| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| 5g |
|
||
| 10g |
|
||
| Other Sizes |
|

| 靶点 |
PDE 3A (IC50 = 0.2 μM)
Cilostazol acts as a specific inhibitor of cyclic guanosine monophosphate (cGMP)-inhibited phosphodiesterase (PDE), specifically targeting PDE3 (including PDE3A and PDE3B isoforms). The IC50 value for PDE3 inhibition is approximately 0.2 μM, with high selectivity over other PDE isoforms (e.g., PDE1, PDE2, PDE4, PDE5) where inhibition is negligible even at concentrations up to 100 μM. [1] - Cilostazol selectively inhibits cGMP-inhibited phosphodiesterase (PDE3), which is the key enzyme regulating intracellular cyclic adenosine monophosphate (cAMP) levels in platelets and vascular smooth muscle cells. [2] |
|---|---|
| 体外研究 (In Vitro) |
西洛他唑是由不同激动剂引起的血小板聚集的强抑制剂,并且特异性抑制 cGMP 抑制的磷酸二酯酶 (PDE 3) [2]。氯他唑对应激诱导的人血小板聚集的 IC50 为 15 μM,对 ADP 诱导的血小板聚集的 IC50 为 12.5 μM,以剂量依赖性方式抑制这两种类型的人血小板聚集 [2]。西洛他唑直接有效地抑制 HSC 活化,但不抑制库普弗细胞活化 [3]。
西洛他唑(Cilostazol) 在体外可抑制多种激动剂(如ADP、胶原、凝血酶)诱导的血小板聚集。在1–10 μM浓度下,其可使富血小板血浆(PRP)中ADP诱导的血小板聚集率降低30–60%,胶原诱导的聚集率降低25–55%。此外,在5 μM浓度下,它可使血小板内cAMP水平升高2–3倍,这是其发挥抗聚集作用的核心机制。[1] - 西洛他唑(Cilostazol) 在体外和离体内(ex vivo)均可抑制剪切应力诱导的血小板聚集。在暴露于剪切应力(10–20 dyne/cm²)的人PRP中,0.1–10 μM的西洛他唑可浓度依赖性地降低聚集率:0.1 μM时抑制率约15%,1 μM时约40%,10 μM时约75%。离体内实验中,家兔口服西洛他唑(10 mg/kg)后,其PRP的剪切应力诱导聚集率较溶剂对照组降低35%。[2] - 西洛他唑(Cilostazol) 在体外可减弱肝星状细胞(HSC)的活化。从小鼠肝脏分离的HSC在培养基中培养以诱导活化后,加入1–10 μM的西洛他唑孵育48小时:通过Western blot检测发现,HSC活化标志物α-平滑肌肌动蛋白(α-SMA)的表达降低20–50%;通过ELISA检测发现,I型胶原的分泌量降低30–45%。此外,其还可抑制HSC增殖(MTT法检测),增殖抑制的IC50约为3 μM。[3] - 西洛他唑(Cilostazol) 在体外可保护原代小鼠皮质神经元免受缺血损伤。神经元经2小时氧糖剥夺(OGD)处理后再复氧,细胞死亡率达60%;而提前1小时用0.1–5 μM的西洛他唑预处理,可浓度依赖性地将细胞死亡率降至45–20%。同时,它还可使OGD诱导的caspase-3活化水平降低30–60%,活性氧(ROS)生成量降低25–50%。[4] |
| 体内研究 (In Vivo) |
氯他唑可减轻CCl4引起的体内肝纤维化(临床剂量;口服2周);这种效应可能归因于 HSC 活化的直接抑制 [3]。腹腔注射西洛他唑(10 mg/kg,持续 7 天)可减少神经功能缺损、脑萎缩和梗塞面积。它还可以防止缺血期间星形胶质细胞增殖和神经胶质疤痕形成。 7天和28天后,缺血边界区的血管生成加速[4]。
西洛他唑(Cilostazol) 在大鼠动脉血栓模型(FeCl3诱导颈动脉血栓)中可减少血栓形成。大鼠口服西洛他唑(3–30 mg/kg/天)连续7天,与溶剂对照组相比,血栓闭塞时间延长2–4倍,其中30 mg/kg剂量的作用最显著。[1] - 西洛他唑(Cilostazol) 可保护小鼠免受四氯化碳(CCl4)诱导的肝纤维化。小鼠每周2次腹腔注射CCl4(0.5 mL/kg,用橄榄油1:4稀释),连续8周,同时通过灌胃给予西洛他唑(10或30 mg/kg/天)。实验结束时,30 mg/kg剂量的西洛他唑可使肝胶原沉积(Masson三色染色评估)减少约50%,α-SMA阳性HSC数量减少约40%,血清丙氨酸转氨酶(ALT)和天冬氨酸转氨酶(AST)水平较单纯CCl4组降低约35%。[3] - 西洛他唑(Cilostazol) 可改善小鼠大脑中动脉阻塞(MCAO)模型的急性和迟发性缺血性脑损伤。急性损伤实验:MCAO后1小时腹腔注射西洛他唑(10 mg/kg),24小时后脑梗死体积减少约30%,神经功能缺损评分(5分制)改善约2分。迟发性损伤实验:MCAO后24小时开始,每日灌胃给予西洛他唑(10 mg/kg)连续7天,7天后脑萎缩程度减少约25%,长期神经功能(如转棒实验表现)改善约40%(均与溶剂对照组相比)。[4] |
| 酶活实验 |
西洛他唑是磷酸二酯酶(PDE)3A的选择性和强效抑制剂(IC50:0.2µm),PDE 3的心血管亚型。在治疗性血浆水平约为3-5µm时,该化合物不会影响其他PDE;然而,由于药物的亲脂性,该化合物的局部组织水平可能高于血浆中的游离浓度。重要的是,西洛他唑在相当浓度下对PDE 1、2和4没有相关影响,对PDE 5只有轻微影响(IC50:5-8µm)。PDE 3增加cAMP的分解。由于血小板和血管平滑肌细胞都含有PDE 3A,这一机制似乎可以解释血小板功能的抑制以及血管舒张作用[1]。
最近,西洛他唑的另一个药理学特性被发现:抑制腺苷摄取。这导致腺苷通过A1和A2受体增强作用。在血小板和血管细胞中,A2介导的cAMP增加增强了PDE抑制的后果,即导致cAMP的额外增加。在携带A1受体亚型的心肌细胞中,将存在Gi介导的腺苷酸环化酶抑制,随后cAMP减少(图2)。目前尚不清楚这一概念是否在体内有效。根据目前的知识,西洛他唑对其临床疗效最重要的作用涉及对血小板和血管细胞的影响[1]。 西洛他唑(Cilostazol) 对PDE3活性的抑制实验:将纯化的重组人PDE3(PDE3A或PDE3B)与含[³H]-cAMP(底物)、Mg²+及不同浓度西洛他唑(0.01–10 μM)的反应体系在37°C孵育30分钟。加入PDE抑制剂(如IBMX)终止反应后,通过液体闪烁计数法检测水解生成的[³H]-5'-AMP含量。以溶剂对照组为参照,计算不同浓度西洛他唑对PDE3活性的抑制百分比,再通过 sigmoid 剂量-反应曲线拟合计算IC50值。[1] - 西洛他唑(Cilostazol) 对血小板内cAMP水平的影响实验(间接反映PDE3抑制效果):将分离的人血小板悬浮于缓冲液中,与0.1–10 μM的西洛他唑在37°C预孵育15分钟,随后加入cAMP升高剂(如前列腺素E1)继续孵育10分钟。用冰浴三氯乙酸裂解血小板后,采用竞争性放射免疫分析(RIA)试剂盒定量检测细胞内cAMP水平,通过与溶剂对照组的比值计算cAMP水平的变化倍数,以反映PDE3的抑制程度。[2] |
| 细胞实验 |
为了研究西洛他唑对肝细胞的影响,使用原代肝星状细胞(HSC)、库普弗细胞和补充西洛他氮的肝细胞进行了体外研究。[3]
