| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| 5g |
|
||
| 10g | |||
| Other Sizes |

| 靶点 |
Inosine monophosphate dehydrogenase (IMPDH); de novo purine synthesis
|
|---|---|
| 体外研究 (In Vitro) |
肌苷单磷酸脱氢酶是 T 淋巴细胞和 B 淋巴细胞用于从头产生鸟苷核苷酸的关键酶 [1]。
Mycophenolate Mofetil/霉酚酸是霉酚酸酯的活性代谢产物,是肌苷单磷酸脱氢酶(IMPDH)的非竞争性可逆抑制剂。抑制IMPDH会阻断鸟苷核苷酸的从头合成,鸟苷核苷酸是DNA和RNA合成所必需的底物。与其他可以使用补救途径的细胞类型不同,B和T淋巴细胞依赖于从头途径产生鸟苷。 体外研究的数据表明,霉酚酸和/或霉酚酸酯/Mycophenolate Mofetil可抑制多种丝裂原和抗原诱导的混合淋巴细胞反应和人类外周血淋巴细胞增殖。霉酚酸降低了丝裂原刺激的人外周血单核细胞或T淋巴细胞系中三磷酸鸟苷(GTP)和脱氧鸟苷三磷酸(dGTP)的细胞内池,但对人中性粒细胞中的GTP浓度没有影响[2]。 目的:免疫抑制剂霉酚酸酯(MMF)诱导的核苷酸耗竭已被证明具有神经保护作用。目前尚不清楚核苷酸耗竭是直接抵消神经元死亡,还是抑制小胶质细胞或星形胶质细胞的激活,从而产生间接的神经保护作用。 方法:通过免疫细胞化学、定量形态计量学和elisa分析MMF对分离的小胶质细胞、星形胶质细胞/小胶质细胞共培养物和分离的海马神经元的影响。 结果:我们发现:(i)MMF抑制脂多糖诱导的小胶质细胞分泌白细胞介素-1β、肿瘤坏死因子-α和一氧化氮;(ii)MMF抑制脂多糖诱导的星形胶质细胞产生肿瘤坏死因子-α,但不抑制一氧化氮;(iii)MMF强烈抑制小胶质细胞和星形胶质细胞的增殖;(iv)MMF不能保护分离的海马神经元免受兴奋性毒性损伤;(v)鸟苷处理后,MMF对神经胶质细胞的作用被逆转。 结论:MMF诱导的核苷酸耗竭抑制了小胶质细胞和星形胶质细胞的活化。MMF诱导的补救途径酶肌苷单磷酸脱氢酶的抑制抑制了小胶质细胞和星形胶质细胞的增殖。先前观察到的MMF治疗后的神经保护作用似乎是间接介导的,使该化合物成为治疗急性中枢神经系统病变的一种有趣的免疫抑制剂[4]。 |
| 体内研究 (In Vivo) |
在 ACI-to-Lewis 大鼠异位心脏移植模型中,20 mg/kg 和 40 mg/kg 剂量的吗替麦考酚酯治疗可延长移植物存活时间,中位存活时间 (MST) 分别为 14.5 天和 18.5 天, 分别。在博莱霉素 (BLM) 诱导的硬皮病小鼠模型中,吗替麦考酚酯可减少炎症细胞浸润、组织羟脯氨酸含量和真皮厚度。
霉酚酸酯/Mycophenolate Mofetil已被证明在几种移植动物模型(包括心脏、肝脏、胰岛和肾脏)中具有疗效。霉酚酸酯能有效预防或逆转啮齿动物心脏和犬肾同种异体移植的排斥反应。然而,该药物在一致性方面效果甚微,在不一致的心脏异种移植物移植中无效。 在大鼠肾移植模型中,Mycophenolate Mofetil/霉酚酸酯有效地减轻了与慢性排斥相关的功能、形态和免疫组织学变化(蛋白尿、肾小球硬化、动脉闭塞、巨噬细胞和淋巴细胞浸润以及粘附分子和细胞因子表达的显著减少)。该药物还被证明可以抑制大鼠和人类的抗体产生。在啮齿动物研究中,霉酚酸酯与心脏同种异体移植后移植心房组织的供体特异性耐受诱导以及胰岛同种异体移植术后移植甲状腺组织或注射脾细胞的供体特异性耐受诱导有关[2]。 霉酚酸酯是一种活性免疫抑制剂霉酚酸的酯类前药。它是一种非竞争性、选择性和可逆的肌苷单磷酸脱氢酶抑制剂,肌苷单磷酸脱氢酶是T和B淋巴细胞中鸟苷核苷酸从头合成的重要酶。霉酚酸酯和/或霉酚酸抑制淋巴细胞的增殖和各种丝裂原和抗原诱导的抗体的产生。霉酚酸酯在几种动物移植模型中也有活性,并在动物身上产生了影响,表明它可能抑制慢性排斥反应过程。在3项大型、随机、双盲、多中心试验中,将霉酚酸酯与硫唑嘌呤或安慰剂进行了比较,作为环孢菌素和皮质类固醇联合免疫抑制治疗的一部分。与安慰剂或硫唑嘌呤(1至2 mg/kg/天或100至150 mg/天)相比,霉酚酸酯2或3 g/天与移植后前6个月发生急性排斥反应或治疗失败的患者比例显著降低有关。霉酚酸酯也往往与需要全疗程抗排斥治疗的患者比例较低有关。然而,所有治疗组死亡或移植物丢失的患者比例相似。目前尚无关于霉酚酸酯对长期患者或移植物存活率影响的数据,而长期患者或移植植物存活率是评估霉酚酸酯在肾移植管理中地位的重要临床结果。还需要进行临床试验,以评估霉酚酸酯在特定患者群体(如重复肾移植患者或高度敏感患者)中的疗效,确定其在替代免疫抑制方案中的有效性,并研究其在其他实体器官移植中的应用。总之,霉酚酸酯似乎是一种预防肾移植受者移植物排斥反应的有吸引力的新药,其疗效优于硫唑嘌呤。尽管需要长期临床结果数据,但霉酚酸酯是移植免疫抑制的一个潜在重要进展[2]。 背景:T淋巴细胞诱导成纤维细胞转化为肌成纤维细胞,这是纤维形成的主要介质。肌苷5'-单磷酸脱氢酶抑制剂霉酚酸酯(MMF)和抗CD25单克隆抗体达利珠单抗(DCZ)已被报道可抑制T淋巴细胞的增殖。 目的:评价MMF和DCZ对博莱霉素(BLM)诱导的硬皮病早期的预防作用。 方法:本研究涉及五组Balb/c小鼠(每组n=10)。其中四组小鼠皮下注射BLM[100μg/天,溶于100μL磷酸盐缓冲盐水(PBS)]4周;其余(对照组)仅接受100μL PBS。三个BLM治疗组也接受了腹腔注射MMF50或150mg/kg/天,或SC DCZ 100μg/周。在第四周结束时,杀死所有小鼠,并采集血液和组织样本进行进一步分析。 结果:在BLM治疗组中,炎症细胞浸润、α-平滑肌肌动蛋白阳性(α-SMA+)成纤维细胞计数、组织羟脯氨酸含量和皮肤厚度均有所增加。皮肤纤维化在组织病理学上表现突出。在BLM治疗的小鼠中,也给予MMF或DCZ,炎症细胞浸润、组织羟脯氨酸含量和皮肤厚度降低。在MMF组中,α-SMA+成纤维细胞计数也有所下降。 结论:在BLM诱导的皮肤纤维化模型中,MMF和DCZ治疗可预防皮肤纤维化的发展。需要进一步的研究来评估靶向T淋巴细胞是否能有效解决人类硬皮病中预先存在的纤维化[5]。 |
| 细胞实验 |
小胶质细胞和星形胶质细胞凋亡和增殖分析[4]
用Mycophenolate Mofetil/MMF处理或在培养基中孵育的小胶质细胞或星形胶质细胞用于确定Mycophenolate Mofetil/MMF可能的毒性浓度范围。通过活化的半胱氨酸天冬氨酸蛋白酶-3的免疫细胞化学显示凋亡细胞。在星形胶质细胞/小胶质细胞共培养中对小胶质细胞进行增殖研究,因为只有在星形胶质胶质细胞存在的情况下才能获得显著的小胶质细胞增殖。单独用LPS或巨噬细胞集落刺激因子刺激分离的小胶质细胞没有诱导显著的增殖活性(数据未显示)。分析小胶质细胞增殖的溴脱氧尿苷(BrdU;0.01 mM)加入培养基中16 h固定前。 胎牛血清(1-10%)或促肾上腺皮质激素释放因子(CRF,10 µM)用于48 h用于刺激分离的星形胶质细胞培养物中的增殖,并加入BrdU(0.01 mM)16 h固定前。增殖指数计算为增殖细胞占细胞总数的百分比。 |
| 动物实验 |
Animals and experimental protocols [5]
