| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5mg |
|
||
| 10mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| Other Sizes |
|
| 靶点 |
Vasopressin V2 receptor ( IC50 = 14 nM ); Vasopressin V1 receptor ( IC50 = 1.2 μM )
|
|---|---|
| 体外研究 (In Vitro) |
Mozavaptan (OPC-31260) 对 V2 受体的特异性大约高 100 倍,并竞争性抑制 AVP 与大鼠肾脏(V2 受体)和肝脏(V1 受体)质膜的结合。大鼠肝脏的 [3H]-AVP Kd 值为 1.1 nM,而大鼠肾脏的浓度为 1.38 nM。 Mozavaptan 显着降低大鼠肝脏和肾脏中 [3H]-AVP 的 Kd(剂量为 0.3 μM 和 1 μM 时,V1 受体的 Kd 分别为 2.47 nM 和 5.51 nM;剂量为 2.4 nM 和 1 μM 时,Kd 分别为 2.47 nM 和 5.51 nM)。在 0.3 μM 和 1 μM 剂量下,V2 受体的浓度为 4.03 nM [1]。
体外活性:Mozavaptan (OPC-31260) 是一种非肽、口服有效的 AVP 竞争性抑制剂,V2:V1 受体选择性比为 25:1,表明相对 V2 受体选择性。 Mozavaptan (OPC-31260) 以竞争性方式抑制 AVP 与 V1 和 V2 受体的结合。激酶测定:为了确定结合动力学常数,将肝脏或肾脏质膜与浓度逐渐增加的[3H]-AVP(有或没有过量(1μM)未标记的AVP)一起孵育,以获得饱和曲线。为了研究莫扎伐普坦是否竞争性或非竞争性相互作用,在肝膜中浓度为 0.3 μM 和 1 μM 以及肾膜中浓度为 3 nM 和 10 nM 的莫扎伐普坦不存在和存在的情况下检查 [3H]-AVP 的饱和结合。饱和曲线上的数据根据Scatchard方法绘制并通过回归分析进行拟合。 OPC-31260是一种苯扎氮平衍生物,已被研究其拮抗精氨酸加压素(AVP)与大鼠肝(V1)和肾(V2)质膜受体结合的能力,拮抗AVP在酒精麻醉大鼠中的抗利尿作用,以及在清醒的正常大鼠中具有利尿作用。2.OPC-31260引起[3H]-AVP与V1和V2受体结合的竞争性置换,IC50值分别为1.2+/-0.2 x 10(-6)M和1.4+/-0.2 x 10-8M[1]。 |
| 体内研究 (In Vivo) |
口服药物莫扎瓦普坦(OPC-31260;1-30 mg/kg)剂量依赖性地增加水合清醒大鼠的尿流量并降低尿液渗透压[1]。在用酒精镇静并灌水的大鼠中,莫扎伐普坦(OPC-31260;10-100 μg/kg;静脉注射;雄性 Sprague-Dawley 大鼠)疗法以剂量依赖性方式抑制外源性精氨酸加压素 (AVP)。抗利尿药的影响[1]。
Mozavaptan (OPC-31260) 以剂量依赖性方式抑制水负载、酒精麻醉的大鼠中外源施用 AVP 的抗利尿作用。在正常清醒大鼠中口服 1 至 30 mg/kg 剂量后,OPC-31260 会剂量依赖性地增加尿流量并降低尿渗透压。
静脉注射10至100微克kg-1剂量的OPC-31260以剂量依赖的方式抑制了水负荷酒精麻醉大鼠外源性AVP的抗利尿作用。OPC-31260没有发挥抗利尿活性,表明它不是部分V2受体激动剂。4.正常清醒大鼠口服1至30mg kg-1剂量的OPC-31260后,尿流量呈剂量依赖性增加,尿渗透压降低。OPC-31260的利尿作用被描述为利尿作用,其利尿作用方式不同于以前已知的利尿剂,如呋塞米、氢氯噻嗪和螺内酯。5.结果表明,OPC-31260是一种选择性V2受体拮抗剂,具有利尿作用。OPC-31260将成为研究AVP生理作用和治疗以保水为特征的各种疾病的有用工具[1]。 异位抗利尿激素综合征是一种以稀释性低钠血症为特征的医疗紧急情况。在16名患者中评估了加压素V2受体拮抗剂莫扎伐普坦的临床疗效。在短期(7天)药物治疗中,血清钠浓度(平均值±标准差)从122.8±6.7显著增加到133.3±8.3 mEq/l(P=0.002),低钠血症症状得到改善。基于这些结果,mozavaptan(Physuline(®))于2006年在日本被批准为治疗该综合征的孤儿药。在推出后的43个月里,已有100名患者接受了该药物的治疗;发现该药物的总体临床效果与本临床试验相似。临床上,莫扎伐普坦可能允许低钠血症患者通过含铂药物的癌症积极化疗进行治疗。此外,该药物可以使患者摆脱严格的液体摄入限制,从而提高他们的生活质量[2]。 |
| 酶活实验 |
为了确定结合动力学常数,将肝脏或肾脏质膜与浓度逐渐增加的 [3H]-AVP 一起孵育,并添加或不添加过量 (1 μM) 未标记的 AVP,以获得饱和曲线。通过检查浓度为 0.3 μM 和 1 μM 的肝膜中的 [3H]-AVP 以及浓度为 3 nM 和 10 nM 的肾膜中的 [3H]-AVP 的饱和结合来确定莫扎伐普坦以非竞争性或竞争性的方式相互作用。使用Scatchard方法将数据绘制在饱和曲线上,并使用回归分析来拟合数据。
|
| 动物实验 |
Animal/Disease Models: Hydrated conscious rat (300-350 g) [1]
