| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 10mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| 5g |
|
||
| 10g |
|
||
| Other Sizes |
|
| 靶点 |
VEGFR3 (IC50 = 20 nM); Braf (IC50 = 22 nM); Raf-1 (IC50 = 6 nM); VEGFR2 (IC50 = 90 nM); PDGFRβ (IC50 = 57 nM); BrafV599E (IC50 = 38 nM); c-Kit (IC50 = 68 nM); Flt3 (IC50 = 58 nM)
|
|---|---|
| 体外研究 (In Vitro) |
索拉非尼的 IC50 值分别为 22 nM 和 38 nM,抑制野生型和 V599E 突变体 B-Raf 活性。此外,mVEGFR2 (Flk-1) 以及 mVEGFR3、mPDGFRβ、Flt3 和 c-Kit 均被索拉非尼有效抑制,IC50 值分别为 15 nM、20 nM、57 nM、58 nM 和 68 nM。索拉非尼的 IC50 为 580 nM,仅中度抑制 FGFR-1。甲苯磺酸索拉非尼对以下靶标无效:ERK-1、MEK-1、EGFR、HER-2、IGFR-1、c-Met、PKB、PKA、cdk1/cyclinB、PKCα、PKCγ 和 pim-1。在 NIH 3T3 细胞中,索拉非尼显着降低 VEGFR2 磷酸化(IC50 为 30 nM),并显着降低 HEK-293 细胞中 Flt-3 磷酸化(IC50 为 20 nM)。在大多数细胞系中,索拉非尼有效抑制 MEK 1/2 和 ERK 1/2 磷酸化,但在 A549 或 H460 细胞中则不然。它对PKB途径的抑制没有影响。 Sorafenib 的 IC50 分别为 0.28 μM 和 2.6 μM,可防止 HAoSMC 和 MDA-MB-231 细胞增殖。 [1] 除了抑制 RAF/MEK/ERK 信号通路外,索拉非尼还以不依赖于 MEK/ERK 的方式显着抑制 eIF4E 磷酸化并下调肝细胞癌 (HCC) 细胞中的 Mcl-1 水平。索拉非尼的 IC50 值分别为 6.3 μM 和 4.5 μM,抑制 PLC/PRF/5 和 HepG2 细胞的增殖,并显着诱导细胞凋亡。 [2]
|
| 体内研究 (In Vivo) |
口服索拉非尼 (60 mg/kg) 对多种人类肿瘤异种移植模型(包括 MDA-MB-231、Colo-205、HT-29、DLD-1)没有毒性,且具有广谱、剂量依赖性抗肿瘤活性、NCI-H460 和 A549。索拉非尼治疗显着降低 MDA MB-231、HT-29 和 Colo-205 肿瘤异种移植物中的肿瘤微血管面积(MVA)和微血管密度(MVD),这与其抗肿瘤功效相关。然而,它对 HT-29 或 MDA-MB-231 异种移植物中的 MEK 1/2 磷酸化或 pERK 1/2 水平没有影响。 [1]在 SCID 小鼠中,索拉非尼治疗导致 PLC/PRF/5 肿瘤异种移植物的剂量依赖性生长抑制,10 mg/kg 和 30 mg/kg 时的 TGI 分别为 49% 和 78%。这与抑制 ERK 和 eIF4E 磷酸化、减少微血管面积以及诱导肿瘤细胞凋亡相一致。 [2] 通过抑制 NF-B 介导的 Mcl-1 和 cIAP2 表达,索拉非尼以剂量依赖性方式使 bax-/- 细胞对 TRAIL 敏感。在 TRAIL 耐药的 HCT116 bax-/- 和 HT29 肿瘤异种移植物中,索拉非尼 (30-60 mg/kg) 和 TRAIL (5 mg/kg) 显示出显着的疗效。 [3]
|
| 酶活实验 |
将 Raf-1 (80 ng)、wt BRAF (80 ng) 或 V599E BRAF (80 ng) 与 MEK-1 (1 μg) 在测定缓冲液(20 mM Tris (pH 8.2)、100 mM NaCl、5 mM MgCl2 和 0.15% β-巯基乙醇)以测试该化合物对不同 RAF 激酶亚型的影响。添加 25 μL 10 μM γ-[33P]ATP (400 Ci/mol) 并将混合物在 32°C 下孵育 25 分钟,启动 RAF 激酶测定(最终体积为 50 μL)。通过将磷酸化的 MEK-1 过滤到磷酸纤维素垫上,未与蛋白质结合的放射性被去除。然后收获磷酸化的 MEK-1。使用 β 板计数器,在微波加热干燥后测量过滤器结合的放射性。
|
| 细胞实验 |
72 小时内,甲苯磺酸索拉非尼以逐渐升高的浓度注入细胞。 Cell TiterGlo ATP 发光检测试剂盒用于计算细胞数量。该测定通过测量发光信号来计算每个孔中的活细胞数量,该信号取决于细胞 ATP 的量。
|
| 动物实验 |
Mice: Female NCr-nu/nu mice are used. Mice bearing 75 to 150 mg tumors are treated orally with Sorafenib (7.5 to 60 mg/kg), administered daily for 9 days. In each model, Sorafenib produces dose-dependent tumor growth inhibition with no evidence of toxicity, as measured by increased weight loss relative to control animals or drug-related lethality. In parallel to the antitumor efficacy studies, additional groups of four mice bearing 100 to 200 mg tumors are treated orally with vehicle or Sorafenib (30 to 60 mg/kg), administered daily for 5 days, which is the shortest treatment duration producing complete tumor stasis in the treated groups.
