| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| Other Sizes |
| 靶点 |
Type II 5α-reductase (IC50: 4.2 nM)
|
|---|---|
| 体外研究 (In Vitro) |
在 PC-3 细胞中,非那雄胺(10 μM;6-24 小时)刺激蛋白质 Nrf2 和 HO-1 的表达[2]。非那雄胺抑制甲壳疟原虫将 [3H] 睾酮 (T) 转化为 [3H]二氢睾酮 (DHT) 的能力[1]。
据报道,许多天然或合成的化学物质显示出前列腺化学预防作用。合成5α-还原酶(5-AR)抑制剂,如非那雄胺和durasteride,作为可能的前列腺化学预防药物获得了特别的兴趣。事实上,两项大规模流行病学研究表明,非那雄胺或杜拉西特显著降低了男性前列腺癌的发病率。然而,这些研究引发了一个意想不到的担忧;非那雄胺和durasteride增加了侵袭性前列腺肿瘤形成的发生。在目前的研究中,研究人员观察到非那雄胺治疗不会影响雄激素难治性PC-3前列腺癌细胞的生长。非那雄胺也不能诱导PC-3细胞凋亡或影响原癌基因的表达。有趣的是,研究发现非那雄胺处理可诱导PC-3细胞中Nrf2和HO-1蛋白的表达。尤其是雄激素难治性前列腺癌细胞(如DU-145和PC-3细胞)中Nrf2蛋白的基础水平高于雄激素应答性前列腺癌细胞(如LNCaP细胞)。此外,非那雄胺处理导致DU-145和PC-3细胞中Nrf2蛋白的选择性诱导,而LNCaP细胞中则没有。考虑到Nrf2介导的II期细胞保护酶的上调有助于减缓正常细胞的肿瘤促进作用,但另一方面,它赋予癌细胞增殖和生存的选择性优势,以抵抗化学致癌和其他形式的毒性,研究人员提出,非那雄胺介导的Nrf2蛋白的诱导可能是男性高级别前列腺肿瘤形成风险增加的原因,至少部分原因是。[2] |
| 体内研究 (In Vivo) |
在患有 BPH 的犬中,非那雄胺(0.1–0.5 毫克/公斤;每天口服一次,持续 16 周)可降低前列腺大小,而不会对精液质量或血清睾酮水平产生负面影响[3]。
非那雄胺显著降低前列腺直径(平均减少20%)、前列腺体积(平均减少43%)和血清DHT浓度(平均减少58%)。非那雄胺减少精液量,但对精液质量或血清睾酮浓度没有不良影响。在这项研究中,狗的主人没有报告任何不良反应。 结论及临床意义:结果表明,非那雄胺可用于减少前列腺增生犬的前列腺大小,而不会对精液质量或血清睾酮浓度产生不良影响。[3] |
| 酶活实验 |
为了开发5α-DHT相关疾病(如BPH和前列腺癌)的治疗方法,需要一个简单的测试系统来筛选5α-SR抑制剂。由于该方法简单、灵敏度高,也适用于筛选5α-SR抑制剂的简单测试系统。在确认非那雄胺对5α-DHT的酶循环没有影响后,我们对大鼠肝脏和前列腺微粒体5α-SR进行了非那雄酰胺的抑制实验。从结果来看,抑制5α-SR-活性50%(IC50)所需的非那雄肽浓度估计分别为21 nM(肝脏5α-SR.)和20 nM(前列腺5α-SR.)。利用瞬时表达5α-SR1和5α-SR2的COS细胞,研究了非那司琼对大鼠5α-SR15α-SR25的抑制作用。在全细胞测定中,非那雄胺对5α-SR1和5α-SR2的IC50值分别为5.2 nM和5.2 nM,而在使用粗酶制剂的测定中,这两个值分别为13和1.0 nM。21 Häusler等人还评估了非那雄酰胺对前列腺微粒体中的大鼠5α-SR的IC50为11 nM,Igarashi等人评估了13 nM,Mitamura等人评估了237 nM。据报道,非那雌胺对前列腺匀浆中的大白鼠5α-SR的IC50在6.8至147 nM的范围内。造成这种差异的原因可能与pH、睾酮浓度和酶制剂等酶活性评价实验条件的差异有关[4]。
|
| 细胞实验 |
蛋白质印迹分析[2]
细胞类型: PC-3、DU-145 和 LNCaP 细胞 测试浓度: 10 μM 孵育时间:6、12、24小时 实验结果:PC-3细胞中HO-1蛋白的表达以时间依赖性方式增加。在 DU-145 和 PC-3 细胞中诱导 Nrf2 蛋白表达,但在 LNCaP 细胞中不表达。 台盼蓝排斥试验[2] 以每孔1×105的密度将PC-3细胞接种于6孔板中。非那雄胺暴露24 h和48 h后,胰蛋白酶化收集细胞,1000 g离心5 min。收集的细胞用冰冷的磷酸盐缓冲盐水(PBS)溶液(pH 7.4)冲洗3次,与100 μl PBS和等量的0.4%台番蓝试剂混合。用血细胞计计算排除台盼蓝试剂的活细胞数后,将稀释系数加倍计算活细胞总数(×2)。 Western blot分析[2] 为了制备全细胞裂解液,细胞在全细胞裂解缓冲液[10 mmol/L Tris-HCl (pH 7.9), 250 mmol/L NaCl, 30 mmol/L二磷酸钠,50 mmol/L氟化钠,0.5% Triton X-100, 10%甘油,1×proteinase抑制剂混合物]中冰保存30分钟。在14800 g离心30分钟后收集裂解物。用BCA蛋白测定试剂盒测定蛋白质浓度。等份含30 mg蛋白质的上清液在1× SDS样品上样缓冲液中煮沸2分钟,用12% SDS- page溶解。将sds -聚丙烯酰胺凝胶中的蛋白质转移到聚偏二氟乙烯(PVDF)膜上。在PBS-Tween 20 (PBST, 0.1% Tween 20)中,用5%脱脂牛奶在室温下封闭膜2小时,然后用一抗(1:10 000)在PBS中在4℃下过夜。用PBST(含0.1% Tween-20的PBS)冲洗印迹3次,然后用1:50 000稀释的辣根过氧化物酶偶联第二抗体在室温下孵育1小时。印迹在PBST缓冲液中洗涤5分钟3次,使用增强化学发光(ECL)观察转移的蛋白。 双荧光素酶活性测定[2] 将U2OS细胞置于六孔板中,让其在70%左右的合流度下生长。0.1 mg COX-2-、MMP2-和nf - kb启动子驱动萤火虫荧光素酶构建体与0.1 μg Renilla荧光素酶质粒共转染,使用脂质体试剂。转染后,用DMSO或非那雄胺处理细胞48小时。然后收集细胞,用GLOMAX multi检测系统测量双荧光素酶活性。将测量的萤火虫荧光素酶活性与测量的Renilla荧光素酶活性归一化,结果值表示为对对照的倍数诱导。实验值以均数±标准差表示,采用n=6的学生t检验进行统计分析。 |
| 动物实验 |
Animal/Disease Models: Male dogs with spontaneous BPH (2.7-11 years old ; 10.3-49 kg)[3]
Doses: 0.1-0.5 mg/kg Route of Administration: Po one time/day for 16 weeks Experimental Results: diminished prostatic diameter (20%), prostatic volume (43%), and serum DHT concentration (58%) . diminished semen volume but did not adversely effect on semen quality or serum testosterone concentration. No adverse effects on dogs. Objective: To determine the effect of the 5alpha-reductase inhibitor finasteride on prostatic diameter and volume, semen quality, and serum dihydrotestosterone (DHT) and testosterone concentrations in dogs with spontaneous benign prostatic hypertrophy (BPH). Design: Double-blind placebo-controlled trial. Animals: 9 dogs with BPH. Procedure: Five dogs were treated with finasteride for 16 weeks (0.1 to 0.5 mg/kg [0.05 to 0.23 mg/lb] of body weight, PO, q 24 h); the other 4 received a placebo. Prostatic diameter, measured radiographically, prostatic volume, measured ultrasonographically, semen quality, and serum DHT and testosterone concentrations were evaluated before and during treatment. After receiving the placebo for 16 weeks, the 4 control dogs were treated with finasteride for 16 weeks, and evaluations were repeated.