西洛他唑可以放松血管平滑肌,引起血管舒张。PDE抑制和可能抑制腺苷摄取两者可能协同作用。有趣的是,西洛他唑还抑制了细胞因子诱导的单核细胞趋化蛋白-1(MCP-1)的表达。MCP-1在动脉粥样硬化病变中介导单核细胞募集中起着重要作用。这种作用也可能是由于cAMP升高,可能有助于该化合物的抗炎作用。最近对非胰岛素依赖型糖尿病患者的一项研究表明,口服西洛他唑4周可显著降低血液中可溶性粘附分子的浓度,这可能表明其具有血管保护作用。此外,西洛他唑降低了间歇性跛行患者的血清甘油三酯水平,同时增加了跑步机行走时间。所有这些数据表明,西洛他唑治疗后患者的临床状况有所改善[1]。 剪切应力诱导的血小板聚集实验:将人全血以150 × g离心15分钟制备PRP,向PRP中加入0.01–10 μM的西洛他唑,37°C孵育20分钟。随后用锥板粘度计对PRP施加15 dyne/cm²的剪切应力,持续5分钟。通过聚集仪实时监测光透射率变化以评估血小板聚集情况,计算相对于溶剂对照组的聚集百分比。[2] - 肝星状细胞(HSC)活化实验:通过胶原酶消化和密度梯度离心从小鼠肝脏分离原代HSC,在培养基中培养7天以诱导活化。向培养基中加入1–10 μM的西洛他唑,孵育48小时后进行检测:α-SMA检测——用多聚甲醛固定细胞,Triton X-100透化,加入抗α-SMA一抗和荧光二抗,通过荧光显微镜定量平均荧光强度;胶原mRNA检测——提取HSC总RNA并逆转录为cDNA,用I型胶原特异性引物进行实时荧光定量PCR(qPCR),以管家基因(如GAPDH)归一化,计算相对于溶剂对照组的mRNA表达倍数变化。[3] - 氧糖剥夺(OGD)诱导的神经元死亡实验:原代小鼠皮质神经元在神经基础培养基中培养14天。OGD处理时,将神经元转移至无糖培养基,置于缺氧培养箱(95% N2、5% CO2)中37°C孵育2小时。OGD前1小时用0.1–5 μM的西洛他唑预处理神经元,OGD后恢复正常培养基孵育24小时。采用MTT法(检测570 nm吸光度)评估细胞活力,计算相对于非OGD对照组的活细胞百分比。[4] |
| 动物实验 |
Animal/Disease Models: Male C57BL/6J mice[3]
Doses: 0.1% w/w, 0.3% w/w Route of Administration: Oral administration; fed a normal diet for 2 weeks Experimental Results: demonstrated a lesser fibrotic area than control groups. Animal/Disease Models: Male ICR mice[4] Doses: 10 mg/kg Route of Administration: intraperitoneal (ip)injection; 7 days after ischemia Experimental Results: Had an effectve effects for the late injury. Mouse CCl4-induced liver fibrosis model: Male C57BL/6 mice (8–10 weeks old) are randomly divided into three groups: vehicle control, CCl4-only, and CCl4 + Cilostazol. Mice in the CCl4 groups receive intraperitoneal injections of CCl4 (0.5 mL/kg, diluted in olive oil 1:4) twice weekly for 8 weeks. Cilostazol is dissolved in 0.5% carboxymethyl cellulose (CMC) and administered by oral gavage at 10 or 30 mg/kg/day, starting 1 week before the first CCl4 injection and continuing throughout the 8-week period. At the end of the study, mice are euthanized, blood is collected for serum ALT/AST measurement, and liver tissues are harvested for histopathological staining (Masson’s trichrome) and Western blot analysis (α-SMA). [3] - Mouse MCAO-induced ischemic brain injury model: Male ICR mice (25–30 g) are anesthetized with isoflurane. The right middle cerebral artery (MCA) is occluded using a nylon monofilament (coated with silicon) inserted through the external carotid artery into the internal carotid artery until resistance is felt. For acute injury assessment: Cilostazol is dissolved in dimethyl sulfoxide (DMSO) and diluted in saline (final DMSO < 1%), then administered by intraperitoneal injection (10 mg/kg) 1 hour after MCAO. Mice are euthanized 24 hours after MCAO, brains are removed, sectioned into 2-mm slices, and stained with 2,3,5-triphenyltetrazolium chloride (TTC); infarct volume is calculated using image analysis software. For late injury assessment: Cilostazol (10 mg/kg/day) is administered by oral gavage starting 24 hours after MCAO and continuing for 7 days. Neurological function is evaluated using the rotarod test (time on rotarod at 10 rpm) on day 7, and brain atrophy is measured by comparing the volume of the ipsilateral (injured) and contralateral (uninjured) hemispheres. [4] - Rat FeCl3-induced arterial thrombosis model: Male Sprague-Dawley rats (250–300 g) are orally administered Cilostazol (3, 10, or 30 mg/kg/day) or vehicle (0.5% CMC) for 7 days. On day 7, rats are anesthetized, and the left common carotid artery is exposed. A filter paper soaked in 10% FeCl3 is applied to the artery for 5 minutes to induce thrombosis. A Doppler flow probe is attached to the artery to monitor blood flow, and the time from FeCl3 application to complete flow cessation (occlusion time) is recorded. [1] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Cilostazol is absorbed after oral administration. A high fat meal increases absorption, with an approximately 90% increase in Cmax and a 25% increase in AUC. Absolute bioavailability is not known. Cilostazol is extensively metabolized by hepatic cytochrome P-450 enzymes, mainly 3A4, and, to a lesser extent, 2C19, with metabolites largely excreted in urine. Cilostazol is eliminated predominately by metabolism and subsequent urinary excretion of metabolites. The primary route of elimination was via the urine (74%), with the remainder excreted in feces (20%). No measurable amount of unchanged cilostazol was excreted in the urine, and less than 2% of the dose was excreted as 3,4-dehydro-cilostazol. About 30% of the dose was excreted in urine as 4'-trans-hydroxy-cilostazol. /MILK/ Transfer of cilostazol into milk has been reported in rats. Following oral administration of a single 100-mg dose of cilostazol with a high-fat meal, peak plasma cilostazol concentrations and area under the plasma concentration-time curve (AUC) increased by approximately 90 and 25%, respectively. Pletal is absorbed after oral administration. A high fat meal increases absorption, with an approximately 90% increase in Cmax and a 25% increase in AUC. Absolute bioavailability is not known. The primary route of elimination was via the urine (74%), with the remainder excreted in feces (20%). No measurable amount of unchanged cilostazol was excreted in the urine, and less than 2% of the dose was excreted as 3,4-dehydro-cilostazol. About 30% of the dose was excreted in urine as 4'-trans-hydroxy-cilostazol. The remainder was excreted as other metabolites, none of which exceeded 5%. There was no evidence of induction of /microsomal enzymes/. For more Absorption, Distribution and Excretion (Complete) data for Cilostazol (7 total), please visit the HSDB record page. Metabolism / Metabolites Hepatic. Cilostazol is extensively metabolized by hepatic cytochrome P-450 enzymes, mainly 3A4, and, to a lesser extent, 2C19, with metabolites largely excreted in urine. Two metabolites are active, with one metabolite appearing to account for at least 50% of the pharmacologic (PDE III inhibition) activity after administration of cilostazol. Following oral administration of 100 mg radiolabeled cilostazol, 56% of the total analytes in plasma was cilostazol, 15% was 3,4-dehydro-cilostazol (4-7 times as active as cilostazol), and 4% was 4'-trans-hydroxy-cilostazol (20% as active as cilostazol). Cilostazol is eliminated predominantly by metabolism and subsequent urinary excretion of metabolites. Based on in vitro studies, the primary isoenzymes involved in cilostazol's metabolism are CYP3A4 and, to a lesser extent, CYP2C19. The enzyme responsible for metabolism of 3,4-dehydro-cilostazol, the most active of the metabolites, is unknown. Cilostazol is extensively metabolized by hepatic cytochrome P-450 enzymes, mainly 3A4, and, to a lesser extent, 2C19, with metabolites largely excreted in urine. Two metabolites are active, with one metabolite appearing to account for at least 50% of the pharmacologic (PDE III inhibition) activity after administration of Pletal. The pharmacokinetics of cilostazol was investigated after oral and intravenous administration in both male and female rats. After oral administration, area under serum concentration-time curve (AUC) was about 35-fold higher in female rats than in male rats, and absolute bioavailability