| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| Other Sizes |
|
| 靶点 |
G-quadruplexe (Kd = 490 nM)
|
|---|---|
| 体外研究 (In Vitro) |
Pyridostatin (RR82) 盐酸盐(10 μM;48 小时)可诱导细胞周期停滞[1]。
Pyridostatin 盐酸盐是一种小分子,可选择性结合 G-四链体 DNA,形成稳定 G-四链体结构的复合物。盐酸吡啶他汀会引起神经突回缩、突触丧失和剂量依赖性神经元死亡。 PyridostatinHCl 可诱导培养的原代神经元中 DNA 双链断裂的形成。保护和固定神经元基因组的 BRCA1 蛋白在转录水平上被盐酸吡咯抑素(1–5 μM,过夜)显着下调[3]。 |
| 体内研究 (In Vivo) |
Pyridostatin对BRCA2缺陷异种移植物具有抗肿瘤活性[4]
结合和稳定G4s的化合物已被证明对小鼠建立的BRCA1/2缺失异种移植物肿瘤有活性(RHPS4和CX‐5461)。然而,这些尚未被证明对BRCA突变患者有益。此外,BRCA突变的肿瘤很难治疗,因为它们对靶向治疗(例如PARP抑制剂;PARPi)。因此,必须找到新的G4配体,不仅可以消除BRCA缺陷肿瘤,还可以抵抗耐药疾病。我们之前发表的结果(Zimmer et al, 2016)表明,G4配体pyridostatin对体外BRCA2缺陷细胞具有特异性毒性。在这项研究中,研究人员评估了pyridostatin在体内消除BRCA2缺陷异种移植物肿瘤中的潜力。为了解决这个问题,我们使用等基因BRCA2 +/+ (BRCA2‐精通)和BRCA2−/−(BRCA2‐缺乏)人结直肠癌DLD1细胞在CB17‐SCID小鼠中产生异种移植物(图1A和B)。研究人员广泛优化了pyridostatin在体内使用的条件,并确定了7.5 mg/kg/天的剂量计划静脉注射连续5天,然后休息2天,第二个5天的治疗耐受性良好。没有明显的体重减轻,没有不良的临床症状(附录表S1)。在这些条件下,研究人员发现pyridostatin有效且特异性地抑制BRCA2‐缺陷DLD1细胞建立的异种移植物肿瘤的生长(图1B)。作为对照,研究人员使用了PARPi talazoparib,该药物以其根除小鼠BRCA1/2缺失肿瘤的能力而闻名(Shen et al ., 2013),最近被许可用于携带BRCA1/2种系突变的转移性乳腺癌患者(Litton et al ., 2018)。pyridostatin对BRCA2 -缺陷肿瘤的抗肿瘤作用与talazoparib相似,两种药物都不会损害BRCA2 -精通肿瘤的生长。 此外,研究人员使用第二种肿瘤模型研究了pyridostatin在体内的反应,该模型是由等基因BRCA2 +/+和BRCA2 - / -结直肠癌HCT116细胞建立的(Xu et al ., 2014)。Pyridostatin显示出对BRCA2缺失HCT116细胞源性肿瘤的选择性毒性(附录图S1A和B;附录表S2),其作用与DLD1细胞来源的异种移植物相似[4] 研究人员之前的研究表明,pyridostatin治疗会导致HR修复受损的细胞(包括BRCA2缺陷细胞)中DNA损伤的积累(Zimmer等,2016)。一致地,免疫组织化学(IHC)分析显示,BRCA2‐缺乏,但不是BRCA2‐完全,肿瘤在暴露于pyridostatin或talazoparib时显示出DNA损伤标记γH2AX水平增加(附录图S1C-F)。这些结果表明,pyridostatin不仅可以特异性抑制细胞的生长(Zimmer等,2016),还可以特异性抑制缺乏BRCA2的肿瘤,并通过造成DNA损伤在体内起作用[4]。 |
| 细胞实验 |
细胞系: 超过 60 种不同的癌细胞系
浓度: 10 μM 孵育时间: 48 小时 结果: 主要在超过 60 种不同的癌细胞系的细胞周期的 G2 期积累。 |
| 动物实验 |
CB17‐SCID mice
7.5 mg/kg i.v. In vivo xenograft experiments[4] CB17‐SCID mice (CB17/Icr‐Prkdcscid/IcrIcoCrl, male or female), FVB female mice were purchased from Charles River Laboratories. The mice were maintained in high‐efficiency, particulate air HEPA‐filtered racks and were fed autoclaved laboratory rodent diet.[4] To generate xenografts derived from DLD1 and HCT116 BRCA2‐proficient or ‐deficient cells, CB17‐SCID male mice 6 weeks old were injected intramuscularly, into the hind leg muscles, with 5 × 106 cells per mouse. When a tumour volume of approximately 250 mm3 was evident, mice were randomised to start the treatments.[4] To generate the PARPi‐resistant mouse tumour model, FVB female mice 6 weeks old were injected intramuscularly into the hind leg muscles with 4 × 106 KP3.33 (Brca1 +/+) cells or KB1PM5 (Brca1 −/− Tp53bp1 −/−) mouse mammary tumour cells. Each experimental group included five mice. When a tumour volume of approximately 250 mm3 was evident, mice were randomised and the treatment started.[4] To generate xenografts derived from MDA‐MB‐436 cells, CB17‐SCID female mice 6 weeks old were injected intramuscularly with 4 × 106 cells per mouse. When a tumour volume of approximately 220 mm3 was evident (6 days after cell injection), treatment was initiated. Each experimental group included five mice.