| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| Other Sizes |
|

| 靶点 |
Factor Xa (FXa)
|
|---|---|
| 体外研究 (In Vitro) |
甲苯磺酸艾多沙班以浓度依赖性方式延长人血浆 PT、TT 和 APTT(分别为 1、1 和 5 分钟)[1]。甲苯磺酸艾多沙班的 IC50 为 2.90 µM,可抑制凝血酶诱导的血小板聚集[1]。
依度沙班/DU-176b对FXa的抑制作用 DU‐176b对人类FXa的抑制具有浓度依赖性和竞争性,如Lineweaver–Burk图所示(图2)。Ki值为0.561 nm(表1),与DX‐9065a相比,效力显著提高(Ki = 41 nm)[6]。DU‐176b也以相似的效力抑制食蟹猴和兔的FXa,而大鼠FXa的Ki高于人类FXa(表1),与DX̴9065a的特征相似。对于使用S‐2222作为底物与凝血酶原酶复合物中的FVa、Ca2+和磷脂结合的FXa,DU̴176b的抑制是竞争性的(图3A)。Ki值为0.903 nm,与其对游离FXa的抑制作用相当。DU‐176b还以非竞争性/混合型抑制方式抑制了凝血酶原酶从凝血酶原产生凝血酶(图3B),Ki(2.98 nm)比游离FXa高5.3倍。 依度沙班/DU‐176b的特异性 DU‐176b是凝血酶和FIXa的弱抑制剂,Ki值分别为6.00和41.7 μm;超过10 000‐比FXa的Ki高出一倍。对FVIIa/sTF、FXIa、tPA、aPC、胰蛋白酶、纤溶酶和胰凝乳蛋白酶的活性没有影响,表明DU-176b对FXa具有高度特异性。 体外抗凝活性 Edoxaban/DU‐176b以浓度依赖的方式延长了人血浆的PT、APTT和TT,使PT和APTT分别加倍至0.256和0.508 μm(表2)。然而,TT的CT2要高得多(4.95μm),反映了其抗凝血酶活性,如酶抑制试验所示。DU‐176b在人类、食蟹猴和兔血浆中延长PT的效力相似,而在大鼠血浆中需要更高的浓度。 体外对人血小板聚集的影响 依度沙班/DU‐176b在高达100μg/ml的浓度下不会损害ADP、胶原蛋白或U46619(一种血栓素A2受体激动剂)诱导的人类血小板聚集 μm。高浓度DU‐176b抑制凝血酶诱导的血小板聚集(IC50:2.90 μm),反映其抗凝血酶活性较弱。 |
| 体内研究 (In Vivo) |
甲苯磺酸艾多沙班(0.5、2.5 和 12.5 mg/kg;口服;一次)可显着延长凝血酶原时间 (PT) 并减少血栓形成,且呈剂量依赖性[1]。
大鼠和猴子的PD和PK研究[1] 大鼠血浆中存在显著的FXa抑制活性(86%和94%的抑制率) 口服依度沙班/DU‐176b后h(2.5和5 mg kg−1)(图4A),持续时间高达4 h.在食蟹猴中,DU‐176b也引发了抗FXa活性的快速发作,在4时达到峰值 h(93%),持续24小时 给药后h(11%)(图4B)。1小时后血浆浓度和最大浓度(Cmax)的曲线下面积(AUC) mg kg−1 DU‐176b剂量为852 ± 284 ng·h mL-1和175 ± 74 ng 毫升-1(n = 6, mean ± 标准偏差)。与DU-176b相比,DX-9065a在两种物种中的抗FXa效力较低(图4)。食蟹猴1小时后的AUC和Cmax mg kg−1 DX‐9065a剂量为191 ± 104 ng·h 毫升-1和36.8 ± 20.5 ng 毫升-1(n = 6). 口服依度沙班/DU‐176b[1]的抗血栓作用 大鼠和家兔静脉淤滞血栓形成模型输注低渗盐水和大鼠下腔静脉淤滞导致血栓形成,重量为4.38 ± 0.53 mg口服DU‐176b(0.5、2.5和12.5 mg kg−1)显著且剂量依赖性地减少血栓形成(图5A)并延长PT(图5B)。来自DU-176b处理大鼠的血浆样本抑制了外源性FXa活性(图5C)。在兔子中,DU‐176b还具有剂量依赖性的抗血栓作用(图5D)、PT延长和血浆中的抗FXa活性(数据未显示),在3℃时血栓显著减少91% mg kg−1。 铂丝诱导静脉血栓形成模型[1] 在大鼠静脉中放置铂丝诱导血栓形成,重量为2.45 ± 0.38 金属丝表面有mg。依多沙班/DU‐176b以剂量依赖的方式显著减少血栓形成(图6A)。剂量为2.5 mg kg−1,DU‐176b将血栓形成减少到0.73 ± 0.21 同样,血浆中的FXa抑制活性显著且呈剂量依赖性(图6B)。 对出血时间的影响[1] 依度沙班/DU‐176b对3岁时尾出血时间的影响与对照组没有显著差异 mg kg−1(表3)。在较高剂量(10和30 mg kg−1),与对照组相比,出血时间显著延长(1.9倍)。 |
| 酶活实验 |
依度沙班/DU‐176b[1]的抗FXa活性