Rats: Male albino rats weighing 100 to 120 g are used for the study. Rats are weighed and randomly split into three groups following an acclimatization period. For 8 weeks, the car is given daily to Group 1 (the healthy control group; n=10). An i.p. single dose of 200 mg/kg DENA is administered to Group 2 (the DENA group; n=15). Six weeks after receiving a DENA intravenously in Group 3 (the Sorafenib group; n=12), Sorafenib is administered orally at a dose of 10 mg/kg daily for two weeks. Rats are weighed, put to sleep with ether, killed at the conclusion of the experiment (8 weeks), and their livers are removed. Fresh liver is weighed after being dried on a clean paper towel and going through two ice-cold saline washes. The liver index is calculated using the formula liver weight (g)/final body weight (g)×100. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
The administration of multiple doses for seven days resulted in a 2.5- to 7-fold accumulation compared to a single dose. Steady-state concentrations were achieved within seven days, with a peak-to-trough ratio of mean concentrations of less than 2. Mean Cmax and AUC increased less than proportionally beyond oral doses of 400 mg administered twice daily. The Tmax is approximately three hours. The mean relative bioavailability was 38–49% following the administration of oral sorafenib tablets. A high-fat meal reduced bioavailability by 29%. Following oral administration of a 100 mg dose of sorafenib, about 96% of the dose was recovered within 14 days, with 77% of the dose being excreted in feces and 19% of the dose being excreted in urine as glucuronidated metabolites. Unchanged sorafenib accounted for 51% of the dose excreted in feces. Sorafenib is widely distributed to tissues, indicating that it is lipophilic. Following oral administration of a 100 mg dose of a solution formulation of sorafenib, 96% of the dose was recovered within 14 days, with 77% of the dose excreted in feces and 19% of the dose excreted in urine as glucuronidated metabolites. Unchanged sorafenib, accounting for 51% of the dose, was found in feces but not in urine. After administration of Nexavar tablets, the mean relative bioavailability was 38-49% when compared to an oral solution. Following oral administration, sorafenib reached peak plasma levels in approximately 3 hours. With a moderate-fat meal (30% fat; 700 calories), bioavailability was similar to that in the fasted state. With a high-fat meal (50% fat; 900 calories), bioavailability was reduced by 29% compared to that in the fasted state. It is recommended that Nexavar be administered without food. Mean Cmax and AUC increased less than proportionally beyond oral doses of 400 mg administered twice daily. In vitro binding of sorafenib to human plasma proteins was 99.5%. The absorption and the basic pharmacokinetics following a single dose of sorafenib tosylate were evaluated in female CD-1 mice, male Wistar rats, and female Beagle dogs. For the determination of the absorption of sorafenib in rats, bile duct-cannulated rats (n=5/group) were used. Twenty-four hours after surgery (14)C-sorafenib tosylate was administered orally or intravenously to the rats at a dose of 5 mg/kg sorafenib. The absorption of sorafenib was almost complete in female CD-1 mice (78.6%) and male Wistar rats (79.2%). In Beagle dogs the absorption (67.6 %, calculated from AUC norm values after intravenous and oral administration) and the absolute bioavailability (59.9 %) were lower than in rodents. Maximum plasma concentrations of radioactivity between 1.5 hr and 2 hr after oral administration were observed in all species. After intravenous administration of (14)C-sorafenib tosylate to mice, rats, and dogs the elimination of the radioactivity from plasma occurred with similar terminal half-lives of 6.8, 8.8, and 7.3 hours, respectively. The terminal half-lives of radioactivity after oral administration were 6.1 hours in mice and 5.8 hours in dogs. In rats, terminal half-live after oral administration was longer (11.2 hr) than after intravenous administration. In rats, the elimination of the unchanged compound was slower (half life: 9.3 hr) than in the mice (half life: 6.5 hr) and dogs (half life:4.3 hr). The total plasma clearance in rats was 0.044 L/(hr/kg) corresponding to a blood clearance of 0.049 L/(hr/kg). In mice and dogs the total plasma clearance was 0.13 and 0.15 lL/(hr/kg) respectively. The volume of distribution at steady state ranged from 0.65 l/kg to 0.74 l/kg, depending on the species. Metabolism / Metabolites Sorafenib undergoes oxidative metabolism by CYP3A4 in the liver, as well as glucuronidation by UGT1A9 in the liver and kidneys. At steady-state, sorafenib accounts for 70-85% of the circulating analytes in plasma. About eight metabolites of sorafenib have been identified, of