍氯米松双丙酸酯(10⁻⁹至10⁻⁶ M)预处理1小时后,与CSE(5%)和IL-17A(10 ng/mL)共孵育24小时。孵育后进行以下检测: 1. 采用2',7'-二氯二氢荧光素二乙酸酯(DCFH-DA)染色检测ROS水平,在激发波长485 nm、发射波长535 nm处测定荧光强度; 2. 通过格里斯(Griess)反应定量NO水平,在540 nm处测定吸光度; 3. 提取总RNA,采用实时PCR检测iNOS和IL-8的mRNA表达(以GAPDH为内参); 4. 提取总蛋白,采用蛋白质印迹法检测磷酸化NF-κB p65的表达(以β-肌动蛋白为内参)[2] |
| 动物实验 |
Animal/Disease Models: Tenweeks old male balb/c (Bagg ALBino) mouse[2].
Doses: 5 mg/kg (100 μg/ml for 60 min). Route of Administration: Orally at 24 h and 1 h before the LPS aerosol. Experimental Results: Dramatically (P < 0.05) inhibited the decrease of IL-10 level in BAL fluid induced by LPS exposure. Markedly decreased the release of both MMP-2 and MMP-9. Animal/Disease Models: Male balb/c (Bagg ALBino) mouse with asthma[1] Doses: 150 µg/kg Route of Administration: Nebulization Experimental Results: diminished total cell number and relative eosinophil number in BALF . OVA-Induced Asthma Murine Model: 1. Sensitization: Female BALB/c mice (6–8 weeks old) were intraperitoneally injected with 10 μg OVA emulsified in aluminum hydroxide on day 0 and day 7. 2. Challenge: From day 14 to day 20, mice were exposed to 1% OVA aerosol (nebulization time: 30 minutes/day) to induce asthma. 3. Drug Administration: Beclomethasone dipropionate was dissolved in phosphate-buffered saline (PBS) containing 0.1% Tween 80. Mice in the treatment groups received ultrasonic nebulization of Beclomethasone dipropionate at 0.5, 1, or 2 mg/kg (nebulization time: 15 minutes/day) from day 14 to day 20 (once daily, concurrent with OVA challenge). The control group received nebulized PBS+0.1% Tween 80. 4. Sample Collection & Detection: On day 21, mice were euthanized. Bronchoalveolar lavage fluid (BALF) was collected to count inflammatory cells and measure cytokines (IL-4, IL-5) via ELISA. Lung tissues were fixed for histological staining (H&E and PAS) to assess inflammation and mucus secretion. Airway hyperresponsiveness (AHR) was measured 24 hours before euthanasia using a whole-body plethysmograph with methacholine (30 mg/mL) [1] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Following oral inhalation of 320 mcg of beclomethasone dipropionate (BDP), the Cmax was 88 pg/mL and it was reached after 0.5 at post-administration. The mean Cmax of the major and most active metabolite, beclomethasone-17-monopropionate (17-BMP), was 1419 pg/mL at 0.7 hour post-dosing. In another pharmacokinetic study, the AUC of BDP and 17-BMP were 6660 and 6185 pgxh/mL, respectively. The Cmax was 35356 pg/mL for BDP and 2633 pg/mL for 17-BMP, and and the median time to reach these concentrations (Tmax) was 0.2 hours. In the same study, the AUC of 17-BMP following oral and intranasal administration were 10158 and 3660 pgxh/mL, respectively. The Cmax of 17-BMP following oral and intranasal administration were 703 and 310 pg/mL, respectively, and the Tmax was 4 hours. The total bioavailability of 17-BMP following oral and intranasal administration were 41% and 44%, respectively. Regardless of the route of administration, beclomethasone dipropionate and its metabolites are predominantly excreted in the feces, with less than 10% of the drug and its metabolites being excreted in the urine. Following intravenous administration, the steady-state volume of distribution was 20 L for beclomethasone dipropionate and 424 L for the active metabolite, beclomethasone-17-monopropionate. Following intravenous administration, the clearance of beclomethasone dipropionate and 17-BMP were 150 L/h and 120 L/h, respectively. Metabolism / Metabolites During absorption, beclomethasone dipropionate is undergoes rapid and extensive hydrolysis mediated by esterases CYP3A to form beclomethasone-17-monopropionate (17-BMP), beclomethasone-21-monopropionate (21-BMP), and beclomethasone (BOH). 17-BMP is the major active metabolite with the most potent anti-inflammatory activity. About 95% of the total beclomethasone dipropionate administered via oral inhalation undergoes presystemic conversion to form 17-BMP in the lung. Biological Half-Life Following intravenous administration, the half life of beclomethasone dipropionate was 0.5 hours while the half life of the active metabolite 17-BMP was 2.7 hours. Following oral and intranasal administration, the half life of 17-BMP was 8.8 and 5.7 hours, respectively. |
| 毒性/毒理 (Toxicokinetics/TK) |
Protein Binding
Based on the findings of _in vitro_ studies, the protein binding of the main active metabolite, beclomethasone-17-monopropionate (17-BMP), was 94-96% over the concentration range of 1000 to 5000 pg/mL. In Vitro Cytotoxicity: Beclomethasone dipropionate (10⁻⁹ to 10⁻⁶ M) did not affect the viability of human bronchial epithelial cells (detected via MTT assay, cell viability >90% compared to the control group) [2] - In Vivo Toxicity: No significant changes in mouse body weight, or signs of liver/kidney toxicity (e.g., abnormal serum ALT, AST, BUN levels) were observed in the Beclomethasone dipropionate treatment groups (0.5–2 mg/kg) compared to the control group [1] |
| 参考文献 |
|
| 其他信息 |
Beclomethasone Dipropionate can cause developmental toxicity according to state or federal government labeling requirements.
