| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| Other Sizes |
|
| 靶点 |
Penicillin-binding proteins (PBPs); bacterial cell wall synthesis.
|
|---|---|
| 体外研究 (In Vitro) |
Ceftobiprole (Ro 63-9141) 的 MIC90 值分别为 0.25、2 和 2 mcg/mL,使其对主要革兰氏阳性菌有效,如粪肠球菌、耐甲氧西林金黄色葡萄球菌和肺炎链球菌 (PRSP)。抗生素头孢比罗罗的最低抑菌浓度 (MIC) 为 2 μg/ml,在体外对多种临床分离的耐甲氧西林金黄色葡萄球菌 (CA-MRSA)、金黄色葡萄球菌 (VISA) 和金黄色葡萄球菌 (VISA) 也表现出强大的作用。金黄色葡萄球菌(VRSA)[1]。头孢比罗罗的 MIC 范围为 0.12 至 4 mg/L(只有一种耐药菌株的 MIC 为 4 mg/L),对金黄色葡萄球菌表现出很强的活性。此外,头孢比普罗对甲氧西林敏感金黄色葡萄球菌(MSSA)菌株的 MIC50 和 MIC90 为 0.5 mg/L,是 MRSA 菌株(1 mg/L)的两倍。此外,与 PVL-MRSA 相比,头孢比罗罗对 Panton-Valentine 杀白细胞素 (PVL) + MRSA 的 MIC50 和 MIC90 略高,分别为 0.5 mg/L 和 1 mg/L(MIC50 和 MIC90 为 1 mg/L)[2]。
|
| 体内研究 (In Vivo) |
头孢比普酯是一种抗菌药物,适用于治疗成人患者的金黄色葡萄球菌血流感染(菌血症)(SAB),包括合并右侧感染性心内膜炎的患者。该药物还适用于治疗成人患者的急性细菌性皮肤及皮肤结构感染(ABSSSI),以及年龄≥3个月的成人和儿童患者的社区获得性细菌性肺炎(CABP)。在加拿大,该药的适应症还包括社区获得性和医院获得性肺炎(不包括呼吸机相关性肺炎)的治疗。
在一项中性粒细胞减少小鼠大腿感染模型中,头孢比普酯的治疗效果与药物游离血浆浓度超过金黄色葡萄球菌、肺炎链球菌和肠杆菌目细菌最低抑菌浓度(MIC)的时间相关。该药物对产生TEM、SHV或CTX-M家族超广谱β-内酰胺酶(ESBLs)的革兰阴性菌无效,对产丝氨酸碳青霉烯酶(如KPC)、B类金属β-内酰胺酶、高水平表达的C类(AmpC头孢菌素酶)以及Ambler D类β-内酰胺酶(包括碳青霉烯酶)的细菌亦无活性。头孢比普酯不适用于呼吸机相关性细菌肺炎(VABP)患者——临床试验显示,与对照治疗组相比,使用头孢比普酯治疗的VABP患者死亡率存在统计学意义上的显著升高。 |
| 药代性质 (ADME/PK) |
Absorption
Because ceftobiprole medocaril is administered intravenously, its bioavailability is 100%. The mean Cmax and AUC0-8h after multiple-dose administration are 33.0 µg/mL and 102 µg*h/mL, respectively. Route of Elimination Active [ceftobiprole] is eliminated primarily unchanged by renal excretion. Approximately 89% of the administered dose is recovered in the urine as active ceftobiprole (83%), the open-ring metabolite (5%) and ceftobiprole medocaril (<1%). Due to the significant degree of renal elimination, patients with renal impairment who are undergoing treatment with ceftobiprole may require lower doses. Volume of Distribution The steady-state volume of distribution of active [ceftobiprole] is 15.5-18.0 L, which approximates extracellular fluid volume in humans. Clearance The mean clearance of active [ceftobiprole] following multiple-dose administration is 4.98 L/h. Protein Binding Active [ceftobiprole] is minimally (16%) bound to plasma proteins. Metabolism / Metabolites Conversion of prodrug ceftobiprole medocaril to the active moiety ceftobiprole occurs rapidly and is mediated by non-specific plasma esterases. Ceftobiprole itself is minimally metabolized to a microbiologically inactive open-ring metabolite, which accounts for approximately 4% of the parent exposure in subject with a normal renal function. Biological Half-Life The half-life of active [ceftobiprole] following multiple-dose administration is approximately 3.3 hours. |
| 毒性/毒理 (Toxicokinetics/TK) |
For adults with SAB, the most common side effects of Zevtera included anemia, nausea, low levels of potassium in the blood (hypokalemia), vomiting, diarrhea, increased levels of certain liver tests (hepatic enzymes and bilirubin), increased blood creatinine, high blood pressure, low white blood cell count (leukopenia), fever, abdominal pain, fungal infection, headache and shortness of breath (dyspnea).