Doses: 1 mg/kg, 3 mg/kg, 10 mg/kg, 30 mg/kg Route of Administration: Oral Experimental Results: Dose-dependent increase in urinary flow and diminished urine osmolarity. Dissolved in 3% ethanol (v/v), 1.67% glucose (w/v) and 0.3% NaCl (w/v); 10, 30, 100μg/kg; i.v. injection; Male Sprague-Dawley rats. This open-label, multicenter study protocol was approved by the Institutional Review Board of each participating medical institution prior to its inception; written informed consent was obtained from all patients. Recruited were inpatients aged 20 to <75 years who had malignant tumors that might cause ectopic ADH syndrome as well as the diagnostic criteria of ectopic ADH syndrome as defined by Bartter and Schwartz such as serum sodium concentration ≤124 mEq/l, persistent urinary sodium excretion, normal renal, adrenal, and thyroid function, and no evidence of edema or dehydration. Following a ≤2-day placebo administration period during which baseline data were collected, patients were given orally mozavaptan (single 30 mg tablet) once daily for 7 days, or where this was difficult, 3 days was allowed. Fluid restriction was used throughout the study period only for patients in whom it had already begun. Treatment of hyponatremia with demeclocycline, lithium chloride, or urea was not permitted. The primary endpoint was serum sodium concentration. Blood samples were collected immediately before dosing on each test day. Clinical symptoms associated with hyponatremia such as anorexia, nausea/vomiting, headache, and CNS symptoms were recorded. Urine volume, urinary osmolality, urinary electrolyte (sodium, potassium, chloride) excretion, serum electrolyte (potassium, chloride) concentration, serum osmolality, and plasma ADH concentration were measured. New medical problems or exacerbations of those already existing were reported as adverse events. In each case, the serum sodium level after the final administration of the study drug was compared with baseline value. The patients are divided into three groups: (i) the serum sodium level is improved to normal range; (ii) the level is still low, but increase is ≥6 mEq/l and (iii) the level is still low, and increase is <6 mEq/l. And mean sodium concentration after the final administration of the study drug was compared with that of baseline value by paired t-test [2]. |
| 药代性质 (ADME/PK) |
At baseline and at the end of study, mean serum sodium concentration was 122.8 ± 6.7 and 133.3 ± 8.3 mEq/l, respectively, a statistically significant difference (P = 0.002; Fig. 1). Serum sodium concentration increased at 24 h after the first administration of mozavaptan and remained elevated ≤24 h after administration for 7 days. Serum osmolality gradually increased starting from 24 h after first administration till the study end. Cumulative urine volume over 24 h increased on the first treatment day, whereas urine osmolality decreased in the first two treatment days. [2]
|
| 毒性/毒理 (Toxicokinetics/TK) |
mouse LDLo oral 1500 mg/kg SENSE ORGANS AND SPECIAL SENSES: PTOSIS: EYE; BEHAVIORAL: SOMNOLENCE (GENERAL DEPRESSED ACTIVITY) Biological and Pharmaceutical Bulletin., 23(182), 2000 [PMID:10706381]
