| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g | |||
| Other Sizes |
| 靶点 |
isoleucyl t-RNA synthetase
Bacterial isoleucyl-tRNA synthetase (IleRS) [1][2] |
|---|---|
| 体外研究 (In Vitro) |
莫匹罗星 (BRL-4910A) 对葡萄球菌和链球菌以及某些革兰氏阴性菌具有高水平的活性。莫匹罗星 (BRL-4910A) 与人血清蛋白高度结合(95% 结合),在人血清存在下活性降低 10 至 20 倍
葡萄球菌属抗菌活性:莫匹罗星(BRL-4910A)对甲氧西林敏感金黄色葡萄球菌(MSSA)、甲氧西林耐药金黄色葡萄球菌(MRSA)及表皮葡萄球菌(包括万古霉素中介菌株)具有强效浓度依赖性抗菌活性。最低抑菌浓度(MIC)范围为:MSSA 0.03-0.12 μg/mL、MRSA 0.06-0.25 μg/mL、表皮葡萄球菌 0.03-0.5 μg/mL [1][5] - 作用机制:特异性抑制细菌异亮氨酸-tRNA合成酶(IleRS),阻断异亮氨酸的活化及其与对应tRNA的氨酰化反应。在MIC浓度下,该作用可在4-6小时内完全抑制靶细菌生长[2] - 无交叉耐药性:在MRSA及多重耐药表皮葡萄球菌菌株中,与β-内酰胺类、万古霉素、大环内酯类等其他类别抗生素无交叉耐药性,证实其作用机制独特[5] - 抗菌谱局限:对革兰氏阴性菌(如大肠杆菌、铜绿假单胞菌)和厌氧菌活性微弱或无活性,MIC值>32 μg/mL [1] |
| 体内研究 (In Vivo) |
莫匹罗星口服和肠胃外给药后吸收良好,但由于广泛降解为无抗菌活性的代谢物莫尼酸 A,因此血清抗生素浓度维持时间较短。
小鼠MRSA浅表皮肤伤口感染:将莫匹罗星(BRL-4910A)制成0.2%(w/w)软膏,每日两次局部涂抹小鼠皮肤伤口,连续5天,较未治疗对照组,伤口MRSA载量降低3-4 log10 CFU/伤口。药物可加速伤口愈合,减轻局部炎症和水肿[3] - 大鼠血管移植物感染预防:血管移植物植入前,用1%(w/w)莫匹罗星(BRL-4910A)溶液浸泡30分钟,可使接受腹主动脉吻合术的大鼠中,表皮葡萄球菌(甲氧西林敏感、MRSA、万古霉素中介菌株)的移植物感染发生率降低70-80%[5] - 全身给药无抗菌疗效:腹腔注射、静脉注射等全身给药方式因全身吸收极少,无显著体内抗菌活性[2] |
| 酶活实验 |
细菌异亮氨酸-tRNA合成酶(IleRS)活性检测:
1. 纯化重组金黄色葡萄球菌IleRS,制备[³H]标记的异亮氨酸和tRNAIle作为反应底物。 2. 将IleRS、[³H]-异亮氨酸、tRNAIle与系列浓度(0.01-1 μg/mL)的莫匹罗星(BRL-4910A)在反应缓冲液(50 mM Tris-HCl pH 7.5,10 mM MgCl₂,2 mM ATP)中于37°C孵育30分钟。 3. 加入5%三氯乙酸终止反应,过滤混合物以保留结合了[³H]-异亮氨酸的tRNA,去除未掺入的核苷酸。 4. 液体闪烁计数法测量保留部分的放射性,定量IleRS介导的氨酰化反应抑制效率[2] |
| 细胞实验 |
细胞系:金黄色葡萄球菌
浓度:0-100 μM/mL 孵育时间:24、48 小时 结果:24 小时后减少 90% 至 99%,MIC 值范围为 0.12- 48 小时时,1.0 μM/mL 和 MBC 值范围为 4.0-32 μM/mL。 最低抑菌浓度(MIC)测定(肉汤稀释法): 1. 在Mueller-Hinton肉汤中制备系列浓度(0.001-64 μg/mL)的莫匹罗星(BRL-4910A)。 2. 向每个浓度梯度中接种MSSA、MRSA或表皮葡萄球菌(含万古霉素中介菌株)的菌悬液(1×10⁵ CFU/mL)。 3. 37°C孵育18-24小时后,肉眼观察细菌生长情况,无可见细菌生长的最低药物浓度即为MIC[1][5] - 抗菌谱琼脂扩散实验: 1. 在Mueller-Hinton琼脂平板上均匀涂布菌苔(MSSA、MRSA、大肠杆菌)。 2. 将浸泡过莫匹罗星(BRL-4910A)(10 μg/片)的无菌滤纸片置于琼脂表面。 3. 37°C孵育24小时后,测量滤纸片周围透明抑菌圈的直径,评估抗菌活性[1] |
| 动物实验 |
MRSA skin infection model in mice (10-12 weeks old)
2% ointment External administration; twice daily; 3-6 days Murine MRSA superficial skin wound infection model: 1. Create 6 mm full-thickness dorsal skin wounds on BALB/c mice (6-8 weeks old), then inoculate each wound with 1×10⁶ CFU of MRSA. 2. Randomly divide mice into an untreated control group and a treatment group (n=8 per group). 3. Formulate Mupirocin (BRL-4910A) as a 0.2% (w/w) ointment and apply it topically to the wounds twice daily for 5 days. 4. On day 5, excise the wound tissues, homogenize them in sterile saline, and plate serial dilutions of the homogenate on agar plates to count bacterial colonies (CFU/wound). Assess wound healing by measuring wound area and performing histopathological analysis of inflammation and tissue regeneration [3] - Rat vascular-graft infection prophylaxis model: 1. Implant polyurethane vascular grafts into male Wistar rats (250-300 g) via abdominal aorta anastomosis. 2. Prior to implantation, soak the grafts in Mupirocin (BRL-4910A) solution (1% w/w) for 30 minutes (treatment group) or sterile saline (control group). 