为了确定DU‐176b对FXa活性的抑制作用,将FXa加入反应缓冲液(20 mm Tris-HCl,pH 7.4,150 mm NaCl、0.1%BSA)。FXa的最终浓度如下:人FXa(0.005 U 毫升-1,0.7 nm)、兔FXa(0.005U mL−1,无摩尔浓度),大鼠FXa(0.025 U 毫升-1,10 nm)和食蟹猴FXa(0.025 U 毫升-1,3 nm).为了测量FXa对S‐2222的酰胺解,在405处的吸光度 使用微孔板分光光度计SPECTRAmax 340(Molecular Devices,Sunnyvale,CA,USA)在30℃下监测nm 10°C 得到反应速度(mO.D./min)。DU‐176b的抑制常数(Ki)值通过Lineweaver–Burk图和随后的次级图计算得出。 依度沙班/DU‐176b[1]对凝血酶原酶的抑制作用 如Rezaie所述,使用S-2222和生理底物凝血酶原检查了DU‐176b对凝血酶原酶活性的抑制作用。简而言之,脂质囊泡是通过混合1.2 mm磷脂酰胆碱和0.4 mm磷脂酰丝氨酸的氯仿溶液,真空干燥,再悬浮在9%蔗糖中。悬浮液经过超声波处理,囊泡通过孔径为50-200的过滤器挤出 nm.凝血酶原酶是通过混合人FXa(S-2222为0.4 nm和0.2 nm)形成的 凝血酶原为pm)、FVa(10 nm)、CaCl2(2.5 mm)和磷脂酰胆碱/磷脂酰丝氨酸囊泡(25μm)在37 5°C 如DU‐176b的抗FXa活性所述,测量了S-2222(250-1000μm)的酰胺解。凝血酶原(7.8-250 nm)的凝血酶生成量测量如下:凝血酶原酶反应持续3 min,并通过添加10 mm EDTA。通过底物S-2238的酰胺解来测量产生的凝血酶的活性,并根据标准曲线确定凝血酶的浓度。Ki值是使用Lineweaver‐Burk图和随后的次级图计算的。 依度沙班/DU‐176b[1]丝氨酸蛋白酶抑制的特异性 研究了DU‐176b对以下丝氨酸蛋白酶(终浓度)的影响:凝血酶(0.03 U 毫升-1,0.5 nm)、FVIIa/sTF(2nm/20 nm)、FIXa(6.25U) mL−1,摩尔浓度不可用),FXIa(0.25 nm),tPA(750 U 毫升-1,20 nm)、aPC(2.5nm)、胰蛋白酶(0.3U 毫升-1,1 nm)、纤溶酶(0.004U) 毫升-1,4 nm)和胰凝乳蛋白酶(0.005 U 毫升-1,2.5 nm).通过以下产色底物对相应蛋白酶的酰胺解来评估酶活性:凝血酶的S‐2238、fVIIa/sTF的Spectrozyme fVIIa、fIXa的Spectrozzyme fIXa、FXIa和aPC的S⁰2366、tPA的S∀2288、纤溶酶的S≮2251、胰蛋白酶的S∆2222和胰凝乳蛋白酶的S?2586。这些酶的Ki值如前所述测定。 体外抗凝活性[1] 研究了依度沙班/DU‐176b的体外抗凝作用。使用微型凝血仪Amelung KC-10A(MC Medical,日本东京)测量人、大鼠、食蟹猴和兔血浆中的凝血时间(CT),抗凝活性表示为CT加倍所需的DU-176b浓度(CT2),通过剂量反应曲线的回归分析估算。凝血酶原时间(PT)是通过将血浆和DU‐176b(对照;4%DMSO/盐水)孵育1小时来测量的 37分钟 °C,然后加入凝血活酶C Plus(终浓度0.25 U mL−1)。通过将血浆、DU‐176b和Platelin LS孵育5小时来测量活化部分凝血活酶时间(APTT) 37分钟 然后加入CaCl2(8.3 mm)。通过将血浆和DU‐176b孵育1小时来测量凝血酶时间(TT) 37分钟 °C,然后加入人凝血酶(4 U mL−1)。 血小板聚集[1] 通过在200℃下离心从健康志愿者的血液样本中制备富血小板血浆(PRP) × g代表10 在室温下保持min。为了制备洗涤过的血小板,然后将PRP在600℃下离心 × g代表10 在Cor缓冲液(138mm NaCl,2.9 氯化钾,10毫米 mm庚烷-氢氧化钠,pH 7.3、5.5 mm葡萄糖,12 mm NaHCO3),含有前列腺素E1(1μm)和EDTA(10mm)。洗涤血小板(2× 108 血小板 mL−1)悬浮在含有纤维蛋白原(1 mg)的Cor缓冲液中 毫升-1)和氯化钙(1毫米)。依度沙班将DU‐176b加入PRP或洗涤血小板悬液中,孵育2或4小时 37分钟 °C.添加胶原蛋白(0.8μg)可诱导血小板聚集(>60%) PRP中的U46619(0.7μm)或ADP(5μm)和凝血酶(0.08 U mL−1)在洗涤的血小板悬浮液中。使用聚集仪PAM‐12C(MC Medical)测量血小板聚集。回归分析用于计算DU‐176b的IC50。 |
| 细胞实验 |
细胞活力测定[1]
细胞类型:人、大鼠、食蟹猴、兔血浆;人血小板 测试浓度: 孵育时间: 1 和 5 分钟 实验结果: 抗凝血酶。 |
| 动物实验 |
Animal/Disease Models: Male Slc: Wistar rat (210-240g); male New Zealand white rabbit (2.5-3.5kg) (both are venous stasis and thrombosis models) [1].