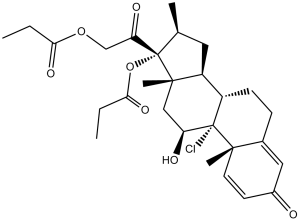
Beclomethasone dipropionate is a steroid ester comprising beclomethasone having propionyl groups at the 17- and 21-positions. It has a role as an anti-inflammatory drug, an anti-asthmatic drug, a prodrug and an anti-arrhythmia drug. It is a steroid ester, an enone, a 20-oxo steroid, an 11beta-hydroxy steroid, a propanoate ester, a corticosteroid, a glucocorticoid, a 3-oxo-Delta(1),Delta(4)-steroid and a chlorinated steroid. It is functionally related to a beclomethasone. Beclomethasone dipropionate is a second-generation synthetic corticosteroid and diester of beclomethasone, which is structurally similar to [dexamethasone]. It is a prodrug of an active metabolite beclomethasone 17-monopropionate (17-BMP) which acts on the glucocorticoid receptor to mediates its therapeutic action. Beclomethasone dipropionate itself posesses weak glucocorticoid receptor binding affinity and is rapidly converted into 17-BMP upon administration. Formulations for oral inhalation, intranasal, and topical use are available for beclomethasone dipropionate. Beclomethasone dipropionate became first available in a pressurized metered-dose inhaler in 1972 and later in a dry powder inhaler and an aqueous nasal spray. Due to its anti-inflammatory, antipruritic, and anti-allergy properties, beclomethasone dipropionate is used in various inflammatory conditions, such as asthma, allergic rhinitis, and dermatoses to reduce symptoms. When inhaled, it is proposed that beclomethasone dipropionate remains active locally in the lung without causing significant side effects associated with systemic corticosteroids. Compared to earlier corticosteroids such as [dexamethasone] and [prednisolone], beclomethasone dipropionate is reported to be less irritating to the nasal mucosa with a longer duration of action when administered intranasally. Beclomethasone Dipropionate is the dipropionate ester of a synthetic glucocorticoid with anti-inflammatory and immunomodulating properties. After cell surface receptor attachment and cell entry, beclomethasone enters the nucleus where it binds to and activates specific nuclear receptors, resulting in an altered gene expression and inhibition of proinflammatory cytokine production. An anti-inflammatory, synthetic glucocorticoid. It is used topically as an anti-inflammatory agent and in aerosol form for the treatment of ASTHMA. See also: Beclomethasone (has active moiety); Beclomethasone 17-Monopropionate (has active moiety); Beclomethasone Dipropionate Monohydrate (annotation moved to). Drug Indication Indicated for oral inhalation use in the maintenance treatment of asthma as prophylactic therapy in patients 5 years of age and older. The aerosol form of beclomethasone diproprionate is not indicated for the relief of acute bronchospasm. Indicated for intranasal use to relieve the symptoms of seasonal or perennial allergic and nonallergic (vasomotor) rhinitis and prevent the recurrence of nasal polyps following surgical removal. Indicated for the relief of the inflammatory and pruritic manifestations of corticosteroid-responsive dermatoses in patients 13 years of age and older. Corticosteroid-responsive dermatoses include psoriasis, contact dermatitis (dermatitis venenata), atopic dermatitis (infantile eczema, allergic dermatitis), neurodermatitis (lichen simplex chronicus, lichen planus, eczema, eczematous dermatitis), intertrigo, dyshidroses (pompholyx), seborrheic dermatitis, exfoliative dermatitis, solar dermatitis, stasis dermatitis, and anogenital and senile pruritus. Mechanism of Action Beclomethasone dipropionate is a corticosteroid and prodrug that is rapidly activated by hydrolysis to the active monoester, 17 monopropionate (17-BMP), which mediates anti-inflammatory actions. 