For adults with ABSSSI, the most common side effects of Zevtera included nausea, diarrhea, headache, injection site reaction, increased levels of hepatic enzymes, rash, vomiting and altered taste (dysgeusia). For adults with CABP, the most common side effects of Zevtera included nausea, increased levels of hepatic enzymes, vomiting, diarrhea, headache, rash, insomnia, abdominal pain, vein inflammation (phlebitis), high blood pressure and dizziness. For pediatric patients with CABP, the most common side effects of Zevtera included vomiting, headache, increased levels of hepatic enzymes, diarrhea, infusion site reaction, vein inflammation (phlebitis) and fever. Patients should not use Zevtera if they have a known history of severe hypersensitivity to ceftobiprole or any of the components of Zevtera, or other members of the cephalosporin antibacterial class. Zevtera comes with certain warnings and precautions such as increased mortality in ventilator-associated bacterial pneumonia patients (an unapproved use), hypersensitivity reactions, seizures and other central nervous system reactions and Clostridioides difficile-associated diarrhea. https://www.fda.gov/news-events/press-announcements/fda-approves-new-antibiotic-three-different-uses |
| 参考文献 |
[1]. Ceftobiprole, a Broad-Spectrum Cephalosporin With Activity against Methicillin-Resistant Staphylococcus aureus (MRSA). P T. 2008 Nov;33(11):631-41.
[2]. In vitro activity of ceftobiprole on 440 Staphylococcus aureus strains isolated from bronchopulmonary infections. Med Mal Infect. 2017 Mar;47(2):152-157. [3]. Efficacy of BAL5788, a prodrug of cephalosporin BAL9141, in a mouse model of acute pneumococcal pneumonia. Antimicrob Agents Chemother. 2004 Apr;48(4):1105-11. |
| 其他信息 |
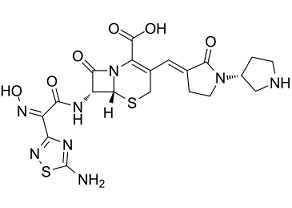
Ceftobiprole is a fifth-generation cephalosporin antibiotic having (E)-[(3'R)-2-oxo[1,3'-bipyrrolidin]-3-ylidene]methyl and [(2Z)-2-(5-amino-1,2,4-thiadiazol-3-yl)-2-(hydroxyimino)acetyl]amino side groups located at positions 3 and 7 respectively; developed for the treatment of hospital-acquired pneumonia (HAP, excluding ventilator-associated pneumonia, VAP) and community-acquired pneumonia (CAP). It has a role as an antimicrobial agent. It is a cephalosporin and a member of thiadiazoles.