Doses: 0.5, 2.5 and 12.5 mg/kg Route of Administration: Oral; Primary Experimental Results:Inhibition of exogenous FXa activity. Anti-thrombotic. PD and PK studies of Edoxaban/DU‐176b after oral administration to rats and cynomolgus monkeys [1] DU‐176b, DX‐9065a or the 0.5% methylcellulose vehicle were administered orally to fasted animals by gavage, and citrated blood samples were collected at 0.5, 1, 2 and 4 h in rats (n = 4 per dose group), and 0.5, 1, 2, 4, 8 and 24 h in cynomolgus monkeys (n = 6 per dose group) after administration. To measure FXa inhibition activity in plasma, a plasma sample (5 μL) was added to the reaction mixture of human FXa (0.01 U mL−1, 1.4 nm) and S‐2222 (300 μm). Amidolysis of S‐2222 was measured as described. The plasma concentrations of DU‐176b and DX‐9065a were measured by high‐performance liquid chromatography with tandem mass spectrometric detection. Antithrombotic effects of orally administered Edoxaban/DU‐176b [1] Venous stasis thrombosis model in rats DU‐176b (0.5–12.5 mg kg−1) or 0.5% methylcellulose was orally administered to fasted rats (n = 8 per dose group). Venous thrombosis was induced 30 min after DU‐176b administration according to the method by Hladovec while the animals were anesthetized with thiopental sodium (100 mg kg−1, i.p.). Briefly, hypotonic NaCl solution (0.225%) was injected into the femoral vein (5 mL kg−1 min−1 for 2 min), and the inferior vena cava was ligated just below the left renal vein. Ten minutes later, the vena cava was ligated again 1.5 cm below the first ligature. The resulting thrombus was removed 1 h after the second ligation and its wet weight was measured. Blood samples were collected 29 min after DU‐176b dosing to measure PT and plasma FXa inhibition activity. Venous stasis thrombosis model in rabbits [1] DU‐176b/Edoxaban (0.3–3 mg kg−1) or 0.5% methylcellulose was administered orally to fasted rabbits (n = 8 per dose group). The rabbits were anesthetized with urethane (2 g kg−1, i.p.) and venous thrombosis was induced 45 min after DU‐176b administration according to the method by Wessler et al. with some modifications. Recombinant human TF (0.05 μg 2‐mL−1 kg−1 for 30 s) was injected into the auricular vein, and 15 s later blood stasis was made in a 2‐cm segment of the jugular vein by a pair of ligations. The resulting thrombus was removed after 30 min, and its wet weight was measured. Platinum wire‐induced venous thrombosis model in rats [1] Thrombus was induced by the insertion of a platinum wire (2 cm long) into the inferior vena cava of rats (n = 8 per dose group) just caudal to the left renal vein 30 min after oral administration of Edoxaban/DU‐176b (0.1–2.5 mg kg−1) or 0.5% methylcellulose according to the method of Lavelle and Iomhair. The resulting thrombus was fixed 1 h later with 1% glutaraldehyde. The wet weight of the thrombus was measured and blood samples were collected 29 min after DU‐176b dosing to measure plasma FXa inhibition activity. Effect of Edoxaban/DU‐176b on bleeding time [1] Hemorrhage was induced 30 min following oral administration of DU‐176b (3–30 mg kg−1) or 0.5% methylcellulose and bleeding time was measured in a rat tail bleeding model. Briefly, an incision (1 mm deep) was made 4 cm from the tip of the tail. Blood was blotted every 15 s on filter papers, and bleeding time was defined as the time from the incision to the first arrest of bleeding. The maximum observation period was 30 min and longer bleeding time was assigned a value of 30 min. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Following oral administration, peak plasma edoxaban concentrations are observed within 1-2 hours. Absolute bioavailability is 62%. Edoxaban is eliminated primarily as unchanged drug in urine. Renal clearance (11 L/hour) accounts for approximately 50% of the total clearance of edoxaban (22 L/hour). Metabolism and biliary/intestinal excretion account for the remaining clearance. The steady state volume of distribution is 107 L. 22 L/hr /MILK/ There are no data on the presence of edoxaban in human milk ... . Edoxaban was present in rat milk. ... Disposition is biphasic. The steady-state volume of distribution (Vdss) is 107 (19.9) L (mean (SD)). In vitro plasma protein binding is approximately 55%. There is no clinically relevant accumulation of edoxaban (accumulation ratio 1.14) with once daily dosing. Administration of a crushed 60 mg tablet, either mixed into applesauce or suspended in water and given through a nasogastric tube, showed similar exposure compared to administration of an intact tablet. Edoxaban is eliminated primarily as unchanged drug in the urine. Renal clearance (11 L/hour) accounts for approximately 50% of the total clearance of edoxaban (22 L/hour). Metabolism and biliary/intestinal excretion account for the remaining clearance. Following oral administration, peak plasma edoxaban concentrations are