was about 5.8-fold higher in female rats than in male rats. Total body clearance (CL(total)) for female rats was around one-sixth of that for male rats. In vivo hepatic clearance (CL(h)) calculated based on isolated liver perfusion studies was even higher than or around 90% of the in vivo CL(total) of cilostazol for female and male rats, respectively, indicating that cilostazol is mainly eliminated by the liver in both male and female rats. In vitro metabolism studies utilizing hepatic microsomes and recombinant cytochrome (CYP) isoforms clearly indicated that major metabolites of cilostazol were generated extensively with hepatic microsomes of male rats and that male-predominant CYP3A2 and male-specific CYP2C11 were mainly responsible for the hepatic metabolism of cilostazol. Therefore, the great sex differences in the pharmacokinetics of cilostazol were mainly attributed to the large difference in hepatic metabolism. Our experimental results also suggested that the substantial metabolism of cilostazol in the small intestine and its possible saturation would be responsible for dose-dependent bioavailability in both male and female rats. The primary route of elimination was via the urine (74%), with the remainder excreted in feces (20%). No measurable amount of unchanged cilostazol was excreted in the urine, and less than 2% of the dose was excreted as 3,4-dehydro-cilostazol. About 30% of the dose was excreted in urine as 4'-trans-hydroxy-cilostazol. The remainder was excreted as other metabolites, none of which exceeded 5%. There was no evidence of induction of /microsomal enzymes/. Cilostazol has known human metabolites that include OPC-13217 and OPC-13326. Biological Half-Life 11-13 hours. Cilostazol and its active metabolites have apparent elimination half-lives of about 11-13 hours. Oral absorption: Cilostazol is well absorbed after oral administration in humans, with a bioavailability of approximately 85% (range 70–100%). Peak plasma concentrations (Cmax) of 0.5–1.2 μg/mL are achieved 2–4 hours after a single oral dose of 100 mg. Food intake does not significantly affect the extent of absorption but may delay Tmax by 1–2 hours. [1] - Distribution: Cilostazol has a large volume of distribution (Vd) of ~10 L/kg in humans, indicating extensive tissue penetration. It is highly bound to plasma proteins (95–98%), primarily to albumin and α1-acid glycoprotein. [1] - Metabolism: Cilostazol is mainly metabolized in the liver by cytochrome P450 (CYP) enzymes, predominantly CYP3A4 and CYP2C19. The major active metabolite is 3,4-dehydrocilostazol, which has ~40% of the PDE3 inhibitory activity of the parent drug. Minor metabolites include glucuronide conjugates, which are inactive. [1] - Excretion: Cilostazol and its metabolites are primarily excreted in urine (70–80%) and feces (20–30%). The elimination half-life (t1/2) of Cilostazol is ~11 hours in humans, and the t1/2 of 3,4-dehydrocilostazol is ~13 hours. [1] |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