17-BMP has been shown _in vitro_ to exhibit a binding affinity for the human glucocorticoid receptor which is approximately 13 times that of dexamethasone and 25 times that of beclomethasone dipropionate. Upon binding of the ligand, the glucocorticoid receptors dimerize and translocate into the nucleus, where they subsequently bind to glucocorticoid response elements (GRE) on glucocorticoid-responsive genes, leading to changes in transcription. There are several proposed mechanisms for the anti-inflammatory action of corticosteroids. Corticosteroids may work by increasing the transcription of genes coding for anti-inflammatory proteins, including lipocortin-1 and interleukin-10. Corticosteroids were also shown to inhibit the expression of multiple genes that encode pro-inflammatory factors, such as cytokines, chemokines, and adhesion molecules, that are activated during the chronic inflammatory process. This is thought to be due to the direct inhibitory interaction between activated glucocorticoid receptors and activated pro-inflammatory transcription factors, such as nuclear factor-kappa B and activator protein-1. Chronic inflammation is often characterized by enhanced expression of these transcription factors that bind to and activate coactivator molecules, which then acetylate core histones to switch on gene transcription to further amplify the inflammatory process. Corticosteroids suppress the multiple inflammatory gene expression by promoting histone deacetylation, resulting in tighter coiling of DNA and reduced access of transcription factors to their binding sites. Drug Background: Beclomethasone dipropionate is an inhaled corticosteroid (ICS) widely used for the treatment of asthma and chronic obstructive pulmonary disease (COPD) [1][2] - Mechanism of Action: Beclomethasone dipropionate exerts anti-inflammatory effects by inhibiting the activation of nuclear factor-κB (NF-κB), thereby reducing the production of pro-inflammatory cytokines (IL-4, IL-5, IL-8) and oxidative stress mediators (ROS, NO) [2] - Drug Delivery Advantage: Ultrasonic nebulization is an effective delivery method for Beclomethasone dipropionate to the airways, as it generates small aerosol droplets (mass median aerodynamic diameter: 3.2 μm) that can reach the lower respiratory tract, enhancing therapeutic efficacy in asthma models [1] |
| 分子式 |
C28H37CLO7
|
|
|---|---|---|
| 分子量 |
521.04
|
|
| 精确质量 |
520.222
|
|
| CAS号 |
5534-09-8
|
|
| 相关CAS号 |
Betamethasone dipropionate;5593-20-4;Beclometasone dipropionate-d10;Beclometasone;4419-39-0;Beclometasone dipropionate-d6;Beclometasone dipropionate monohydrate;77011-63-3
|
|
| PubChem CID |
21700
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 密度 |
1.3±0.1 g/cm3
|
|
| 沸点 |
630.5±55.0 °C at 760 mmHg
|
|
| 熔点 |
210ºC
|
|
| 闪点 |
335.1±31.5 °C
|
|
| 蒸汽压 |
0.0±4.2 mmHg at 25°C
|
|
| 折射率 |
1.564
|
|
| LogP |
4.59
|
|
| tPSA |
106.97
|
|
| 氢键供体(HBD)数目 |
1
|
|
| 氢键受体(HBA)数目 |
7
|
|
| 可旋转键数目(RBC) |
8
|
|
| 重原子数目 |
36
|
|
| 分子复杂度/Complexity |
1050
|
|
| 定义原子立体中心数目 |
8
|
|
| SMILES |
CCC(=O)OCC(=O)[C@]1([C@H](C[C@@H]2[C@@]1(C[C@@H]([C@]3([C@H]2CCC4=CC(=O)C=C[C@@]43C)Cl)O)C)C)OC(=O)CC
|
|
| InChi Key |
KUVIULQEHSCUHY-XYWKZLDCSA-N
|
|
| InChi Code |
InChI=1S/C28H37ClO7/c1-6-23(33)35-15-22(32)28(36-24(34)7-2)16(3)12-20-19-9-8-17-13-18(30)10-11-25(17,4)27(19,29)21(31)14-26(20,28)5/h10-11,13,16,19-21,31H,6-9,12,14-15H2,1-5H3/t16-,19-,20-,21-,25-,26-,27-,28-/m0/s1
|
|
| 化学名 |
(8S,9R,10S,11S,13S,14S,16S,17R)-9-chloro-11-hydroxy-10,13,16-trimethyl-3-oxo-17-[2-(propionyloxy)acetyl]-6,7,8,9,10,11,12,13,14,15,16,17-dodecahydro-3H-cyclopenta[a]phenanthren-17-yl propionate
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (4.80 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (4.80 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL 澄清 DMSO 储备液加入到 900 μL 玉米油中并混合均匀。 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.9192 mL | 9.5962 mL | 19.1924 mL | |
| 5 mM | 0.3838 mL | 1.9192 mL | 3.8385 mL | |
| 10 mM | 0.1919 mL | 0.9596 mL | 1.9192 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。