observed within 1-2 hours. Absolute bioavailability is 62%. Food does not affect total systemic exposure to edoxaban. Savaysa was administered with or without food in the ENGAGE AF-TIMI 48 and Hokusai VTE trials. Metabolism / Metabolites Edoxaban is not extensively metabolized by CYP3A4 resulting in minimal drug-drug interactions. However, it does interact with drugs that inhibit p-gp (p-glycoprotein), which is used to transport edoxaban across the intestinal wall. Unchanged edoxaban is the predominant form in plasma. There is minimal metabolism via hydrolysis (mediated by carboxylesterase 1), conjugation, and oxidation by CYP3A4. The predominant metabolite M-4, formed by hydrolysis, is human-specific and active and reaches less than 10% of the exposure of the parent compound in healthy subjects. Exposure to the other metabolites is less than 5% of exposure to edoxaban. ... All subjects received a single oral 60 mg edoxaban dose in period 1, and 7 days of 600 mg rifampin (2 x 300 mg capsules once daily) with a single oral edoxaban 60 mg dose administered concomitantly on day 7 in period 2. A 6-day washout period separated the treatments. Plasma concentrations of edoxaban and its metabolites M4 and M6 were measured, and limited assessments of pharmacodynamic markers of coagulation were performed. In total, 34 healthy subjects were enrolled; 32 completed the study. Coadministration of rifampin with edoxaban decreased edoxaban exposure but increased active metabolite exposure. Rifampin increased apparent oral clearance of edoxaban by 33% and decreased its half-life by 50%. Anticoagulant effects based on the prothrombin time (PT) and the activated partial thromboplastin time (aPTT) with and without rifampin at early time points were maintained to a greater-than-expected degree than with edoxaban exposure alone, presumably because of an increased contribution from the active metabolites. Edoxaban was well tolerated in this healthy adult population. Rifampin reduced exposure to edoxaban while increasing exposure to its active metabolites M4 and M6. PT and aPTT at early time points did not change appreciably; however, the data should be interpreted with caution. Edoxaban and its low-abundance, active metabolite M4 are substrates of P-glycoprotein (P-gp; MDR1) and organic anion transporter protein 1B1 (OATP1B1), respectively, and pharmacological inhibitors of P-gp and OATP1B1 can affect edoxaban and M4 pharmacokinetics (PK). In this integrated pharmacogenomic analysis, genotype and concentration-time data from 458 healthy volunteers in 14 completed phase 1 studies were pooled to examine the impact on edoxaban PK parameters of allelic variants of ABCB1 (rs1045642: C3435T) and SLCO1B1 (rs4149056: T521C), which encode for P-gp and OATP1B1. Although some pharmacologic inhibitors of P-gp and OATP1B1 increase edoxaban exposure, neither the ABCB1 C3435T nor the SLCO1B1 T521C polymorphism affected edoxaban PK. A slight elevation in M4 exposure was observed among SLCO1B1 C-allele carriers; however, this elevation is unlikely to be clinically significant as plasma M4 concentrations comprise <10% of total edoxaban levels. The predominant metabolite M-4, formed by hydrolysis, is human-specific and active and reaches less than 10% of the exposure of the parent compound in healthy subjects. Exposure to the other metabolites is less than 5% of exposure to edoxaban. Unchanged edoxaban is the predominant form in plasma. There is minimal metabolism via hydrolysis (mediated by carboxylesterase 1), conjugation, and oxidation by CYP3A4. Biological Half-Life The terminal elimination half-life of edoxaban following oral administration is 10 to 14 hours. The terminal elimination half-life of edoxaban following oral administration is 10 to 14 hours. |
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation Because no information is available on the use of edoxaban during breastfeeding and the drug is orally absorbable, an alternate drug is preferred, especially while nursing a newborn or preterm infant. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Toxicity Summary IDENTIFICATION AND USE: Edoxaban is a white to pale yellowish-white crystalline powder. It is used to reduce the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation. It is also used for the treatment of deep vein thrombosis (DVT) and pulmonary embolism following 5 to 10 days of initial therapy with a parenteral anticoagulant. HUMAN STUDIES: Overdose of the drug increases the risk of bleeding. Edoxaban increases the risk of hemorrhage and can cause serious, potentially fatal, bleeding. Patients should be promptly evaluated if any manifestations of blood loss occur during therapy. The drug should be discontinued if active pathological bleeding occurs. However, minor or "nuisance" bleeding is a common occurrence in patients receiving any anticoagulant and should not readily lead