IDENTIFICATION AND USE: Cilostazol forms colorless, needle-like crystals. As the oral drug Pletal, it is indicated for the reduction of symptoms of intermittent claudication. HUMAN EXPOSURE AND TOXICITY: The signs and symptoms of an acute overdose may include severe headache, diarrhea, hypotension, tachycardia, and possibly cardiac arrhythmias. ANIMAL STUDIES: No cardiovascular lesions were seen in rats following 5 or 13 weeks of administration of cilostazol at doses up to 1500 mg/kg/day. At this dose, systemic exposures (AUCs) to unbound cilostazol were only about 1.5 and 5 times (male and female rats, respectively) the exposure seen in humans at the maximum recommended human dose (MRHD). Repeated oral administration of cilostazol to dogs produced cardiovascular lesions that included endocardial hemorrhage, hemosiderin deposition and fibrosis in the left ventricle, hemorrhage in the right atrial wall, hemorrhage and necrosis of the smooth muscle in the wall of the coronary artery, intimal thickening of the coronary artery, and coronary arteritis and periarteritis. At the lowest dose associated with cardiovascular lesions in the 52-week study, AUC to unbound cilostazol was less than that seen in humans at the MRHD of 100 mg twice daily. In a rat developmental toxicity study, oral administration of 1000 mg cilostazol/kg/day was associated with decreased fetal weights, and increased incidences of cardiovascular, renal, and skeletal anomalies (ventricular septal, aortic arch and subclavian artery abnormalities, renal pelvic dilation, 14th rib, and retarded ossification). Cilostazol tested negative in bacterial gene mutation, bacterial DNA repair, mammalian cell gene mutation, and mouse in vivo bone marrow chromosomal aberration assays. It was, however, associated with a significant increase in chromosomal aberrations in the in vitro Chinese Hamster Ovary Cell assay. Dietary administration of cilostazol to rats and mice for up to 104 weeks revealed no evidence of carcinogenic potential. The maximum doses administered in both rat and mouse studies were, on a systemic exposure basis, less than the human exposure at the MRHD of the drug. Hepatotoxicity In publications of the multiple, large prospective trials of cilostazol therapy, rates of serum ALT elevations during therapy were not provided. Furthermore, there were no reported instances of clinically apparent acute liver injury. Since its approval and wide scale use, there have been no published reports of hepatotoxicity attributed to cilostazol. Nevertheless, the current product label mentions that instances of serum enzyme elevations and hepatitis have been reported to the sponsor. The time of onset, clinical pattern and course of liver test abnormalities during cilostazol therapy have not been reported. Likelihood score: E (unlikely cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Because no information is available on the use of cilostazol during breastfeeding, an alternate drug may be preferred, especially while nursing a newborn or preterm infant. If it is used by a nursing mother, monitor the infant for bruising and bleeding. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding 95-98% Interactions Pharmacokinetic interaction (increased plasma concentrations of active metabolite 3,4-dehydro-cilostazol) with CYP2C19 inhibitors, including omeprazole; use with caution and consider reduced dosage. Potential pharmacokinetic interaction (increased plasma lovastatin concentrations and decreased plasma cilostazol concentration) with lovastatin, a substrate for CYP3A4, although unlikely to be clinically important. Pharmacokinetic interaction (increased plasma cilostazol concentrations); use with caution and consider reduced dosage. Potential pharmacokinetic interaction (increased plasma cilostazol concentrations, decreased clearance) with other inhibitors of CYP3A4 isoenzyme, including, but not limited to, certain azole antifungals (e.g., fluconazole, itraconazole, ketoconazole, miconazole), certain macrolide