[4] Talazoparib (BMN 673, Selleckchem) was dissolved in 10% of dimethylacetamide, 6% of solutol HS, 84% of PBS and administered orally at doses of 0.33 mg/kg/day for five consecutive days, followed by 2‐day break and five more days of treatment (Wang et al, 2016). pyridostatin was dissolved in saline solution and administered intravenously at doses of 7.5 mg/kg/day for five consecutive days, followed by 2‐day break and five more days of treatment. NU‐7441 (Selleckchem) was dissolved in 5% of DMSO, 40% PEG300, 5% of Tween‐80 and administered intraperitoneally at doses of 10 mg/kg/day for five consecutive days, followed by 2‐day break and five more days of treatment (Zhao et al, 2006). Paclitaxel was dissolved in saline solution and administered intravenously at doses of 20 mg/kg/day at day 1 and day 8 of treatment (Bizzaro et al, 2018). When combined with other compounds, paclitaxel was administered intravenously at day 5 and 12 of treatment, pyridostatin and NU‐7441 were administered intravenously and intraperitoneally, respectively, for four consecutive days, followed by a 3‐day break and four more days of treatment. NU‐7441 was administered 2 h before pyridostatin. At indicated time points, tumour volumes were measured in two dimensions using a caliper and tumour weight was estimated from tumour volume (1 mg = 1 mm3). The student’s t‐test (unpaired, two‐tailed) was used for single pair‐wise comparisons. Differences were considered statistically significant when P < 0.05. Survival curves of mice were processed using the Kaplan–Meier method, and statistical significance was assessed by log‐rank test. Data were plotted using GraphPad Prism Software 8.3.[4] Generation of PDTX models[4] Fresh tumour samples from patients with gBRCA breast cancer were prospectively collected for implantation into mice under an institutional IRB‐approved protocol and the associated informed consent, or by the National Research Ethics Service, Cambridgeshire 2 REC (REC reference number: 08/H0308/178) (Bruna et al, 2016). The VHI0179 patient‐derived tumour xenografts (PDTXs) were generated from a patient breast tumour with a BRCA1 germline truncation and resistant to Olaparib due to REV7 mutation. Written informed consent was obtained from all patients and the experiments conformed to the principles set out in the WMA Declaration of Helsinki and the Department of Health and Human Services Belmont Report. Frozen tumour fragments (15–20 mm3) were coated in Matrigel and implanted using a small incision in a subcutaneous pocket made in one side of the lower back into one CB17‐SCID female mice 6 weeks old. When the tumour reached approximately 400 mm3, tumour was explanted from the sacrificed mouse, cut into fragments of about 15–20 mm3 and implanted again subcutaneously in fourteen CB17‐ SCID female mice. When the tumour reached approximately 200 mm3, mice were randomised in vehicle and treated group to start the treatments. Each experimental group included seven mice. |
| 参考文献 |
|
| 其他信息 |
Ligands that stabilize the formation of telomeric DNA G-quadruplexes have potential as cancer treatments, because the G-quadruplex structure cannot be extended by telomerase, an enzyme over-expressed in many cancer cells. Understanding the kinetic, thermodynamic and mechanical properties of small-molecule binding to these structures is therefore important, but classical ensemble assays are unable to measure these simultaneously. Here, we have used a laser tweezers method to investigate such interactions. With a force