to treatment discontinuance. Edoxaban and its human-specific metabolite, M-4 were not genotoxic in in vitro human lymphocytes micronucleus test. ANIMAL STUDIES: Edoxaban was not carcinogenic when administered daily to mice and rats by oral gavage for up to 104 weeks. Edoxaban showed no effects on fertility and early embryonic development in rats at doses of up to 1000 mg/kg/day. In a rat pre- and post-natal developmental study, edoxaban was administered orally during the period of organogenesis and through lactation day 20 at doses up to 30 mg/kg/day. Vaginal bleeding in pregnant rats and delayed avoidance response (a learning test) in female offspring were seen at 30 mg/kg/day. Embryo-fetal development studies were conducted in pregnant rats and rabbits during the period of organogenesis. In rats, no malformation was seen when edoxaban was administered orally at doses up to 300 mg/kg/day. Increased post-implantation loss occurred at 300 mg/kg/day, but this effect may be secondary to the maternal vaginal hemorrhage seen at this dose in rats. In rabbits, no malformation was seen at doses up to 600 mg/kg/day. Embryo-fetal toxicities occurred at maternally toxic doses, and included absent or small fetal gallbladder at 600 mg/kg/day, and increased post-implantation loss, increased spontaneous abortion, and decreased live fetuses and fetal weight at doses equal to or greater than 200 mg/kg/day. Edoxaban and its human-specific metabolite, M-4, were genotoxic in in vitro chromosomal aberration tests but were not genotoxic in the in vitro bacterial reverse mutation (Ames test), in in vivo rat bone marrow micronucleus test, in in vivo rat liver micronucleus test, and in in vivo unscheduled DNA synthesis tests. Hepatotoxicity Edoxaban is associated with serum aminotransferase elevations greater than 3 times the upper limit of normal in 2% to 5% of treated patients. This rate is similar or lower than rates with warfarin or comparator arms. The elevations are generally transient and not associated with symptoms or jaundice. In premarketing studies, no instances of clinically apparent liver injury were reported, but there was little experience in large numbers of patients treated for extend periods of time. In large health care databases, the rate of liver injury has been somewhat less with edoxaban than rivaroxaban and apixaban, but the numbers of patients treated with edoxaban has been limited and the nature of the liver injury not described. Likelihood score: D (possible race cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Because no information is available on the use of edoxaban during breastfeeding and the drug is orally absorbable, an alternate drug is preferred, especially while nursing a newborn or preterm infant. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding In vitro plasma protein binding is ~55%. Interactions Edoxaban, an oral direct factor Xa inhibitor, is in development for thromboprophylaxis, including prevention of stroke and systemic embolism in patients with atrial fibrillation (AF). P-glycoprotein (P-gp), an efflux transporter, modulates absorption and excretion of xenobiotics. Edoxaban is a P-gp substrate, and several cardiovascular (CV) drugs have the potential to inhibit P-gp and increase drug exposure. /The objective of the study was/ to assess the potential pharmacokinetic interactions of edoxaban and 6 cardiovascular drugs used in the management of AF and known P-gp substrates/inhibitors. Drug-drug interaction studies with edoxaban and CV drugs with known P-gp substrate/inhibitor potential were conducted in healthy subjects. In 4 crossover, 2-period, 2-treatment studies, subjects received edoxaban 60 mg alone and coadministered with quinidine 300 mg (n = 42), verapamil 240 mg (n = 34), atorvastatin 80 mg (n = 32), or dronedarone 400 mg (n = 34). Additionally, edoxaban 60 mg alone and coadministered with amiodarone 400 mg (n = 30) or digoxin 0.25 mg (n = 48) was evaluated in a single-sequence study and 2-cohort study, respectively. Edoxaban exposure measured as area under the curve increased for concomitant administration of edoxaban with quinidine (76.7%), verapamil (52.7%), amiodarone (39.8%), and dronedarone (84.5%), and exposure measured as 24 hr concentrations for quinidine (11.8%), verapamil (29.1%), and dronedarone (157.6%) also increased. Administration of edoxaban with amiodarone decreased the 24-hr concentration for edoxaban by 25.7%. Concomitant administration with digoxin or atorvastatin had minimal effects on edoxaban exposure. Coadministration of the P-gp inhibitors quinidine, verapamil, and dronedarone increased edoxaban exposure. Modest/minimal effects were observed for amiodarone, atorvastatin, and digoxin. The oral direct factor Xa inhibitor edoxaban is a P-glycoprotein (P-gp) substrate metabolized via carboxylesterase-1 and cytochrome P450 (CYP) 3A4/5. The effect of