[3] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Finasteride is well absorbed following oral administration and displays a slow accumulation phase after multiple dosing.[lablel] In healthy male subjects receiving oral finasteride, the mean oral bioavailability was 65% for 1 mg finasteride and 63% for 5 mg finasteride, and the values ranged from 26 to 170% for 1 mg dose and from 34 to 108% for 5 mg dose, respectively. It is reported that food intake does not affect the oral bioavailability of the drug. The peak plasma concentrations (Cmax) averaged 37 ng/mL (range, 27-49 ng/mL) and was reached 1-2 hours post administration. The AUC(0-24 hr) was 53 ngxhr/mL (range, 20-154 ngxhr/mL). The plasma concentrations and AUC are reported to be higher in elderly male patients aged 70 years or older. In healthy subjects, about 32-46% of total oral dose of finasteride was excreted in the urine in the form of metabolites while about 51-64% of the dose was excreted in the feces. In patients with renal impairment, the extent of urinary excretion of finasteride is expected to be decreased while the fecal excretion is increased. The volume of distribution is 76 L at steady state, ranging from 44 to 96 L. Finasteride has been shown to cross the blood brain barrier but does not appear to distribute preferentially to the CSF. It is not known whether finasteride is excreted in human milk. In healthy young subjects (n=15), the mean plasma clearance of finasteride was 165 mL/min with the range between 70 and 279 mL/min. Metabolism / Metabolites Finasteride undergoes extensive hepatic metabolism predominantly mediated by the cytochrome P450 3A4 (CYP3A4) enzyme to form the t-butyl side chain monohydroxylated and monocarboxylic acid metabolites. Theses metabolites retain less than 20% of the pharmacological activity of the parent compound. Finasteride has known human metabolites that include N-(1-Hydroxy-2-methylpropan-2-yl)-9a,11a-dimethyl-7-oxo-1,2,3,3a,3b,4,5,5a,6,9b,10,11-dodecahydroindeno[5,4-f]quinoline-1-carboxamide. Drug is extensively metabolized, primarily in the liver via CYP3A4. Two metabolites have been identified with дЉ_20% of the activity of finasteride. Route of Elimination: Following an oral dose of 14C-finasteride in man (n = 6), a mean of 39% (range, 32 to 46%) of the dose was excreted in the urine in the form of metabolites; 57% (range, 51 to 64%) was excreted in the feces. Urinary excretion of metabolites was decreased in patients with renal impairment. This decrease was associated with an increase in fecal excretion of metabolites. Half Life: 4.5 hours (range 3.3-13.4 hours) Biological Half-Life In healthy young subjects receiving finasteride, the mean elimination half-life in plasma was 6 hours ranging from 3 to 16 hours. In elderly patients over the age of 70 years, the half-life is prolonged to 8 hours. |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