Fifty specific‐pathogen‐free female Balb/c mice, 6 weeks old and weighing 20–25 g, were used for the experimental procedures. Defined areas of the lower back skins of the mice were shaved for subcutaneous injections. Mice in the control group received 100 μL/day phosphate‐buffered saline (PBS) subcutaneously (SC) to the shaved back skin. To induce dermal fibrosis, the remaining four groups received BLM 100 μg dissolved in 100 μL PBS and sterilized by filtration (0.2 μm filter) to the shaved skin on the back. Two groups of these BLM‐treated mice were also injected either intraperitoneally with MMF 50 or 150 mg/kg/day dissolved in 100 μL and 300 μL saline containing 0.4% Tween 80 and 0.9% benzyl alcohol, respectively, and a third BLM‐treated group was given DCZ 100 μg (100 μL) SC once weekly. Dissolved in 0.5% methylcellulose water; 40 mg/kg; i.v. administration Lewis rats with abdominal vascularized heterotopic cardiac transplantation Clinical Efficacy [2] Initial noncomparative trials helped to determine the efficacy of mycophenolate mofetil and provided the appropriate dosage regimens for use in larger clinical trials. Three randomised, double-blind, multicentre trials have been conducted comparing mycophenolate mofetil with either placebo or azathioprine as part of combination therapy (with cyclosporin and corticosteroids) for the prevention of renal transplant rejection. Acute rejection or treatment failure (premature withdrawal from the study for any reason) during the first 6 months after transplantation occurred in significantly fewer patients receiving mycophenolate mofetil 2 or 3 g/day (range 30.3 to 38.8%) than either placebo (56.0%), or azathioprine 1 to 2 mg/kg/day (47.6%) or 100 to 150 mg/day (50%). The proportion of patients who required full courses of antirejection therapy (corticosteroids and/or anti-lymphocyte therapy) during the first 6 months post-transplant also tended to be lower in patients who received mycophenolate mofetil (range 21.1 to 31%) than either placebo (51.8%) or azathioprine (44.5 and 46%) recipients although the differences were not statistically significant. There were no differences between any of the treatment groups in terms of graft loss or patient survival at 6 or 12 months. There are currently no data on the effect of mycophenolate mofetil on long term patient or renal graft survival. Subgroup analysis of one multicentre study revealed that African-Americans receiving mycophenolate mofetil 3 g/day tended to have a lower rate of biopsy-proven acute rejection and/or treatment failure than those receiving 2 g/day. The use of mycophenolate mofetil in children is limited to a single report involving 14 patients. Data regarding the use of mycophenolate mofetil in the treatment of acute rejection are limited but initial results are promising. In patients with biopsy-proven rejection, mycophenolate mofetil 3 g/day was associated with a significantly lower frequency of subsequent biopsy-proven rejection or treatment failure than high dose intravenous corticosteroids (29 vs 51%). Dosage and Administration [2] The initial recommended dosage of mycophenolate mofetil for the prevention of renal transplant rejection is lg twice daily to be initiated within 72 hours of transplantation as part of a combination regimen with cyclosporin and corticosteroids. Although dosages of up to 3 g/day have been used, they were less well tolerated than 2 g/day and there was no difference in clinical efficacy between these dosages. In patients with glomerular filtration rate <25 ml/min (1.5 L/h)/ 1.73m dosages should not exceed 2 g/day. Dosage adjustments in patients with delayed graft function are not required. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Mycophenolate mofetil is rapidly absorbed in the small intestine. The maximum concentration of its active metabolite, MPA, is attained 60 to 90 minutes following an oral dose. The average bioavailability of orally administered mycophenolate mofetil in a pharmacokinetic study of 12 healthy patients was 94%. In healthy volunteers, the Cmax of mycophenolate mofetil was 24.5 (±9.5)μg/mL. In renal transplant patients 5 days post-transplant, Cmax was 12.0 (±3.82) μg/mL, increasing to 24.1 (±12.1)μg/mL 3 months after transplantation. AUC values were 63.9 (±16.2) μg•h/mL in healthy volunteers after one dose, and 40.8 (±11.4) μg•h/mL, and 65.3 (±35.4)μg•h/mL 5 days and 3 months after a renal transplant, respectively. The absorption of mycophenolate mofetil is not affected by food. A small amount of drug is excreted as MPA in the urine (less than 1%). When mycophenolate mofetil was given orally in a pharmacokinetic study, it was found to be 93% excreted in urine and 6% excreted in feces. Approximately 87% of the entire administered dose is found to be excreted in the urine as MPAG, an inactive metabolite. The volume of distribution of mycophenolate mofetil is 3.6 (±1.5) to 4.0 (±1.2) L/kg. Plasma clearance of mycophenolate mofetil is 193 mL/min after an oral dose and 177 (±31) mL/min after an intravenous dose. /Absorption/ is rapid and extensive after oral administration. In 12 healthy volunteers, the mean absolute bioavailability of oral mycophenolate mofetil relative to intravenous mycophenolate mofetil (based on MPA AUC) was 94%. The area under the plasma-concentration time curve (AUC) for MPA appears to increase in a dose-proportional fashion in renal transplant patients receiving multiple doses of mycophenolate mofetil up to a daily dose of 3 g. Protein binding: To plasma albumin: High (97% for mycophenolic acid (MPA) at concentration ranges normally seen in stable renal transplant patients). At higher mycophenolic acid glucuronide (MPAG) concentrations (e.g., in patients with renal impairment or delayed graft function), binding of MPA may be decreased as a result of competition between MPA and MPAG for binding sites. The mean (+/-SD) apparent volume of distribution of MPA in 12 healthy volunteers is approximately 3.6 (+/-1.5) and 4.0 (+/-1.2) L/kg following intravenous and oral administration, respectively. MPA, at clinically relevant concentrations, is 97% bound to plasma albumin. MPAG is 82% bound to plasma albumin at MPAG concentration ranges that are normally seen in stable renal transplant patients; however, at higher MPAG concentrations (observed in patients with renal impairment or delayed renal graft function), the binding of MPA may be reduced as a result of competition between MPAG and MPA for protein binding. Mean blood to plasma ratio of radioactivity concentrations was approximately 0.6 indicating that MPA and MPAG do not extensively distribute into the cellular fractions of blood. For more Absorption, Distribution and Excretion (Complete) data for MYCOPHENOLATE MOFETIL (9 total), please visit the HSDB record page. Metabolism / Metabolites After both oral and intravenous administration mycophenolate mofetil is entirely metabolized by liver carboxylesterases 1 and 2 to mycophenolic acid (MPA), the active parent drug. It is then metabolized by the enzyme glucuronyl transferase, producing the inactive phenolic glucuronide of MPA (MPAG). The glucuronide metabolite is important, as it is then converted to MPA through enterohepatic recirculation. Mycophenolate mofetil that escapes metabolism in the intestine enters the liver via the portal vein and is transformed to pharmacologically active MPA in the liver cells.N-(2-carboxymethyl)-morpholine, N-(2-hydroxyethyl)-morpholine, and the N-oxide portion of N-(2-hydroxyethyl)-morpholine are additional metabolites of MMF occurring in the intestine as a result of liver carboxylesterase 2 activity. UGT1A9 and UGT2B7 in