rifampin-induced induction of P-gp and CYP3A4/5 on transport and metabolism of edoxaban through the CYP3A4/5 pathway was investigated in a single-dose edoxaban study. This was a phase 1, open-label, two-treatment, two-period, single-sequence drug interaction study in healthy adults. All subjects received a single oral 60 mg edoxaban dose in period 1, and 7 days of 600 mg rifampin (2 x 300 mg capsules once daily) with a single oral edoxaban 60 mg dose administered concomitantly on day 7 in period 2. A 6-day washout period separated the treatments. Plasma concentrations of edoxaban and its metabolites M4 and M6 were measured, and limited assessments of pharmacodynamic markers of coagulation were performed. In total, 34 healthy subjects were enrolled; 32 completed the study. Coadministration of rifampin with edoxaban decreased edoxaban exposure but increased active metabolite exposure. Rifampin increased apparent oral clearance of edoxaban by 33% and decreased its half-life by 50%. Anticoagulant effects based on the prothrombin time (PT) and the activated partial thromboplastin time (aPTT) with and without rifampin at early time points were maintained to a greater-than-expected degree than with edoxaban exposure alone, presumably because of an increased contribution from the active metabolites. Edoxaban was well tolerated in this healthy adult population. Rifampin reduced exposure to edoxaban while increasing exposure to its active metabolites M4 and M6. PT and aPTT at early time points did not change appreciably; however, the data should be interpreted with caution. Verapamil increased peak plasma concentrations and systemic exposure of edoxaban by approximately 53%; pharmacokinetic parameters of verapamil were altered to only a slight extent. Dosage of edoxaban should be reduced when the drug is administered concomitantly with verapamil in patients with venous thromboembolism. Quinidine increased peak plasma concentrations and systemic exposure of edoxaban by approximately 85 and 77%, respectively, but edoxaban did not affect pharmacokinetics of quinidine. Dosage of edoxaban should be reduced when the drug is administered concomitantly with quinidine in patients with venous thromboembolism. For more Interactions (Complete) data for Edoxaban (19 total), please visit the HSDB record page. |
| 参考文献 | |
| 其他信息 |
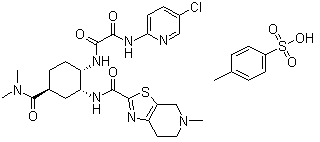
Edoxaban tosylate hydrate is a hydrate that is the monohydrate of the tosylate salt of edoxaban. Used for the treatment of deep vein thrombosis and pulmonary embolism. It has a role as an anticoagulant, an EC 3.4.21.6 (coagulation factor Xa) inhibitor and a platelet aggregation inhibitor. It contains an edoxaban tosylate.
Drug Indication Prevention of stroke and systemic embolism in adult patients with nonvalvular atrial fibrillation (NVAF) with one or more risk factors, such as congestive heart failure, hypertension, age ⥠75 years, diabetes mellitus, prior stroke or transient ischaemic attack (TIA). Treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE), and prevention of recurrent DVT and PE in adults. Edoxaban tosylate is an organosulfonate salt obtained by combining equimolar amounts of edoxaban and 4-toluenesulfonic acid. Used (in the form of its monohydrate) for the treatment of deep vein thrombosis and pulmonary embolism. It has a role as an anticoagulant, an EC 3.4.21.6 (coagulation factor Xa) inhibitor and a platelet aggregation inhibitor. It contains an edoxaban(1+). ChEBI Edoxaban Tosylate is the tosylate salt form of edoxaban, an orally active inhibitor of coagulation factor Xa (activated factor X) with anticoagulant activity. Edoxaban is administered as edoxaban tosylate. This agent has an elimination half-life of 9-11 hours and undergoes renal excretion. NCI Thesaurus (NCIt) EDOXABAN TOSYLATE is a small molecule drug with a maximum clinical trial phase of IV (across all indications) that was first approved in 2015 and has 5 approved and 1 investigational indication. This drug has a black box warning from the FDA. Therapeutic Uses Factor Xa Inhibitors /CLINICAL TRIALS/ ClinicalTrials.gov is a registry and results database of publicly and privately supported clinical studies of human participants conducted around the world. The Web site is maintained by the National Library of Medicine (NLM) and the National Institutes of Health (NIH). Each ClinicalTrials.gov record presents summary information about a study protocol and includes the following: Disease or condition; Intervention (for example, the medical product, behavior, or procedure being studied); Title, description, and design of the study; Requirements for participation (eligibility criteria); Locations where the study is being conducted; Contact information for the study locations; and Links to relevant information on other health Web sites, such as NLM's MedlinePlus for patient health information and PubMed