A total of 16 patients were evaluated for the serum sodium level. The serum sodium level was improved to normal range in eight patients, still below normal range but increased by at least 6 mEq/l in four patients and increased by <6 mEq/l in four patients (Table 1). Symptoms associated with ectopic ADH syndrome such as anorexia, nausea/vomiting, headache and CNS symptoms improved or disappeared in seven of eight patients who had at least one of these symptoms at baseline. By symptom, anorexia disappeared in three and improved in two among eight patients who had the symptom at baseline, whereas nausea/vomiting, headache and CNS symptoms disappeared by the completion of treatment in all patients who had at least one of the symptoms at baseline. On the other hand, however, new anorexia and headache developed in one patient each. Although some patients showed slight increases or decreases of plasma ADH concentration after receiving mozavaptan, overall there were no obvious changes. There were 35 adverse events in 11 of the 16 patients; none was serious. The most common adverse event was dry mouth developing in five patients. Fifteen adverse drug reactions occurred in six patients (dry mouth, n = 5; increased blood potassium, n = 2; malaise, increased AST, increased ALT, decreased blood calcium, increased blood lactate dehydrogenase, increased blood urea, decreased appetite and nocturia, n = 1 each). One patient was withdrawn after administration of the study drug for 3 days because of anorexia. After completion of administration of mozavaptan, one cancer-related death occurred 30 days post-treatment (ID 1 in Table 1); the patient had small cell lung cancer, and had myasthenia gravis, diabetes, pneumonia and hypertension. Chemotherapy (carboplatin and etoposide) was given from 146 to 144 days before treatment with mozavaptan, which reduced the tumor size and improved SIADH. However, the chemotherapy was terminated due to marked myelosuppression, and then this led to marked tumor growth. The serum sodium concentration was 132 mEq/l 29 days before the mozavaptan treatment, but gradually decreased to 119 mEq/l 14 days before treatment. At that time, the patient's condition did not permit chemotherapy, and mozavaptan therapy was performed. Although mozavaptan was effective, the condition became worse due to rapid tumor progression. The patient died 30 days after completion of the mozavaptan therapy, and the autopsy demonstrated direct invasion to heart and thoracic vertebra, indicating that the patient had died of cancer. No other serious adverse events were reported.[2] |
| 参考文献 |
|
| 其他信息 |
Mozavaptane hydrochloride is a member of benzamides. It has a role as an aquaretic.