The mechanism of action of Finasteride is based on its preferential inhibition of Type II 5a-reductase through the formation of a stable complex with the enzyme. Inhibition of Type II 5a-reductase blocks the peripheral conversion of testosterone to DHT, resulting in significant decreases in serum and tissue DHT concentrations, minimal to moderate increase in serum testosterone concentrations, and substantial increases in prostatic testosterone concetrations. As DHT appears to be the principal androgen responsible for stimulation of prostatic growth, a decrease in DHT concentrations will result in a decrease in prostatic volume (approximately 20-30% after 6-24 months of continued therapy). In men with androgenic alopecia, the mechanism of action has not been fully determined, but finasteride has shown to decrease scalp DHT concentration to the levels found in hairy scalp, reduce serum DHT, increase hair regrowth, and slow hair loss. |
| 参考文献 | |
| 其他信息 |
Therapeutic Uses
Enzyme Inhibitors Treatment of benign prostatic hypertrophy Antiandrogen therapy appears to produce a 30 to 40% decrease in the volume of the hyperplastic prostate after 3 to 6 months of therapy. Longer treatment may result in further prostatic regression, although this remains to be seen. Biopsy studies suggest that epithelial regression occurs to a much more significant degree than does stromal regression, but this finding may simply reflect the relatively longer turnover of the stromal cell population. The significant placebo effect of oral medication in patients with benign prostatic hyperplasia makes interpretation of clinical symptomatology and uro-flow data difficult. Analysis of symptom improvement is further complicated by the relatively slow improvement of patients on antiandrogen therapy, in contrast to surgery, in which relief is immediate. In addition to limited stromal involution and inadequate treatment duration, other biologic factors may limit the clinical efficacy of antiandrogen therapy. Most importantly, prostatic involution may not necessarily decrease urethral resistance. In addition, obstruction induced detrusor dysfunction may persist after relief of outflow obstruction in some patients, as it does after surgery. Incomplete antiandrogen action of the compounds, as well as compliance issues, may likewise limit efficacy. Although there are no data to suggest that the 5 alpha-reductase inhibitor finasteride will be more effective than other antiandrogen compounds in the treatment of benign prostatic hyperplasia, preliminary studies suggest that it has less toxicity. If long-term studies validate a modest but significant clinical response rate and preservation of sexual function, then finasteride therapy may well be acceptable to a subgroup of men presenting with the symptoms of benign prostatic hyperplasia. Pharmacodynamics Finasteride is an antiandrogenic compound that works by suppressing the production of serum and intraprostatic dihydrotestosterone (DHT) in men via inhibiting the enzyme responsible for the biosynthesis of DHT. The maximum effect of a rapid reduction in serum DHT concentration is expected to be observed 8 hours following administration of the first dose. In a single man receiving a single oral dose of 5 mg finasteride for up to 4 years, there was a reduction in the serum DHT concentrations by approximately 70% and the median circulating level of testosterone increased by approximately 10-20% within the physiologic range. In a double-blind, placebo-controlled study, finasteride reduced intraprostatic DHT level by 91.4% but finasteride is not expected to decrease the DHT