for citations and abstracts for scholarly articles in the field of medicine. Edoxaban is included in the database. Savaysa is indicated to reduce the risk of stroke and systemic embolism (SE) in patients with nonvalvular atrial fibrillation (NVAF). /Included in US product label/ Savaysa is indicated for the treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE) following 5 to 10 days of initial therapy with a parenteral anticoagulant. /Included in US product label/ For more Therapeutic Uses (Complete) data for Edoxaban (7 total), please visit the HSDB record page. Drug Warnings /BOXED WARNING/ REDUCED EFFICACY IN NONVALVULAR ATRIAL FIBRILLATION PATIENTS WITH CRCL > 95 ML/MIN. Savaysa should not be used in patients with CrCL > 95 mL/min. In the ENGAGE AF-TIMI 48 study, nonvalvular atrial fibrillation patients with CrCL > 95 mL/min had an increased rate of ischemic stroke with Savaysa 60 mg once daily compared to patients treated with warfarin. In these patients another anticoagulant should be used. /BOXED WARNING/ PREMATURE DISCONTINUATION OF SAVAYSA INCREASES THE RISK OF ISCHEMIC EVENTS. Premature discontinuation of any oral anticoagulant in the absence of adequate alternative anticoagulation increases the risk of ischemic events. If Savaysa is discontinued for a reason other than pathological bleeding or completion of a course of therapy, consider coverage with another anticoagulant as described in the transition guidance. /BOXED WARNING/ SPINAL/EPIDURAL HEMATOMA. Epidural or spinal hematomas may occur in patients treated with Savaysa who are receiving neuraxial anesthesia or undergoing spinal puncture. These hematomas may result in long-term or permanent paralysis. Consider these risks when scheduling patients for spinal procedures. Factors that can increase the risk of developing epidural or spinal hematomas in these patients include: use of indwelling epidural catheters; concomitant use of other drugs that affect hemostasis, such as nonsteroidal anti-inflammatory drugs (NSAIDs), platelet inhibitors, other anticoagulants; a history of traumatic or repeated epidural or spinal punctures; a history of spinal deformity or spinal surgery; optimal timing between the administration of Savaysa and neuraxial procedures is not known. Monitor patients frequently for signs and symptoms of neurological impairment. If neurological compromise is noted, urgent treatment is necessar. Consider the benefits and risks before neuraxial intervention in patients anticoagulated or to be anticoagulated. Safety and efficacy of edoxaban have not been evaluated in patients with mechanical heart valves or moderate to severe mitral stenosis; use of the drug is not recommended in such patients. For more Drug Warnings (Complete) data for Edoxaban (18 total), please visit the HSDB record page. Pharmacodynamics Administration of edoxaban results in prolongation of clotting time tests such as aPTT (activated partial thromboplastin time), PT (prothrombin time), and INR (international normalized ratio). Edoxaban is a monocarboxylic acid amide that is used (as its tosylate monohydrate) for the treatment of deep vein thrombosis and pulmonary embolism. It has a role as an anticoagulant, an EC 3.4.21.6 (coagulation factor Xa) inhibitor and a platelet aggregation inhibitor. It is a monocarboxylic acid amide, a chloropyridine, a thiazolopyridine and a tertiary amino compound. It is a conjugate base of an edoxaban(1+). Edoxaban is a member of the Novel Oral Anti-Coagulants (NOACs) class of drugs, and is a rapidly acting, oral, selective factor Xa inhibitor. By inhibiting factor Xa, a key protein in the coagulation cascade, edoxaban prevents the stepwise amplification of protein factors needed to form blood clots. It is indicated to reduce the risk of stroke and systemic embolism (SE) in patients with nonvalvular atrial fibrillation (NVAF) and for the treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE) following 5-10 days of initial therapy with a parenteral anticoagulant. Traditionally, warfarin, a vitamin K antagonist, was used for stroke prevention in these individuals but effective use of this drug is limited by it's delayed onset, narrow therapeutic window, need for regular monitoring and INR testing, and numerous drug-drug and drug-food interactions. This has prompted enthusiasm for newer agents such as dabigatran, apixaban, and rivaroxaban for effective clot prevention. In addition to once daily dosing, the benefits over warfarin also include significant reductions in hemorrhagic stroke and GI bleeding, and improved compliance, which is beneficial as many patients will be on lifelong therapy. Edoxaban is a Factor Xa Inhibitor. The mechanism of action of edoxaban is as a Factor Xa Inhibitor. Edoxaban is an oral, small molecule inhibitor of factor Xa which is used as an anticoagulant to decrease the risk of venous thromboses, systemic