3. Inoculate the graft implantation site with 1×10⁶ CFU of S. epidermidis (methicillin-susceptible, MRSA, or vancomycin-intermediate strain). 4. Four weeks after implantation, harvest the grafts, culture them for bacterial growth, and calculate the infection incidence by comparing the number of infected grafts in the treatment and control groups [5] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Systemic or percutaneous absorption of mupirocin following dermal application is expected to be minimal in adults and children. Occlusive dressings do not significantly enhance drug absorption, but damaged skin may allow enhanced penetration of the drug across the skin barrier. Any mupirocin reaching the systemic circulation is rapidly metabolized to form the inactive monic acid, which is eliminated by renal excretion. Following the application of Centany (mupirocin ointment),2% to a 400 cm2 area on the back of 23 healthy volunteers once daily for 7 days, the mean (range) cumulative urinary excretion of monic acid over 24 hrs following the last administration was 1.25% (0.2% to 3.0%) of the administered dose of mupirocin. No information available. No information available. Metabolism / Metabolites Following intravenous or oral administration, mupirocin undergoes rapid hepatic metabolism to form the principal metabolite monic acid, which has no antibacterial activity. Biological Half-Life In healthy male volunteers, the elimination half-life of mupirocin was about 20 to 40 minutes following intravenous administration. The elimination half-life of monic acid was about 30 to 80 minutes. Absorption: Minimal systemic absorption after topical application—<0.3% of the dose is absorbed through intact skin, and <1% through broken skin. Oral bioavailability is <5% due to degradation in the gastrointestinal tract [2] - Distribution: Primarily remains at the site of topical application with negligible distribution to systemic tissues. Plasma concentrations are undetectable (<0.01 μg/mL) following standard topical use [2] - Metabolism: Metabolized in the skin and liver to inactive metabolites, mainly monic acid derivatives [2] - Excretion: Over 60% of the absorbed dose is excreted in urine as metabolites within 24 hours. The plasma elimination half-life of the absorbed drug is 2-4 hours [2] |
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation Because less than 1% is absorbed after topical application, mupirocin is considered a low risk to the nursing infant.[1] Ensure that the infant's skin does not come into direct contact with the areas of skin that have been treated. Only water-miscible cream or gel products should be applied to the breast because ointments may expose the infant to high levels of mineral paraffins via licking.