levels to castrate levels since circulating testosterone is also converted to DHT by the type 1 isoenzyme expressed in other tissues. It is expected that DHT levels return to normal within 14 days upon discontinuation of the drug. In a study of male patients with benign prostatic hyperplasia prior to prostatectomy, the treatment with finasteride resulted in an approximate 80% lower DHT content was measured in prostatic tissue removed at surgery compared to placebo. While finasteride reduces the size of the prostate gland by 20%, this may not correlate well with improvement in symptoms. The effects of finasteride are reported to be more pronounced in male patients with enlarged prostates (>25 mL) who are at the greatest risk of disease progression. In phase III clinical studies, oral administration of finasteride in male patients with male pattern hair loss promoted hair growth and prevented further hair loss by 66% and 83% of the subjects, respectively, which lasted during two years' treatment. The incidences of these effects in treatment groups were significantly higher than that of the group receiving a placebo. Following finasteride administration, the levels of DHT in the scalp skin was shown to be reduced by more than 60%, indicating that the DHT found in scalp is derived from both local DHT production and circulating DHT. The effect of finasteride on scalp DHT is likely seen because of its effect on both local follicular DHT levels as well as serum DHT levels.. There is evidence from early clinical observations and controlled studies that finasteride may reduce bleeding of prostatic origin. |
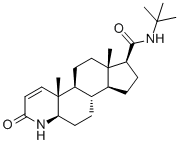
| 分子式 |
C23H36N2O2
|
|
|---|---|---|
| 分子量 |
372.54
|
|
| 精确质量 |
372.277
|
|
| 元素分析 |
C, 74.15; H, 9.74; N, 7.52; O, 8.59
|
|
| CAS号 |
98319-26-7
|
|
| 相关CAS号 |
Finasteride acetate;222989-99-3;Finasteride-d9;1131342-85-2
|
|
| PubChem CID |
57363
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 密度 |
1.1±0.1 g/cm3
|
|
| 沸点 |
576.6±50.0 °C at 760 mmHg
|
|
| 熔点 |
253 °C
|
|
| 闪点 |
177.4±30.3 °C
|
|
| 蒸汽压 |
0.0±1.6 mmHg at 25°C
|
|
| 折射率 |
1.524
|
|
| LogP |
3.24
|
|
| tPSA |
58.2
|
|
| 氢键供体(HBD)数目 |
2
|
|
| 氢键受体(HBA)数目 |
2
|
|
| 可旋转键数目(RBC) |
2
|
|
| 重原子数目 |
27
|
|
| 分子复杂度/Complexity |
678
|
|
| 定义原子立体中心数目 |
7
|
|
| SMILES |
O=C([C@@]1([H])C([H])([H])C([H])([H])[C@@]2([H])[C@]3([H])C([H])([H])C([H])([H])[C@]4([H])[C@@](C([H])=C([H])C(N4[H])=O)(C([H])([H])[H])[C@@]3([H])C([H])([H])C([H])([H])[C@@]21C([H])([H])[H])N([H])C(C([H])([H])[H])(C([H])([H])[H])C([H])([H])[H]
|
|
| InChi Key |
DBEPLOCGEIEOCV-WSBQPABSSA-N
|
|
| InChi Code |
InChI=1S/C23H36N2O2/c1-21(2,3)25-20(27)17-8-7-15-14-6-9-18-23(5,13-11-19(26)24-18)16(14)10-12-22(15,17)4/h11,13-18H,6-10,12H2,1-5H3,(H,24,26)(H,25,27)/t14-,15-,16-,17+,18+,22-,23+/m0/s1
|
|
| 化学名 |
(4aR,4bS,6aS,7S,9aS,9bS,11aR)-N-(tert-butyl)-4a,6a-dimethyl-2-oxo-2,4a,4b,5,6,6a,7,8,9,9a,9b,10,11,11a-tetradecahydro-1H-indeno[5,4-f]quinoline-7-carboxamide
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (6.71 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (6.71 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL 澄清 DMSO 储备液添加到 900 μL 玉米油中并混合均匀。 View More
配方 3 中的溶解度: 2 mg/mL (5.37 mM) in 50% PEG300 50% Saline (这些助溶剂从左到右依次添加,逐一添加), 悬浊液; 超声助溶。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.6843 mL | 13.4214 mL | 26.8428 mL | |
| 5 mM | 0.5369 mL | 2.6843 mL | 5.3686 mL | |
| 10 mM | 0.2684 mL | 1.3421 mL | 2.6843 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。