the liver are the major enzymes contributing to the metabolism of MPA in addition to other UGT enzymes, which also play a role in MPA metabolism. The four major metabolites of MPA are 7-O-MPA-β-glucuronide (MPAG, inactive), MPA acyl-glucuronide (AcMPAG), produced by uridine 5ʹ-diphosphate glucuronosyltransferases (UGT) activities, 7-O-MPA glucoside produced via UGT, and small amounts 6-O-des-methyl-MPA (DM-MPA) via CYP3A4/5 and CYP2C8 enzymes. Following oral and intravenous dosing, mycophenolate mofetil undergoes complete metabolism to MPA /mycophenolic acid/, the active metabolite. Metabolism to MPA occurs presystemically after oral dosing. MPA is metabolized principally by glucuronyl transferase to form the phenolic glucuronide of MPA (MPAG) which is not pharmacologically active. In vivo, MPAG is converted to MPA via enterohepatic recirculation. The following metabolites of the 2- hydroxyethyl-morpholino moiety are also recovered in the urine following oral administration of mycophenolate mofetil to healthy subjects: N-(2-carboxymethyl)-morpholine, N-(2- hydroxyethyl)-morpholine, and the N-oxide of N-(2-hydroxyethyl)-morpholine. Biological Half-Life The average apparent half-life of mycophenolate mofetil is 17.9 (±6.5) hours after oral administration and 16.6 (±5.8) hours after intravenous administration. For mycophenolic acid (MPA):Mean apparent: Approximately 17.9 hours after oral administration and 16.6 hours after intravenous administration. Mean (+/-SD) apparent half-life and plasma clearance of MPA are 17.9 (+/-6.5) hours and 193 (+/-48) mL/min following oral administration and 16.6 (+/-5.8) hours and 177 (+/-31) mL/min following intravenous administration, respectively. Pharmacokinetic Properties [2] Mycophenolate mofetil is well absorbed after oral administration and is rapidly converted to the active metabolite mycophenolic acid. The area under the plasma concentration-time curve (AUC) is generally proportional to dosage; however, there is some interpatient variation in values. The AUC and peak plasma concentration (Cmax) of mycophenolic acid are approximately 50% higher in stable renal transplant patients (>3 months post-transplantation) than in patients during the immediate post-transplant period. Mycophenolic acid is primarily eliminated (≈87%) in the urine as mycophenolic acid glucuronide; 6% is eliminated in the faeces. The mean ‘apparent’ half-life and plasma clearance of mycophenolic acid are 17.9 hours and 11.6 L/h, respectively, after oral administration. The AUC of mycophenolic acid and its glucuronide metabolite were higher in patients with renal impairment than in patients with normal renal function following single dose administration. However, the pharmacokinetic s of mycophenolic mofetil after a single dose are not altered in patients with cirrhosis. There are limited data in children but AUC and Cmax of mycophenolic acid appear to rise with increasing age. |
| 毒性/毒理 (Toxicokinetics/TK) |
Protein Binding
The protein binding of mycophenolic acid, the metabolite of mycophenolate mofetil, is 97% and it is mainly bound to albumin. MPAG, the inactive metabolite, is 82% bound to plasma albumin at normal therapeutic concentrations. At elevated MPAG concentrations due to various reasons, including renal impairment, the binding of MPA may be decreased due to competition for binding. Mycophenolate mofetil (the morpholinoethyl ester of mycophenolic acid) inhibits de novo purine synthesis via the inhibition of inosine monophosphate dehydrogenase. Its selective lymphocyte antiproliferative effects involve both T and B cells, preventing