Ceftobiprole is a cephalosporin antibiotic with activity against methicillin-resistant Staphylococcus aureus. It was discovered by Basilea Pharmaceutica and is being developed by Johnson & Johnson Pharmaceutical Research and Development. Ceftobiprole is the first cephalosporin to demonstrate clinical efficacy in patients with infections due to methicillin-resistant staphylococci and, if approved by regulatory authorities, is expected to be a useful addition to the armamentarium of agents for the treatment of complicated skin infections and pneumonia. Ceftobiprole is a broad-spectrum, fifth-generation, pyrrolidinone cephalosporin with antibacterial activity. Ceftobiprole binds to and inactivates penicillin-binding proteins (PBPs) located on the inner membrane of the bacterial cell wall. PBPs are enzymes involved in the terminal stages of assembling the bacterial cell wall and in reshaping the cell wall during growth and division. Inactivation of PBPs interferes with the cross-linkage of peptidoglycan chains necessary for bacterial cell wall strength and rigidity. This results in the weakening of the bacterial cell wall and causes cell lysis. Drug Indication For the treatment of serious bacterial infections in hospitalised patients. Mechanism of Action Cephalosporins, such as ceftobiprole, are bactericidal and have the same mode of action as other beta-lactam antibiotics (such as penicillins). Cephalosporins disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. The peptidoglycan layer is important for cell wall structural integrity, especially in Gram-positive organisms. The final transpeptidation step in the synthesis of the peptidoglycan is facilitated by transpeptidases known as penicillin binding proteins (PBPs). PBPs bind to the D-Ala-D-Ala at the end of muropeptides (peptidoglycan precursors) to crosslink the peptidoglycan. Beta-lactam antibiotics mimic this site and competitively inhibit PBP crosslinking of peptidoglycan. Pharmacodynamics Ceftobiprole, a cephalosporin antibiotic, is active against methicillin-resistant Staphylococcus aureus. Ceftobiprole medocaril is a cephalosporin. It has a role as a prodrug. Ceftobiprole medocaril is a prodrug of [ceftobiprole], a fifth-generation semisynthetic cephalosporin antibacterial. Ceftobiprole is a broad-spectrum agent with demonstrated activity against both Gram-positive and Gram-negative bacteria, including antibiotic-resistant strains of Staphylcoccus aureus (methicillin-resistant Staphylococcus aureus; MRSA). The EMA's Committee for Medicinal Products for Human Use (CHMP) adopted a negative opinion of ceftobiprole medocaril in February 2010, recommending the refusal of its marketing authorization in the European Union primarily due to data quality issues in pivotal clinical studies. It received its first approval in Canada in October 2017 for use in certain patients with bacterial pneumonia, and was subsequently approved in the United States with additional indications for skin and skin structure infections and bacteremia in April 2024. Ceftobiprole Medocaril Sodium is the sodim salt form of ceftobiprole medocaril, a water-soluble prodrug of ceftobiprole, a pyrrolidinone cephalosporin antibiotic, with bactericidal activity. Ceftobiprole binds to and inactivates penicillin-binding proteins (PBPs), enzymes involved in the terminal stages of bacterial cell wall assembly and cell wall reshaping during bacterial growth and division. This agent exhibits a broad spectrum of activity against gram-negative and gram-positive pathogens including methicillin-resistant S. aureus (MRSA), vancomycin-intermediate S. aureus (VISA) and vancomycin-resistant S. aureus (VRSA). Ceftobiprole is refractory to hydrolysis by class A and class C lactamases. Zevtera’s efficacy in treating SAB was evaluated in a randomized, controlled, double-blind, multinational, multicenter trial. In the trial, researchers randomly assigned 390 subjects to receive Zevtera (192 subjects) or daptomycin plus optional aztreonam [the comparator] (198 subjects). The primary measure of efficacy for this trial was the overall success (defined as survival, symptom improvement, S. aureus bacteremia bloodstream clearance, no new S. aureus bacteremia complications and no use of other potentially effective antibiotics) at the post-treatment evaluation visit, which occurred 70 days after being randomly assigned an antibiotic. A total of 69.8% of