[2] Mupirocin applied topically to the nipples appears to be relatively ineffective as a treatment for sore, cracked nipples. ◉ Effects in Breastfed Infants A mother who was exclusively nursing her 52-day-old infant developed a soft-tissue infection. She was treated with intravenous teicoplanin 400 mg every 12 hours for 3 doses, then 400 mg daily for 5 days total, intravenous ceftriaxone 1 gram daily, topical mupirocin cream twice daily. A careful follow-up indicated that her infant had no adverse effects.[3] ◉ Effects on Lactation and Breastmilk A small, randomized, unblinded trial of mothers with sore, cracked nipples was performed. Mupirocin 2% applied to the nipples after each feeding was much less effective (16% vs 79%) than an oral antibiotic (cloxacillin or erythromycin for 10 days) in resolving the problem. Additionally, more patients' condition worsened (28% vs 5%) with mupirocin than with an oral antibiotic.[4] In a randomized, double-bind trial, lanolin was compared to an all-purpose nipple ointment containing mupirocin 1%, betamethasone 0.05%, and miconazole 2% for painful nipples while nursing in the first 2 weeks postpartum. The two treatments were equally effective in reducing nipple pain, nipple healing time, breastfeeding duration, breastfeeding exclusivity rate, mastitis and nipple symptoms, side effects or maternal satisfaction with treatment.[5] Protein Binding The protein binding of mupirocin is reported to be over 95%. Local toxicity: Mild and transient skin irritation (erythema, pruritus) was observed in 5-8% of treated mice, which resolved spontaneously within 24 hours without dose interruption [3] - Dermal toxicity in pigs: Topical application of 1% (w/w) Mupirocin (BRL-4910A) for 14 days caused no significant epidermal thickening, inflammation, cytotoxicity, or allergic contact dermatitis in pig skin [4] - Systemic toxicity: No significant systemic toxicity (hepatic/renal dysfunction, hematological abnormalities) was observed in rats and pigs after topical administration at 10× the therapeutic dose. Serum transaminase, creatinine, and white blood cell counts remained within normal ranges [2][4] - Mutagenicity and teratogenicity: No evidence of mutagenicity was found in bacterial reverse mutation assays, and no teratogenic effects were observed in pregnant rats [2] |
| 参考文献 |
|
| 其他信息 |
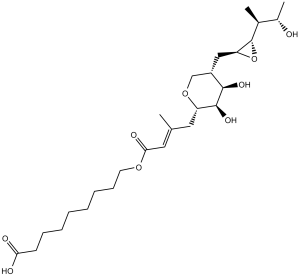
Mupirocin is an alpha,beta-unsaturated ester resulting from the formal condensation of the alcoholic hydroxy group of 9-hydroxynonanoic acid with the carboxy group of (2E)-4-[(2S)-tetrahydro-2H-pyran-2-yl]-3-methylbut-2-enoic acid in which the tetrahydropyranyl ring is substituted at positions 3 and 4 by hydroxy groups and at position 5 by a {(2S,3S)-3-[(2S,3S)-3-hydroxybutan-2-yl]oxiran-2-yl}methyl group. Originally isolated from the Gram-negative bacterium Pseudomonas fluorescens, it is used as a topical antibiotic for the treatment of Gram-positive bacterial infections. It has a role as a bacterial metabolite, an antibacterial drug and a protein synthesis inhibitor. It is a monocarboxylic acid, a member of oxanes, an epoxide, a secondary alcohol, a triol and an alpha,beta-unsaturated carboxylic ester. It is a conjugate acid of a mupirocin(1-).