antibody formation. Mycophenolate mofetil has immunosuppressive effects alone, but is used most commonly in combination with other immunosuppressants. Mycophenolate mofetil, in combination with cyclosporin and corticosteroids, has been studied in large, randomised clinical trials involving nearly 1500 renal allograft transplant recipients. These trials demonstrated that mycophenolate mofetil is significantly more effective in reducing treatment failure and acute rejection episodes than placebo or azathioprine. Additionally, mycophenolate mofetil may be able to reduce the occurrence of chronic rejection. Mycophenolate mofetil is relatively well tolerated. The most common adverse effect reported is gastrointestinal intolerance; haematological aberrations have also been noted. The reversible cytostatic action of mycophenolate mofetil allows for dose adjustment or discontinuation, preventing serious toxicity or an overly suppressed immune system. Cytomegalovirus tissue invasive disease and the development of malignancies are concerns that merit evaluation in long term follow-up studies. Mycophenolate mofetil does not cause the adverse effects typically associated with other commercially available immunosuppressant medications such as nephrotoxicity, hepatotoxicity, hypertension, nervous system disturbances, electrolyte abnormalities, skin disorders, hyperglycaemia, hyperuricaemia, hypercholesterolaemia, lipid disorders and structural bone loss. Based on preliminary information, a positive benefit-risk ratio has been demonstrated with the use of mycophenolate mofetil in the prophylaxis of rejection in cadaveric renal allograft transplantation. Data from studies in other types of organ transplants are promising, but are too limited to draw clear conclusions. Long term follow-up studies are required to confirm these observations. Although mycophenolate mofetil is expensive, the beneficial effects on the reduction of rejection, treatment failure and related expenses suggest that it is most likely to be cost effective.[1] Tolerability [2] Rates of adverse events associated with mycophenolate mofetil appear to be dose related: 2 g/day is generally better tolerated than 3 g/day. Gastrointestinal (diarrhoea, vomiting), haematological and lymphatic (leucopenia, anaemia), and infectious (sepsis, opportunistic infections) events are most common. Diarrhoea and sepsis (most commonly cytomegalovirus viraemia) were slightly more common in patients receiving mycophenolate mofetil than in those receiving azathi-oprine. There was also an increased proportion of patients with leucopenia after treatment with mycophenolate mofetil 3 g/day compared with azathioprine treatment. The overall risk of malignancies associated with mycophenolate mofetil was similar to that of azathioprine. |
| 参考文献 |
|
| 其他信息 |
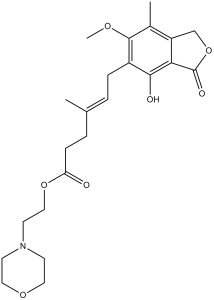
Mycophenolate mofetil is a carboxylic ester resulting from the formal condensation between the carboxylic acid group of mycophenolic acid and the hydroxy group of 2-(morpholin-4-yl)ethanol. In the liver, it is metabolised to mycophenolic acid, an immunosuppressant for which it is a prodrug. It is widely used to prevent tissue rejection following organ transplants as well as for the treatment of certain autoimmune diseases. It has a role as an immunosuppressive agent, a prodrug, an EC 1.1.1.205 (IMP dehydrogenase) inhibitor and an anticoronaviral agent. It is a gamma-lactone, a member of phenols, an ether, a carboxylic ester and a tertiary amino compound. It is functionally related to a mycophenolic acid and a 2-(morpholin-4-yl)ethanol.