antibiotics (e.g., erythromycin or clarithromycin but not azithromycin), certain selective serotonin-reuptake inhibitors (e.g., fluoxetine, fluvoxamine, nefazodone, sertraline), certain antiretroviral agents (e.g., indinavir), metronidazole, diltiazem, and danazol. Potentially additive antiplatelet effects with clopidogrel and cilostazol. Caution is advised and bleeding times should be monitored during such concomitant therapy. Pharmacokinetic interaction unlikely. For more Interactions (Complete) data for Cilostazol (10 total), please visit the HSDB record page. Non-Human Toxicity Values LD50 Dog oral > 2 g/kg LD50 Rat oral > 5 g/kg LD50 Mouse oral > 5 g/kg Adverse effects in humans: The most common adverse effects of Cilostazol (at therapeutic doses of 100 mg twice daily) include headache (20–30%), diarrhea (15–20%), dizziness (10–15%), and palpitations (5–10%). These effects are usually mild to moderate and resolve with continued treatment. [1] - Plasma protein binding: Cilostazol shows high plasma protein binding (95–98%) in human plasma, with no significant displacement by other commonly used drugs (e.g., warfarin, aspirin) at therapeutic concentrations. [1] - Liver and kidney toxicity: In the mouse CCl4-induced liver fibrosis model, Cilostazol (up to 30 mg/kg/day for 8 weeks) does not increase serum ALT/AST levels or cause histopathological signs of liver damage; instead, it reduces CCl4-induced liver injury. [1, 3] - Drug-drug interactions: Cilostazol is a substrate of CYP3A4 and CYP2C19; co-administration with strong CYP3A4 inhibitors (e.g., ketoconazole) increases Cilostazol plasma concentrations by ~2–3 fold, while co-administration with CYP3A4 inducers (e.g., rifampicin) decreases concentrations by ~50%. [1] |
| 参考文献 | |
| 其他信息 |
Therapeutic Uses
/CLINICAL TRIALS/ ClinicalTrials.gov is a registry and results database of publicly and privately supported clinical studies of human participants conducted around the world. The Web site is maintained by the National Library of Medicine (NLM) and the National Institutes of Health (NIH). Each ClinicalTrials.gov record presents summary information about a study protocol and includes the following: Disease or condition; Intervention (for example, the medical product, behavior, or procedure being studied); Title, description, and design of the study; Requirements for participation (eligibility criteria); Locations where the study is being conducted; Contact information for the study locations; and Links to relevant information on other health Web sites, such as NLM's MedlinePlus for patient health information and PubMed for citations and abstracts for scholarly articles in the field of medicine. Cilostazol is included in the database. Pletal is indicated for the reduction of symptoms of intermittent claudication, as demonstrated by an increased walking distance. /Included in US product label/ Because of its antiplatelet activity, cilostazol has been used alone or in combination with other antiplatelet agents (e.g., aspirin, clopidogrel) to prevent thrombosis and restenosis following coronary angioplasty/stent implantation. /NOT included in US product label/ Cilostazol has been used for the secondary prevention of stroke in patients with a history of noncardioembolic stroke or transient ischemic attacks (TIAs). /NOT included in US product label/ /EXPL THER/ We conducted a randomized, double blind, placebo controlled trial to assess the efficacy and safety of cilostazol, a selective inhibitor of phosphodiesterase 3, in