Mupirocin, formerly termed pseudomonic acid A, is a novel antibacterial agent with a unique chemical structure and mode of action apart from other antibiotic agents. Produced by fermentation using the organism Pseudomonas fluorescens, mupirocin is a naturally-occurring antibiotic that displays a broad-specturm activity against many gram-positive bacteria and certain gram-negative bacteria in vitro. It primarily works by inhibiting bacterial protein synthesis. Due to its unique mode of action of inhibiting the activity of bacterial isoleucyl-tRNA synthetase, mupirocin does not demonstrate cross-resistance with other classes of antimicrobial agents, giving it a therapeutic advantage. It is available in topical formulations only due to extensive systemic metabolism and is used in the treatment of impetigo caused by Staphylococcus aureus and Streptococcus pyogenes and traumatic skin lesions due to secondary skin infections caused by S. aureus and S. pyogenes. There is also some clinical evidence that suggests the potential role of mupirocin in eradicating nasal carriage of Staphylococci when administered intranasally. Mupirocin is commonly marketed under the brand name Bactroban. Mupirocin is a RNA Synthetase Inhibitor Antibacterial. The mechanism of action of mupirocin is as a RNA Synthetase Inhibitor. Mupirocin has been reported in Pseudomonas fluorescens with data available. Mupirocin is a natural crotonic acid derivative extracted from Pseudomonas fluorescens. Mupirocin inhibits bacterial protein synthesis by specific reversible binding to bacterial isoleucyl tRNA synthase. With excellent activity against gram-positive staphylococci and streptococci, it is primarily used for treatment of primary and secondary skin disorders, nasal infections, and wound healing. (NCI04) A topically used antibiotic from a strain of Pseudomonas fluorescens. It has shown excellent activity against gram-positive staphylococci and streptococci. The antibiotic is used primarily for the treatment of primary and secondary skin disorders, nasal infections, and wound healing. Drug Indication Indicated for the treatment of impetigo and secondary skin infections, leading to traumatic skin lesions, due to _Staphylococcus aureus_ and _Streptococcus pyogenes_. Mechanism of Action Mupirocin specifically and reversibly binds to bacterial isoleucyl transfer-RNA (tRNA) synthetase, which is an enzyme that promotes the conversion of isoleucine and tRNA to isoleucyl-tRNA. Inhibition of this enzyme subsequently leads to the inhibition of the bacterial protein and RNA synthesis. Mupirocin is bacteriostatic at lower concentrations but it exerts bactericidal effects with prolonged exposure, killing 90-99% of susceptible bacteria over a 24 hour period. Pharmacodynamics Mupirocin is reported to be active against susceptible aerobic gram-positive cocci, such as _Staphylococcus aureus_, _Staphylococcus epidermidis_, and other beta-hemolytic streptococci_Streptococcus pyogenes_. It mediates its antibacterial activity by inhibiting the bacterial protein synthesis and formation of bacterial proteins essential for survival. The minimum bactericidal concentration (MBC) against relevant pathogens is generally eight-fold to thirty-fold higher than the minimum inhibitory concentration (MIC). In one clinical study investigating the therapeutic effectiveness of topical mupirocin in impetigo, the therapeutic response rate was about 94 to 98% after one week following the end of therapy. In clinical studies of