Mycophenolate mofetil, also known as MMF or CellCept, is a prodrug of mycophenolic acid, and classified as a reversible inhibitor of inosine monophosphate dehydrogenase (IMPDH). This drug is an immunosuppressant combined with drugs such as [Cyclosporine] and corticosteroids to prevent organ rejection after hepatic, renal, and cardiac transplants. It is marketed by Roche Pharmaceuticals and was granted FDA approval for the prophylaxis of transplant rejection in 1995. In addition to the above uses, mycophenolate mofetil has also been studied for the treatment of nephritis and other complications of autoimmune diseases. Unlike another immunosuppressant class, the calcineurin inhibitors, MMF generally does not cause nephrotoxicity or fibrosis. Previously, mycophenolic acid (MPA) was administered to individuals with autoimmune diseases beginning in the 1970s, but was discontinued due to gastrointestinal effects and concerns over carcinogenicity. The new semi-synthetic 2-morpholinoethyl ester of MPA was synthesized to avoid the gastrointestinal effects associated with the administration of MPA. It demonstrates an increased bioavailability, a higher efficacy, and reduced gastrointestinal effects when compared to MPA. Mycophenolate Mofetil is the morpholinoethyl ester of mycophenolic acid (MPA) with potent immunosuppressive properties. Mycophenolate stops T-cell and B-cell proliferation through selective inhibition of the de novo pathway of purine biosynthesis. In vivo, the active metabolite, MPA, reversibly inhibits inosine 5'-monophosphate dehydrogenase, an enzyme involved in the de novo synthesis of guanine nucleotides. MPA displays high lymphocyte specificity and cytotoxicity due to the higher dependence of activated lymphocytes on both salvage and de novo synthesis of guanine nucleotides relative to other cell types. (NCI04) Compound derived from Penicillium stoloniferum and related species. It blocks de novo biosynthesis of purine nucleotides by inhibition of the enzyme inosine monophosphate dehydrogenase (IMP DEHYDROGENASE). Mycophenolic acid exerts selective effects on the immune system in which it prevents the proliferation of T-CELLS, LYMPHOCYTES, and the formation of antibodies from B-CELLS. It may also inhibit recruitment of LEUKOCYTES to sites of INFLAMMATION. See also: Mycophenolic Acid (has active moiety); Mycophenolate Mofetil Hydrochloride (has salt form). Drug Indication Mycophenolate mofetil is indicated in combination with other immunosuppressants to prevent the rejection of kidney, heart, or liver transplants in adult and pediatric patients ≥3 months old. Mycophenolate mofetil may also be used off-label as a second-line treatment for autoimmune hepatitis that has not responded adequately to first-line therapy. Other off-label uses of this drug include lupus-associated nephritis and dermatitis in children. FDA Label CellCept is indicated in combination with ciclosporin and corticosteroids for the prophylaxis of acute transplant rejection in patients receiving allogeneic renal, cardiac or hepatic transplants. Myfenax is indicated in combination with ciclosporin and corticosteroids for the prophylaxis of acute transplant rejection in patients receiving allogeneic renal, cardiac or hepatic transplants. Myclausen is indicated in combination with ciclosporin and corticosteroids for the prophylaxis of acute transplant rejection in patients receiving allogeneic renal, cardiac or hepatic transplants. , Mycophenolate mofetil Teva is indicated in combination with ciclosporin and corticosteroids for the prophylaxis of acute transplant rejection in patients receiving allogeneic renal, cardiac or hepatic transplants. Mechanism of Action The active metabolite of mycophenolate, mycophenolic acid, prevents T-cell and B-cell proliferation and the production of cytotoxic T-cells and antibodies. Lymphocyte and monocyte adhesion to endothelial cells of blood vessels that normally part of inflammation is prevented via the glycosylation of cell adhesion molecules by MPA. MPA inhibits de novo purine biosynthesis (that promotes immune cell proliferation) by inhibiting inosine 5’-monophosphate dehydrogenase enzyme (IMPDH), with a preferential inhibition of IMPDH II. IMPDH normally transforms inosine monophosphate (IMP) to xanthine monophosphate (XMP), a metabolite contributing to the production of guanosine triphosphate (GTP). GTP is an important molecule for the synthesis of ribonucleic acid (RNA), deoxyribonucleic acid (DNA), and protein. As a result of the above cascade of effects, mycophenolate mofetil reduces de-novo production of guanosine nucleotides, interfering with the synthesis of DNA, RNA, and protein required for immune cell production. Further contributing to the above anti-inflammatory effects, MMF depletes tetrahydrobiopterin, causing the decreased function of inducible nitric oxide synthase enzyme, in turn decreasing the production of peroxynitrite, a molecule that promotes inflammation. As a potent, selective, noncompetitive, and reversible, inhibitor of inosine monophosphate dehydrogenase (IMPDH), mycophenolic acid (MPA), the active metabolite /of mycophenolate mofetil/, inhibits the de novo synthesis pathway of guanosine nucleotides without being incorporated into DNA. Because T and B lymphocytes are critically dependent for their proliferation on de novo synthesis of purines, while other cell types can utilize salvage pathways, MPA has potent cytostatic effects on lymphocytes. MPA inhibit proliferative responses of T and B lymphocytes to both mitogenic and allospecific stimulation. The addition of guanosine or deoxyguanosine reverses the cytostatic effects of MPA on lymphocytes. MPA also suppresses antibody formation by B lymphocytes. MPA prevents the glycosylation of lymphocytes and monocyte glycoproteins that are involved in intercellular adhesion of these cells to endothelial cells, and may inhibit recruitment of leukocytes into sites of inflammation and graft rejection. Mycophenolate mofetil dose not inhibit the early events in the activation of human peripheral blood mononuclear cells, such as the production of interleukin-1 and interleukin-2, but does block the coupling of these events to DNA synthesis and proliferation. Mycophenolate mofetil (the morpholinoethyl ester of mycophenolic acid) inhibits de novo purine synthesis via the inhibition of inosine monophosphate dehydrogenase. Its selective lymphocyte antiproliferative effects involve both T and B cells, preventing antibody formation. Mycophenolate mofetil has immuno-suppressive effects alone, but is used most commonly in combination with other immunosuppressants. Mycophenolate mofetil, in combination with cyclosporin and corticosteroids, has been studied in large, randomised clinical trials involving nearly 1500 renal allograft transplant recipients. These trials demonstrated that mycophenolate mofetil is significantly more effective in reducing treatment failure and acute rejection episodes than placebo or azathioprine. Additionally, mycophenolate mofetil may be able to reduce the occurrence of chronic rejection. Mycophenolate mofetil is relatively well tolerated. The most common adverse effect reported is gastrointestinal intolerance; haematological aberrations have also been noted. The reversible cytostatic action of mycophenolate mofetil allows for dose adjustment or discontinuation, preventing serious toxicity or an overly suppressed immune system. Cytomegalovirus tissue invasive disease and the development of malignancies are concerns that merit evaluation in long term follow-up studies. Mycophenolate mofetil does not cause the adverse effects typically associated with other commercially available immunosuppressant medications such as nephrotoxicity, hepatotoxicity, hypertension, nervous system disturbances, electrolyte abnormalities, skin disorders, hyperglycaemia, hyperuricaemia, hypercholesterolaemia, lipid disorders and structural bone loss. Based on preliminary information, a positive benefit-risk ratio has been demonstrated with the use of mycophenolate mofetil in the prophylaxis of rejection in cadaveric renal allograft transplantation. Data from studies in other types of organ transplants are promising, but are too limited to draw clear conclusions. Long term follow-up studies are required to confirm these observations. Although mycophenolate mofetil is expensive, the beneficial effects on the reduction of rejection, treatment failure and related expenses suggest that it is most likely to be cost effective.