subjects who received Zevtera achieved overall success compared to 68.7% of subjects who received the comparator. Zevtera’s efficacy in treating ABSSSI was evaluated in a randomized, controlled, double-blind, multinational trial. In the trial, researchers randomly assigned 679 subjects to receive either Zevtera (335 subjects) or vancomycin plus aztreonam [the comparator] (344 subjects). The primary measure of efficacy was early clinical response 48-72 hours after start of treatment. Early clinical response required a reduction of the primary skin lesion by at least 20%, survival for at least 72 hours and the absence of additional antibacterial treatment or unplanned surgery. Of the subjects who received Zevtera, 91.3% achieved an early clinical response within the necessary timeframe compared to 88.1% of subjects who received the comparator. Zevtera’s efficacy in treating adult patients with CABP was evaluated in a randomized, controlled, double-blind, multinational, multicenter trial. In the trial, researchers randomly assigned 638 adults hospitalized with CABP and requiring IV antibacterial treatment for at least 3 days to receive either Zevtera (314 subjects) or ceftriaxone with optional linezolid [the comparator] (324 subjects). The primary measurement of efficacy were clinical cure rates at test-of-cure visit, which occurred 7-14 days after end-of-treatment. Of the subjects who received Zevtera, 76.4% achieved clinical cure compared to 79.3% of subjects who received the comparator. An additional analysis considered an earlier timepoint of clinical success at Day 3, which was 71% in patients receiving Zevtera and 71.1% in patients receiving the comparator. Given the similar course of CABP in adults and pediatric patients, today’s approval of Zevtera in pediatric patients three months to less than 18 years with CABP was supported by evidence from the CABP trial of Zevtera in adults and a trial in 138 pediatric subjects three months to less than 18 years of age with pneumonia. https://www.fda.gov/news-events/press-announcements/fda-approves-new-antibiotic-three-different-uses |
| 分子式 |
C20H22N8O6S2
|
|---|---|
| 分子量 |
534.56900
|
| 精确质量 |
534.11
|
| 元素分析 |
C, 44.94; H, 4.15; N, 20.96; O, 17.96; S, 12.00
|
| CAS号 |
209467-52-7
|
| 相关CAS号 |
252188-71-9 (medocaril);209467-52-7; 376653-43-9;
|
| PubChem CID |
135413542
|
| 外观&性状 |
Light yellow to yellow solid powder
|
| 密度 |
2.0±0.1 g/cm3
|
| 折射率 |
1.942
|
| LogP |
-2.69
|
| tPSA |
256.98
|
| 氢键供体(HBD)数目 |
5
|
| 氢键受体(HBA)数目 |
13
|
| 可旋转键数目(RBC) |
6
|
| 重原子数目 |
36
|
| 分子复杂度/Complexity |
1100
|
| 定义原子立体中心数目 |
3
|
| SMILES |
O=C(C(N12)=C(/C=C3C(N([C@H]4CNCC4)CC/3)=O)CS[C@]2([H])[C@H](NC(/C(C5=NSC(N)=N5)=N\O)=O)C1=O)O
|
| InChi Key |
VOAZJEPQLGBXGO-SDAWRPRTSA-N
|
| InChi Code |
InChI=1S/C20H22N8O6S2/c21-20-24-14(26-36-20)11(25-34)15(29)23-12-17(31)28-13(19(32)33)9(7-35-18(12)28)5-8-2-4-27(16(8)30)10-1-3-22-6-10/h5,10,12,18,22,34H,1-4,6-7H2,(H,23,29)(H,32,33)(H2,21,24,26)/b8-5+,25-11-/t10-,12-,18-/m1/s1
|
| 化学名 |
(6R,7R)-7-((Z)-2-(5-amino-1,2,4-thiadiazol-3-yl)-2-(hydroxyimino)acetamido)-8-oxo-3-((E)-((R)-2-oxo-[1,3'-bipyrrolidin]-3-ylidene)methyl)-5-thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylic
acid
|
| 别名 |
Ro 63-9141; Ro-63-9141; Ro63-9141; BAL 9141;Ceftobiprole medocaril; Ceftobiprole medocaril sodium; BAL5788; Ro 65-5788; (6R,7R)-7-[[(2Z)-2-(5-amino-1,2,4-thiadiazol-3-yl)-2-hydroxyiminoacetyl]amino]-3-[(E)-[1-[(3R)-1-[(5-methyl-2-oxo-1,3-dioxol-4-yl)methoxycarbonyl]pyrrolidin-3-yl]-2-oxopyrrolidin-3-ylidene]methyl]-8-oxo-5-thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid; AC1OCFF8; Zeftera; UNII-5T97333YZK; BAL-9141; BAL9141.
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 该产品在溶液状态不稳定,请现配现用。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ~4.95 mg/mL (~9.26 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 0.5 mg/mL (0.94 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 5.0 mg/mL澄清DMSO储备液加入400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 0.5 mg/mL (0.94 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 5.0 mg/mL 澄清 DMSO 储备液加入 900 μL 20% SBE-β-CD 生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 0.5 mg/mL (0.94 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.8707 mL | 9.3533 mL | 18.7066 mL | |
| 5 mM | 0.3741 mL | 1.8707 mL | 3.7413 mL | |
| 10 mM | 0.1871 mL | 0.9353 mL | 1.8707 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。