On the basis of these results, mozavaptan (Physuline®) was approved in Japan as an orphan drug for the treatment of ectopic ADH syndrome, in 2006. It is worth noting that until now demeclocycline, lithium chloride or urea was reported effective for the ectopic ADH syndrome, although clinical experiences revealed that the effects of these drugs are limited. In the USA and EU, there are two V2R antagonists available on the market—conivaptan (injection formulation) and tolvaptan (oral tablet). Conivaptan, a dual V1a receptor and V2R antagonist, is marketed in the USA with the indication of ‘treatment of euvolemic and hypervolemic hyponatremia in hospitalized patients’. Tolvaptan, which by structural modification has a higher affinity for the V2R than does its parent drug, mozavaptan, is marketed in the USA with the indication of ‘treatment of clinically significant hypervolemic and euvolemic hyponatremia, including patients with heart failure, cirrhosis and SIADH’ and in the EU with the indication of ‘treatment of adult patients with hyponatremia secondary to syndrome of inappropriate antidiuretic hormone secretion (SIADH)’. Mozavaptan is currently the only approved drug available for treatment of patients with ectopic ADH syndrome in Japan but is neither approved nor under development outside Japan. During the 43 months following its launch, 100 patients have been treated with the drug. On the basis of the post-marketing drug use results survey, overall clinical effects of the drug have been found similar to those of the clinical trial. Mozavaptan provides two important contributions for the treatment of ectopic ADH syndrome. First, short-term treatment with mozavaptan may allow hyponatremic patients who might otherwise be contraindicated to receive aggressive cancer chemotherapy with platinum-containing drugs. Second, mozavaptan may free patients from strict fluid-intake restrictions and thereby improve their quality of life. Thus, mozavaptan provides new treatment options for aggressive chemotherapy as well as for palliative care in patients with ectopic ADH syndrome. [2] |
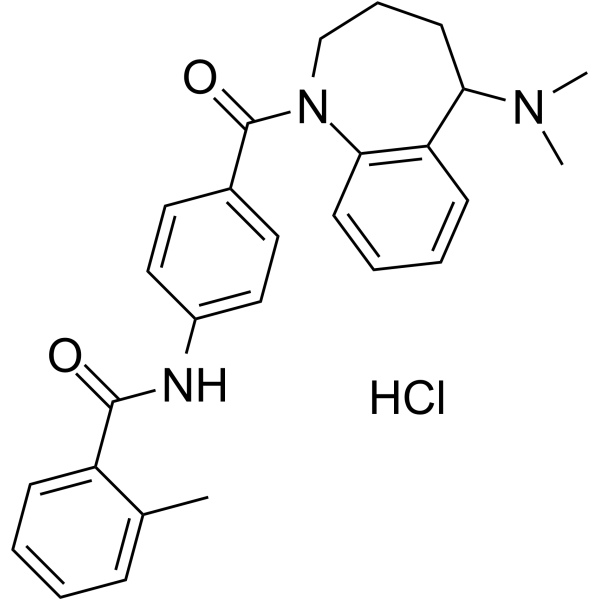
| 分子式 |
C27H30CLN3O2
|
|---|---|
| 分子量 |
464.006
|
| 精确质量 |
463.202
|
| 元素分析 |
C, 69.89; H, 6.52; Cl, 7.64; N, 9.06; O, 6.90
|
| CAS号 |
138470-70-9
|
| 相关CAS号 |
Mozavaptan;137975-06-5
|
| PubChem CID |
636389
|
| 外观&性状 |
White to off-white solid powder
|
| 沸点 |
543ºC at 760mmHg
|
| 闪点 |
282.2ºC
|
| 蒸汽压 |
7.49E-12mmHg at 25°C
|
| LogP |
6.23
|
| tPSA |
52.65
|
| 氢键供体(HBD)数目 |
2
|
| 氢键受体(HBA)数目 |
3
|
| 可旋转键数目(RBC) |
4
|
| 重原子数目 |
33
|
| 分子复杂度/Complexity |
643
|
| 定义原子立体中心数目 |
0
|
| InChi Key |
MOROBKPIULFQDC-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C27H29N3O2.ClH/c1-19-9-4-5-10-22(19)26(31)28-21-16-14-20(15-17-21)27(32)30-18-8-13-24(29(2)3)23-11-6-7-12-25(23)30;/h4-7,9-12,14-17,24H,8,13,18H2,1-3H3,(H,28,31);1H
|
| 化学名 |
N-[4-[5-(dimethylamino)-2,3,4,5-tetrahydro-1-benzazepine-1-carbonyl]phenyl]-2-methylbenzamide;hydrochloride
|
| 别名 |
OPC31260l; OPC31260; Mozavaptan hydrochloride; 138470-70-9; Physuline; mozavaptan HCl; Mozavaptan (hydrochloride); OPC 31260
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ~20.83 mg/mL (~44.89 mM)
H2O : ~10 mg/mL (~21.55 mM) |
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.08 mg/mL (4.48 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 20.8 mg/mL澄清DMSO储备液加入400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.08 mg/mL (4.48 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 20.8 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.08 mg/mL (4.48 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.1551 mL | 10.7756 mL | 21.5513 mL | |
| 5 mM | 0.4310 mL | 2.1551 mL | 4.3103 mL | |
| 10 mM | 0.2155 mL | 1.0776 mL | 2.1551 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。