[1] Compound derived from Penicillium stoloniferum and related species. It blocks de novo biosynthesis of purine nucleotides by inhibition of the enzyme inosine monophosphate dehydrogenase (IMP DEHYDROGENASE). Mycophenolic acid exerts selective effects on the immune system in which it prevents the proliferation of T-CELLS, LYMPHOCYTES, and the formation of antibodies from B-CELLS. It may also inhibit recruitment of LEUKOCYTES to sites of INFLAMMATION. See also: Mycophenolic Acid (has active moiety); Mycophenolate Mofetil (is salt form of). In summary, our results indicate that MMF: (i) inhibits the secretion of TNF-α, IL-1β and NO of microglial cells; (ii) inhibits TNF-α secretion of astrocytes; (iii) suppresses the proliferation of microglial cells and astrocytes; (iv) has no direct neuroprotective effects on cultured, excitotoxically injured hippocampal neurones; and (v) acts by inhibiting glial IMPDH. Against a background of promising animal experiments and open label clinical trials on the use of MMF in various CNS disorders, MMF seems to be a promising candidate for further investigations on the treatment of acute brain and spinal cord pathologies.[4] MMF and DCZ, which target T lymphocytes, inhibit inflammatory activity, and thus prevent the development of skin fibrosis in early stages of a mouse model of BLM‐induced scleroderma. However, MMF is more effective at suppressing fibroblastic activation than in DCZ, and has a more prominent antifibrotic effect. These results support the assumption that T lymphocytes play an important role in the pathogenesis of scleroderma, and that suppression of T lymphocytes may be an effective strategy for treatment of human scleroderma, when started during the early stages of the disease. However, targeting T lymphocytes alone may not be an adequate treatment approach for scleroderma.[5] |
| 分子式 |
C23H31NO7
|
|---|---|
| 分子量 |
433.4947
|
| 精确质量 |
433.21
|
| 元素分析 |
C, 63.73; H, 7.21; N, 3.23; O, 25.83
|
| CAS号 |
128794-94-5
|
| 相关CAS号 |
Mycophenolate Mofetil-d4;1132748-21-0;Mycophenolate mofetil hydrochloride;116680-01-4
|
| PubChem CID |
5281078
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
1.2±0.1 g/cm3
|
| 沸点 |
637.6±55.0 °C at 760 mmHg
|
| 熔点 |
95-96ºC
|
| 闪点 |
339.4±31.5 °C
|
| 蒸汽压 |
0.0±2.0 mmHg at 25°C
|
| 折射率 |
1.557
|
| LogP |
3.15
|
| tPSA |
94.53
|
| 氢键供体(HBD)数目 |
1
|
| 氢键受体(HBA)数目 |
8
|
| 可旋转键数目(RBC) |
10
|
| 重原子数目 |
31
|
| 分子复杂度/Complexity |
646
|
| 定义原子立体中心数目 |
0
|
| SMILES |
O1C([H])([H])C([H])([H])N(C([H])([H])C([H])([H])OC(C([H])([H])C([H])([H])/C(/C([H])([H])[H])=C(\[H])/C([H])([H])C2C(=C3C(=O)OC([H])([H])C3=C(C([H])([H])[H])C=2OC([H])([H])[H])O[H])=O)C([H])([H])C1([H])[H]
|
| InChi Key |
RTGDFNSFWBGLEC-SYZQJQIISA-N
|
| InChi Code |
InChI=1S/C23H31NO7/c1-15(5-7-19(25)30-13-10-24-8-11-29-12-9-24)4-6-17-21(26)20-18(14-31-23(20)27)16(2)22(17)28-3/h4,26H,5-14H2,1-3H3/b15-4+
|
| 化学名 |
2-morpholin-4-ylethyl (E)-6-(4-hydroxy-6-methoxy-7-methyl-3-oxo-1H-2-benzofuran-5-yl)-4-methylhex-4-enoate
|
| 别名 |
RS61443; Mycophenolic acid; mycophenolate mofetil; 128794-94-5; 115007-34-6; Myfenax; myclausen; Mycophenylate mofetil; Mycophenolic acid morpholinoethyl ester; Mycophenolate mofetil Teva; Mycophenolate mofetil, Cellcept, Myfortic, RS-61443;Mycophenolate mofetil (free acid);
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (5.77 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (5.77 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (5.77 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: 0.5% methylcellulose:20 mg/mL 配方 5 中的溶解度: 33.33 mg/mL (76.89 mM) in Cremophor EL (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶. 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.3069 mL | 11.5343 mL | 23.0686 mL | |
| 5 mM | 0.4614 mL | 2.3069 mL | 4.6137 mL | |
| 10 mM | 0.2307 mL | 1.1534 mL | 2.3069 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT05627739 | Recruiting | Drug: Mycophenolate Mofetil | Vogt-Koyanagi-Harada Disease Mycophenolate Mofetil |
October 1, 2021 | August 23, 2017 | |
| NCT03200002 | Completed | Drug: Cyclophosphamide Drug: Mycophenolate Mofetil |
To Compare the Effects of Mycophenolate Mofetil With Cyclophosphamide in Neplaese Lupus Nephritis Patients |
Chitwan Medical College | January 1, 2014 | Phase 2 |
| NCT03678987 | Completed | Diagnostic Test: P-MPA concentration Drug: mycophenolic acid |
Systemic Sclerosis Gastrointestinal Complication |
Region Skane | September 13, 2018 | |
| NCT02743247 | Completed | Drug: Tacrolimus Drug: Mycophenolate mofetil |
Healthy Volunteers | Seoul National University Hospital | October 2015 | Phase 1 |