patients with primary and secondary skin infections, both elimination of the bacterial pathogen and clinical cure or improvement hav been demonstrated in over 90% of patients receiving topical mupirocin. Mupirocin resistance as high as 81% has been reported previously. Resistance to mupirocin, which occurs more frequently in methicillin-resistant than methicillin-susceptible staphylococci, may occur with the production of a modified isoleucyl-tRNA synthetase, or the acquisition of, by genetic transfer, a plasmid mediating a new isoleucyl-tRNA synthetase. Mupirocin (BRL-4910A) is a natural antibiotic produced by the bacterium Pseudomonas fluorescens, specifically developed for topical clinical use [1][2] - Mechanism of action: Binds specifically to bacterial isoleucyl-tRNA synthetase (IleRS) with high affinity, preventing the activation of isoleucine and its subsequent charging onto tRNAIle. This blocks bacterial protein synthesis, leading to growth inhibition and eventual bacterial death [1][2] - Clinical indications: Approved for the treatment of superficial skin infections (e.g., impetigo, folliculitis) caused by MSSA and MRSA. It is also used for the prophylaxis of vascular-graft infections and nasal decolonization of S. aureus (including MRSA) [5] - Selectivity advantage: Exhibits 1000-fold higher affinity for bacterial IleRS compared to human IleRS, minimizing off-target effects on mammalian cells [2] - Resistance profile: Intrinsic resistance is rare; acquired resistance is associated with mutations in the bacterial ileS gene (which encodes IleRS) and occurs at a low rate in clinical settings [5] |
| 分子式 |
C26H44O9
|
|
|---|---|---|
| 分子量 |
500.62
|
|
| 精确质量 |
500.298
|
|
| 元素分析 |
C, 62.38; H, 8.86; O, 28.76
|
|
| CAS号 |
12650-69-0
|
|
| 相关CAS号 |
73346-79-9;115074-43-6;104486-81-9
|
|
| PubChem CID |
446596
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 密度 |
1.2±0.1 g/cm3
|
|
| 沸点 |
672.3±55.0 °C at 760 mmHg
|
|
| 熔点 |
77-780C
|
|
| 闪点 |
216.5±25.0 °C
|
|
| 蒸汽压 |
0.0±4.7 mmHg at 25°C
|
|
| 折射率 |
1.524
|
|
| LogP |
3.44
|
|
| tPSA |
146.05
|
|
| 氢键供体(HBD)数目 |
4
|
|
| 氢键受体(HBA)数目 |
9
|
|
| 可旋转键数目(RBC) |
17
|
|
| 重原子数目 |
35
|
|
| 分子复杂度/Complexity |
694
|
|
| 定义原子立体中心数目 |
8
|
|
| SMILES |
O1[C@@]([H])([C@@]([H])(C([H])([H])[H])[C@]([H])(C([H])([H])[H])O[H])[C@]1([H])C([H])([H])[C@@]1([H])C([H])([H])O[C@@]([H])(C([H])([H])/C(=C(\[H])/C(=O)OC([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C(=O)O[H])/C([H])([H])[H])[C@@]([H])([C@]1([H])O[H])O[H]
|
|
| InChi Key |
MINDHVHHQZYEEK-HBBNESRFSA-N
|
|
| InChi Code |
InChI=1S/C26H44O9/c1-16(13-23(30)33-11-9-7-5-4-6-8-10-22(28)29)12-20-25(32)24(31)19(15-34-20)14-21-26(35-21)17(2)18(3)27/h13,17-21,24-27,31-32H,4-12,14-15H2,1-3H3,(H,28,29)/b16-13+/t17-,18-,19-,20-,21-,24+,25-,26-/m0/s1
|
|
| 化学名 |
9-[(E)-4-[(2S,3R,4R,5S)-3,4-dihydroxy-5-[[(2S,3S)-3-[(2S,3S)-3-hydroxybutan-2-yl]oxiran-2-yl]methyl]oxan-2-yl]-3-methylbut-2-enoyl]oxynonanoic acid
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (4.99 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (4.99 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (4.99 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.9975 mL | 9.9876 mL | 19.9752 mL | |
| 5 mM | 0.3995 mL | 1.9975 mL | 3.9950 mL | |
| 10 mM | 0.1998 mL | 0.9988 mL | 1.9975 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Pharmacology of Mupirocin in Nasal Application in Healthy Volunteers: Monocentric Study
CTID: NCT06368856
Phase: Phase 1 Status: Recruiting
Date: 2024-04-16
|