embolization and stroke in patients with atrial fibrillation, and as treatment of deep vein thrombosis and pulmonary embolism. Edoxaban has been linked to a low rate of serum aminotransferase elevations during therapy and to rare instances of clinically apparent acute liver injury. Edoxaban is an orally active inhibitor of coagulation factor Xa (activated factor X) with anticoagulant activity. Edoxaban is administered as edoxaban tosylate. This agent has an elimination half-life of 9-11 hours and undergoes renal excretion. EDOXABAN is a small molecule drug with a maximum clinical trial phase of IV (across all indications) that was first approved in 2015 and has 6 approved and 15 investigational indications. This drug has a black box warning from the FDA. Background: Factor Xa (FXa), a key serine protease that converts prothrombin to thrombin in the coagulation cascade, is a promising target enzyme for the prophylaxis and treatment of thromboembolic diseases. Edoxaban/DU-176b is a novel antithrombotic agent that directly inhibits FXa activity. Objective: To evaluate the in vitro pharmacological profiles and in vivo effects of DU-176b in animal models of thrombosis and bleeding. Methods: In vitro, FXa inhibition, specificity and anticoagulant activities were examined. Oral absorption was studied in rats and cynomolgus monkeys. In vivo effects were studied in rat and rabbit models of venous thrombosis and tail bleeding. Results: DU-176b/Edoxaban inhibited FXa with Ki values of 0.561 nm for free FXa, 2.98 nm for prothrombinase, and exhibited >10 000-fold selectivity for FXa. In human plasma, DU-176b doubled prothrombin time and activated partial thromboplastin time at concentrations of 0.256 and 0.508 microm, respectively. DU-176b did not impair platelet aggregation by ADP, collagen or U46619. DU-176b was highly absorbed in rats and monkeys, as demonstrated by more potent anti-Xa activity and higher drug concentration in plasma following oral administration than a prototype FXa inhibitor, DX-9065a. In vivo, DU-176b dose-dependently inhibited thrombus formation in rat and rabbit thrombosis models, although bleeding time in rats was not significantly prolonged at an antithrombotic dose. Conclusions: DU-176b/Edoxaban is a more potent and selective FXa inhibitor with high oral bioavailability compared with its prototype, DX-9065a. DU-176b represents a promising new anticoagulant for the prophylaxis and treatment of thromboembolic diseases. [1] In conclusion, Edoxaban/DU‐176b is a potent and highly selective direct FXa inhibitor and represents a remarkable improvement in the potency, selectivity and oral bioavailability compared with DX‐9065a. The present study demonstrates that DU‐176b has potential as an oral antithrombotic agent and a promising novel anticoagulant for the prophylaxis and treatment of thromboembolic diseases.[1] |
| 分子式 |
C₃₁H₃₈CLN₇O₇S₂
|
|---|---|
| 分子量 |
720.26
|
| 精确质量 |
719.196
|
| 元素分析 |
C, 51.70; H, 5.32; Cl, 4.92; N, 13.61; O, 15.55; S, 8.90
|
| CAS号 |
480449-71-6
|
| 相关CAS号 |
Edoxaban;480449-70-5;Edoxaban tosylate monohydrate;1229194-11-9;Edoxaban hydrochloride;480448-29-1
|
| PubChem CID |
25022378
|
| 外观&性状 |
White to off-white solid powder
|
| LogP |
4.404
|
| tPSA |
227.62
|
| 氢键供体(HBD)数目 |
5
|
| 氢键受体(HBA)数目 |
12
|
| 可旋转键数目(RBC) |
6
|
| 重原子数目 |
49
|
| 分子复杂度/Complexity |
1090
|
| 定义原子立体中心数目 |
3
|
| SMILES |
CC1=CC=C(C=C1)S(=O)(=O)O.CN1CCC2=C(C1)SC(=N2)C(=O)N[C@@H]3C[C@H](CC[C@@H]3NC(=O)C(=O)NC4=NC=C(C=C4)Cl)C(=O)N(C)C
|
| InChi Key |
ZLFZITWZOYXXAW-QXXZOGQOSA-N
|
| InChi Code |
InChI=1S/C24H30ClN7O4S.C7H8O3S/c1-31(2)24(36)13-4-6-15(27-20(33)21(34)30-19-7-5-14(25)11-26-19)17(10-13)28-22(35)23-29-16-8-9-32(3)12-18(16)37-23;1-6-2-4-7(5-3-6)11(8,9)10/h5,7,11,13,15,17H,4,6,8-10,12H2,1-3H3,(H,27,33)(H,28,35)(H,26,30,34);2-5H,1H3,(H,8,9,10)/t13-,15-,17+;/m0./s1
|
| 化学名 |
N'-(5-chloropyridin-2-yl)-N-[(1S,2R,4S)-4-(dimethylcarbamoyl)-2-[(5-methyl-6,7-dihydro-4H-[1,3]thiazolo[5,4-c]pyridine-2-carbonyl)amino]cyclohexyl]oxamide;4-methylbenzenesulfonic acid
|
| 别名 |
DU-176b; DU 176; DU176; Edoxaban tosylate; 480449-71-6; Edoxaban tosilate; DU 176-b; edoxaban monotosylate; UNII-32W99UE810; CHEBI:85975; edoxaban p-toluenesulfonate; DU-176b; DU-176; Edoxaban; Savaysa; Lixiana
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ~50 mg/mL (~69.42 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (3.47 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (3.47 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (3.47 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.3884 mL | 6.9419 mL | 13.8839 mL | |
| 5 mM | 0.2777 mL | 1.3884 mL | 2.7768 mL | |
| 10 mM | 0.1388 mL | 0.6942 mL | 1.3884 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Prospective Comparison of Incidence of Heavy Menstrual Bleeding in Women Treated With Direct Oral Anticoagulants
CTID: NCT04477837
Phase: Status: Completed
Date: 2024-08-21