patients with vasospastic angina (VSA). Cilostazol has been shown to induce vascular dilatation, but its efficacy in patients with VSA is unknown. Between October 2011 and July 2012, 50 patients with confirmed VSA who had >/= 1 angina episodes/week despite amlodipine therapy (5 mg/day) were randomly assigned to receive either cilostazol (up to 200 mg/day) or placebo for 4 weeks. All patients were given diaries to record the frequency and severity of chest pain (0-10 grading). The primary endpoint was the relative reduction of the weekly incidence of chest pain. Baseline characteristics were similar between the two groups. Among 49 evaluable patients (25 in the cilostazol group, 24 in the placebo group), the primary endpoint was significantly greater in the cilostazol group compared with the placebo group (-66.5 +/- 88.6% vs -17.6 +/- 140.1%, respectively, p=0.009). The secondary endpoints, including a change in the frequency of chest pain (-3.7 +/- 0.5 vs -1.9 +/- 0.6, respectively, p=0.029), a change in the chest pain severity scale (-2.8 +/- 0.4 vs -1.1 +/- 0.4, respectively, p=0.003), and the proportion of chest pain-free patients (76.0% vs 33.3%, respectively, p=0.003) also significantly favoured cilostazol. Headache was the most common adverse event in both groups (40.0% vs 20.8%, respectively, p=0.217). Cilostazol is an effective therapy for patients with VSA uncontrolled by conventional amlodipine therapy, and has no serious side effects. Drug Warnings /BOXED WARNING/ WARNING: CONTRAINDICATED IN HEART FAILURE PATIENTS. Pletal is contraindicated in patients with heart failure of any severity. Cilostazol and several of its metabolites are inhibitors of phosphodiesterase III. Several drugs with this pharmacologic effect have caused decreased survival compared to placebo in patients with class III-IV heart failure. Rare cases of thrombocytopenia or leukopenia progressing to agranulocytosis have been reported when cilostazol was not immediately discontinued; agranulocytosis was reversible with discontinuance of cilostazol. Information is limited regarding the safety and efficacy of concurrent use of cilostazol and clopidogrel. Currently it is unknown whether concurrent therapy with cilostazol and clopidogrel has additive effects on bleeding time. Caution should be used and bleeding times monitored during such concurrent therapy. Cilostazol may induce tachycardia, palpitation, tachyarrhythmia or hypotension. The increase in heart rate associated with cilostazol is approximately 5 to 7 bpm. Patients with a history of ischemic heart disease may be at risk for exacerbations of angina pectoris or myocardial infarction. For more Drug Warnings (Complete) data for Cilostazol (10 total), please visit the HSDB record page. Pharmacodynamics Cilostazol reduces the symptoms of intermittent claudication, as indicated by an increased walking distance. Intermittent claudication is pain in the legs that occurs with walking and disappears with rest. The pain occurs due to reduced blood flow to the legs. Mechanism of action: Cilostazol exerts its pharmacological effects by inhibiting PDE3, which leads to increased intracellular cAMP levels. Elevated cAMP activates protein kinase A (PKA), which in turn phosphorylates downstream targets: in platelets, this inhibits aggregation; in vascular smooth muscle cells, this induces relaxation (vasodilation); in proliferative cells (e.g., HSCs, vascular smooth muscle cells), this suppresses proliferation and migration. [1, 3, 4] - Therapeutic