jump approach, we observe that pyridostatin promotes the folding of telomeric G-quadruplexes. The increased mechanical stability of pyridostatin-bound G-quadruplex permits the determination of a dissociation constant K(d) of 490 ± 80 nM. The free-energy change of binding obtained from a Hess-like process provides an identical K(d) for pyridostatin and a K(d) of 42 ± 3 µM for a weaker ligand RR110. We anticipate that this single-molecule platform can provide detailed insights into the mechanical, kinetic and thermodynamic properties of liganded bio-macromolecules, which have biological relevance.[1]
Guanine-rich DNA sequences that can adopt non-Watson-Crick structures in vitro are prevalent in the human genome. Whether such structures normally exist in mammalian cells has, however, been the subject of active research for decades. Here we show that the G-quadruplex-interacting drug pyridostatin promotes growth arrest in human cancer cells by inducing replication- and transcription-dependent DNA damage. A chromatin immunoprecipitation sequencing analysis of the DNA damage marker γH2AX provided the genome-wide distribution of pyridostatin-induced sites of damage and revealed that pyridostatin targets gene bodies containing clusters of sequences with a propensity for G-quadruplex formation. As a result, pyridostatin modulated the expression of these genes, including the proto-oncogene SRC. We observed that pyridostatin reduced SRC protein abundance and SRC-dependent cellular motility in human breast cancer cells, validating SRC as a target of this drug. Our unbiased approach to define genomic sites of action for a drug establishes a framework for discovering functional DNA-drug interactions.[2] Viruses that establish latent infections have evolved unique mechanisms to avoid host immune recognition. Maintenance proteins of these viruses regulate their synthesis to levels sufficient for maintaining persistent infection but below threshold levels for host immune detection. The mechanisms governing this finely tuned regulation of viral latency are unknown. Here we show that mRNAs encoding gammaherpesviral maintenance proteins contain within their open reading frames clusters of unusual structural elements, G-quadruplexes, which are responsible for the cis-acting regulation of viral mRNA translation. By studying the Epstein-Barr virus-encoded nuclear antigen 1 (EBNA1) mRNA, we demonstrate that destabilization of G-quadruplexes using antisense oligonucleotides increases EBNA1 mRNA translation. In contrast, pretreatment with a G-quadruplex-stabilizing small molecule, pyridostatin, decreases EBNA1 synthesis, highlighting the importance of G-quadruplexes within virally encoded transcripts as unique regulatory signals for translational control and immune evasion. Furthermore, these findings suggest alternative therapeutic strategies focused on targeting RNA structure within viral ORFs.[3] The cells with compromised BRCA1 or BRCA2 (BRCA1/2) function accumulate stalled replication forks, which leads to replication-associated DNA damage and genomic instability, a signature of BRCA1/2-mutated tumours. Targeted therapies against BRCA1/2-mutated tumours exploit this vulnerability by introducing additional DNA lesions. Because homologous recombination (HR) repair is abrogated in the absence of BRCA1 or BRCA2, these lesions are specifically lethal to tumour cells, but not to the healthy tissue. Ligands that bind and stabilise G-quadruplexes (G4s) have recently emerged as a class of compounds that selectively eliminate the cells and tumours lacking BRCA1 or BRCA2. Pyridostatin is a small molecule that binds G4s and is specifically toxic to BRCA1/2-deficient cells in vitro. However, its in vivo potential has not yet been evaluated. Here, we demonstrate that pyridostatin exhibits a high specific activity against BRCA1/2-deficient tumours, including patient-derived xenograft tumours that have acquired PARP inhibitor (PARPi) resistance. Mechanistically, we demonstrate that pyridostatin disrupts replication leading to DNA double-stranded breaks (DSBs) that can be repaired in the absence of BRCA1/2 by canonical non-homologous end joining (C-NHEJ). Consistent with this, chemical inhibitors of DNA-PKcs, a core component of C-NHEJ kinase activity, act synergistically with pyridostatin in eliminating BRCA1/2-deficient cells and tumours. Furthermore, we demonstrate that pyridostatin triggers cGAS/STING-dependent innate immune responses when BRCA1 or BRCA2 is abrogated. Paclitaxel, a drug routinely used in cancer chemotherapy, potentiates the in vivo toxicity of pyridostatin. Overall, our results demonstrate that pyridostatin is a compound suitable for further therapeutic development, alone or in combination with paclitaxel and DNA-PKcs inhibitors, for the benefit of cancer patients carrying BRCA1/2 mutations.[4] |
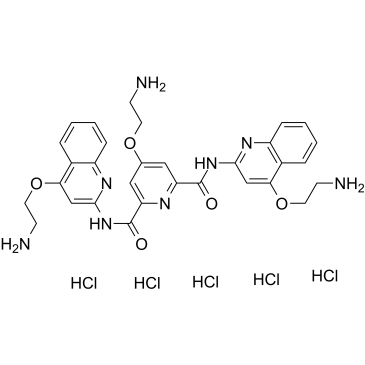
| 分子式 |
C31H37CL5N8O5
|
|---|---|
| 分子量 |
778.9411
|
| 精确质量 |
778.13
|
| CAS号 |
1781882-65-2
|
| 相关CAS号 |
Pyridostatin;1085412-37-8;Pyridostatin TFA;1472611-44-1
|
| PubChem CID |
78243739
|
| 外观&性状 |
White to off-white solid
|
| tPSA |
203
|
| 氢键供体(HBD)数目 |
10
|
| 氢键受体(HBA)数目 |
11
|
| 可旋转键数目(RBC) |
13
|
| 重原子数目 |
49
|
| 分子复杂度/Complexity |
850
|
| 定义原子立体中心数目 |
0
|
| InChi Key |
SRIZPFGTXSQRFM-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C31H32N8O5.5ClH/c32-9-12-42-19-15-24(30(40)38-28-17-26(43-13-10-33)20-5-1-3-7-22(20)36-28)35-25(16-19)31(41)39-29-18-27(44-14-11-34)21-6-2-4-8-23(21)37-29;;;;;/h1-8,15-18H,9-14,32-34H2,(H,36,38,40)(H,37,39,41);5*1H
|
| 化学名 |
4-(2-aminoethoxy)-2-N,6-N-bis[4-(2-aminoethoxy)quinolin-2-yl]pyridine-2,6-dicarboxamide;pentahydrochloride
|
| 别名 |
RR82 hydrochloride; Pyridostatin hydrochloride; 1781882-65-2; Pyridostatin (hydrochloride); RR82 hydrochloride; 4-(2-aminoethoxy)-2-N,6-N-bis[4-(2-aminoethoxy)quinolin-2-yl]pyridine-2,6-dicarboxamide;pentahydrochloride; Pyridostatin pentahydrochloride; RR-82 hydrochloride; 4-(2-aminoethoxy)-N2,N6-bis[4-(2-aminoethoxy)quinolin-2-yl]pyridine-2,6-dicarboxamide pentahydrochloride
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中(例如氮气保护),避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
H2O: ~50 mg/mL (~64.2 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 100 mg/mL (128.38 mM) in PBS (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶。
请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.2838 mL | 6.4190 mL | 12.8380 mL | |
| 5 mM | 0.2568 mL | 1.2838 mL | 2.5676 mL | |
| 10 mM | 0.1284 mL | 0.6419 mL | 1.2838 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
|
|
|
|
|