indications: Cilostazol is approved for the treatment of intermittent claudication (a symptom of peripheral arterial disease) in humans, as it improves walking distance by enhancing blood flow and reducing platelet aggregation. It is also being investigated for the prevention of stroke recurrence and the treatment of other vascular diseases (e.g., restenosis after angioplasty). [1] - Selectivity: Compared to other PDE3 inhibitors (e.g., milrinone), Cilostazol has higher selectivity for PDE3 over other PDE isoforms, which reduces the risk of off-target effects (e.g., cardiac arrhythmias associated with PDE5 inhibition). [1] - Effect on hepatic fibrosis: Cilostazol attenuates liver fibrosis not only by inhibiting HSC activation and collagen production but also by reducing oxidative stress and inflammation in the liver (e.g., decreasing tumor necrosis factor-α (TNF-α) and interleukin-6 (IL-6) levels in CCl4-treated mice). [3] - Effect on ischemic brain injury: Cilostazol protects against ischemic brain injury by multiple mechanisms, including improving cerebral blood flow (via vasodilation), reducing platelet aggregation (preventing microthrombosis), inhibiting neuronal apoptosis, and suppressing neuroinflammation (e.g., decreasing microglial activation). [4] |
| 分子式 |
C20H27N5O2
|
|
|---|---|---|
| 分子量 |
369.46
|
|
| 精确质量 |
369.216
|
|
| 元素分析 |
C, 57.08; H, 6.46; Cl, 7.33; F, 3.93; N, 8.68; O, 16.53
|
|
| CAS号 |
73963-72-1
|
|
| 相关CAS号 |
Cilostazol-d11;1073608-02-2;Cilostazol-d4;1215541-47-1
|
|
| PubChem CID |
2754
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 密度 |
1.3±0.1 g/cm3
|
|
| 沸点 |
664.7±55.0 °C at 760 mmHg
|
|
| 熔点 |
159-160ºC
|
|
| 闪点 |
355.8±31.5 °C
|
|
| 蒸汽压 |
0.0±2.0 mmHg at 25°C
|
|
| 折射率 |
1.676
|
|
| LogP |
3.05
|
|
| tPSA |
81.93
|
|
| 氢键供体(HBD)数目 |
1
|
|
| 氢键受体(HBA)数目 |
5
|
|
| 可旋转键数目(RBC) |
7
|
|
| 重原子数目 |
27
|
|
| 分子复杂度/Complexity |
485
|
|
| 定义原子立体中心数目 |
0
|
|
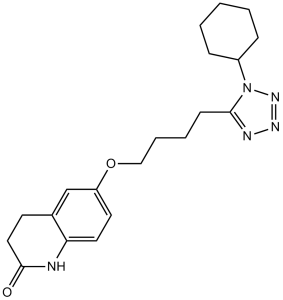
| SMILES |
O=C1NC2=C(C=C(OCCCCC3=NN=NN3C4CCCCC4)C=C2)CC1
|
|
| InChi Key |
RRGUKTPIGVIEKM-UHFFFAOYSA-N
|
|
| InChi Code |
InChI=1S/C20H27N5O2/c26-20-12-9-15-14-17(10-11-18(15)21-20)27-13-5-4-8-19-22-23-24-25(19)16-6-2-1-3-7-16/h10-11,14,16H,1-9,12-13H2,(H,21,26)
|
|
| 化学名 |
6-[4-(1-cyclohexyltetrazol-5-yl)butoxy]-3,4-dihydro-1H-quinolin-2-one
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 2 mg/mL (5.41 mM) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 悬浮液;超声助溶。
例如,若需制备1 mL的工作液,可将100 μL 20.0mg/mL澄清的DMSO储备液加入到900μL 20%SBE-β-CD生理盐水中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2 mg/mL (5.41 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 20.0 mg/mL 澄清 DMSO 储备液添加到 900 μL 玉米油中并混合均匀。 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.7067 mL | 13.5333 mL | 27.0665 mL | |
| 5 mM | 0.5413 mL | 2.7067 mL | 5.4133 mL | |
| 10 mM | 0.2707 mL | 1.3533 mL | 2.7067 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT01915069 | Completed | Drug: Cilostazol | Contraception | University of Southern California | July 2013 | Phase 2 |
| NCT05671497 | Recruiting | Drug: Cilostazol 100 MG | Rheumatoid Arthritis | Ain Shams University | November 1, 2022 | Phase 2 Phase 3 |
| NCT02374957 | Terminated Has Results | Drug: Cilostazol | Peripheral Arterial Disease Claudication (Finding) |
Wake Forest University Health Sciences | February 2015 | Phase 4 |
| NCT05126836 | Completed Has Results | Drug: Cilostazol 100Mg Tab Drug: Placebo |
Heart Failure With Preserved Ejection Fraction |
University of Minnesota | September 1, 2021 | Phase 2 |