which five were detected in plasma. The main circulating metabolite was the pyridine N-oxide form, which comprises approximately 9–16% of the total circulating dose at steady-state: the pharmacological activity of this metabolite was comparable to the parent drug. Sorafenib undergoes oxidative metabolism by hepatic CYP3A4, as well as glucuronidation by UGT1A9. Inducers of CYP3A4 activity can decrease the systemic exposure of sorafenib. Sorafenib accounted for approximately 70-85% of the circulating analytes in plasma at steady-state. Eight metabolites of sorafenib have been identified, of which 5 have been detected in plasma. The main circulating metabolite of sorafenib, the pyridine N-oxide that comprises approximately 9-16% of circulating analytes at steady-state, showed in vitro potency similar to that of sorafenib. Sorafenib has known human metabolites that include Sorafenib and A-D-GlucuronideDISCONTINUED. Sorafenib is metabolized primarily in the liver, undergoing oxidative metabolism, mediated by CYP3A4, as well as glucuronidation mediated by UGT1A9. Sorafenib accounts for approximately 70-85% of the circulating analytes in plasma at steady- state. Eight metabolites of sorafenib have been identified, of which five have been detected in plasma. The main circulating metabolite of sorafenib in plasma, the pyridine N-oxide, shows in vitro potency similar to that of sorafenib. This metabolite comprises approximately 9-16% of circulating analytes at steady-state. Route of Elimination: Following oral administration of a 100 mg dose of a solution formulation of sorafenib, 96% of the dose was recovered within 14 days, with 77% of the dose excreted in feces, and 19% of the dose excreted in urine as glucuronidated metabolites. Half Life: 25-48 hours Biological Half-Life The mean elimination half-life of sorafenib was approximately 25 to 48 hours. After intravenous administration of (14)C-sorafenib tosylate to mice, rats, and dogs the elimination of the radioactivity from plasma occurred with similar terminal half-lives of 6.8, 8.8, and 7.3 hours, respectively. The terminal half-lives of radioactivity after oral administration were 6.1 hours in mice and 5.8 hours in dogs. In rats, terminal half-live after oral administration was longer (11.2 hr) than after intravenous administration. In rats, the elimination of the unchanged compound was slower (half life: 9.3 hr) than in the mice (half life: 6.5 hr) and dogs (half life:4.3 hr). The mean elimination half-life of sorafenib was approximately 25 to 48 hours. |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
Sorafenib interacts with multiple intracellular (CRAF, BRAF and mutant BRAF) and cell surface kinases (KIT, FLT-3, VEGFR-2, VEGFR-3, and PDGFR-ß). Several of these kinases are thought to be involved in angiogenesis, thus sorafenib reduces blood flow to the tumor. Sorafenib is unique in targeting the Raf/Mek/Erk pathway. By inhibiting these kinases, genetic transcription involving cell proliferation and angiogenesis is inhibited. Hepatotoxicity In large clinical trials of sorafenib, elevations in serum aminotransferase levels were common, occurring in up to half of patients, but values greater than 5 times the upper limit of normal (ULN) occurred in only 1% to 3% of treated subjects. In addition, there have been several single case reports of clinically apparent liver injury arising during sorafenib therapy which was often severe and occasionally fatal. The onset of acute liver injury ranged from a few days to 8 weeks of starting sorafenib, and the pattern of injury was typically hepatocellular with marked elevations in serum aminotransferase levels. Immunoallergic and autoimmune features were absent. Recovery was usually rapid once sorafenib was stopped, but some cases were associated with progressive liver injury and hepatic failure. Most of the reports of severe liver injury occurred in patients being treated for hepatocellular carcinoma who also had cirrhosis or in patients receiving other potentially hepatotoxic drugs31. Likelihood score: B (likely cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation No information is available on the clinical use of sorafenib during breastfeeding. Because sorafenib is 99.5% bound to plasma proteins, the amount in milk is likely to be low. However, its half-life is 25 to 48 hours and it might accumulate in the infant. The manufacturer recommends that breastfeeding be discontinued during sorafenib therapy and for 2 weeks after the last dose. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding _In vitro_, sorafenib is 99.5% bound to human plasma proteins. Interactions Sorafenib does not appear to affect the metabolism of warfarin (a CYP2C9 substrate) in vivo; mean changes from baseline in prothrombin time (PT)/international normalized ratio (INR) did not appear to be greater in patients receiving sorafenib as compared with placebo. However, infrequent bleeding events or elevations in INR have been reported in some patients receiving concomitant therapy with warfarin and sorafenib. Potential pharmacokinetic interaction with doxorubicin and irinotecan (increased area under the serum concentration-time curve (AUC) of doxorubicin and of irinotecan and its active metabolite SN-38). The clinical importance of these findings is not known. Caution is advised. In vitro studies indicate that sorafenib inhibits glucuronidation by the uridine diphosphate-glucuronosyltransferase (UGT) 1A1 and 1A9 pathways; potential pharmacokinetic interaction (increased systemic exposure to UGT 1A1 or 1A9 substrates). Caution is advised when sorafenib is used concomitantly with drugs predominantly metabolized by the UGT 1A1 pathway (e.g., irinotecan, whose active metabolite SN-38 is metabolized by UGT 1A1). In vitro studies using human hepatic microsomes indicate that sorafenib inhibits CYP isoenzymes 2B6, 2C8, 2C9, 2C19, 2D6, and 3A4; however, sorafenib does not appear to alter exposure to dextromethorphan (a CYP2D6 substrate), midazolam (a CYP3A4 substrate), or omeprazole (a CYP2C19 substrate). The manufacturer states that it is unlikely that sorafenib will alter the metabolism of substrates of CYP isoenzymes 2C19, 2D6, or 3A4 in vivo or induce CYP isoenzymes 1A2 or 3A4. However, sorafenib may increase systemic exposure to CYP2B6 or CYP2C8 substrates; caution is advised when substrates of CYP2B6 or CYP2C8 are used concomitantly with sorafenib. For more Interactions (Complete) data for Sorafenib (6 total), please visit the HSDB record page. |
| 参考文献 | |
| 其他信息 |
Therapeutic Uses
Antineoplastic Agents; Protein Kinase Inhibitors Nexavar is indicated for the treatment of patients with unresectable hepatocellular carcinoma (HCC). /Included in US product label/ Nexavar is indicated for the treatment of patients with locally recurrent or metastatic, progressive, differentiated thyroid carcinoma (DTC) that is refractory to radioactive iodine treatment. /Included in US product label/ Nexavar is indicated for the treatment of patients with advanced renal cell carcinoma (RCC). /Included in US product label/ Drug Warnings Palmar-plantar erythrodysesthesia (commonly referred to as hand-foot syndrome) and rash are common adverse effects of sorafenib, occurring in 30 and 40%, respectively, of patients receiving the drug in clinical studies, compared with 7 and 16%, respectively, of patients receiving placebo. Analysis of cumulative event rates suggests that rash and hand-foot syndrome usually are grade 1 or 2 and generally appear during the first 6 weeks of treatment with sorafenib. Management of dermatologic toxicities may include topical therapies for symptomatic relief, temporary interruption of therapy, and/or dosage modification of sorafenib; in severe or persistent cases, permanent discontinuance of sorafenib therapy may be necessary. Possible increased risk of bleeding. In clinical studies, bleeding (regardless of causality) was reported in 15.3 or 8.2% of patients receiving sorafenib or placebo, respectively. The incidences of grade 3 and 4 bleeding were 2 and 0%, respectively, in patients receiving sorafenib compared with 1.3 and 0.2%, respectively, in patients receiving placebo. Fatal hemorrhage occurred in one patient in each treatment group. Permanent discontinuance of sorafenib should be considered if any bleeding episode requires medical intervention. GI perforation, sometimes associated with apparent intra-abdominal tumor, has been reported rarely in patients receiving sorafenib. Sorafenib therapy should be discontinued if GI perforation occurs. Based on its mechanism of action and findings in animals, Nexavar may cause fetal harm when administered to a pregnant woman. Sorafenib caused embryo-fetal toxicities in animals at maternal exposures that were significantly lower than the human exposures at the recommended dose of 400 mg twice daily. Advise women of childbearing potential to avoid becoming pregnant while on Nexavar because of the potential hazard to the fetus. For more Drug Warnings (Complete) data for Sorafenib (16 total), please visit the HSDB record page. Pharmacodynamics Sorafenib decreases tumour cell proliferation _in vitro_. It attenuated tumour growth of human tumour xenografts in immunocompromised mice, reduced tumour angiogenesis, and increased tumour apoptosis in models of hepatocellular carcinoma, renal cell carcinoma, and differentiated thyroid carcinoma. Some studies suggest that sorafenib induces apoptosis in several tumour cell lines, although this effect is inconsistent across cell lines. Antiviral effects of sorafenib have been documented, as it was shown to inhibit hepatitis C viral replication _in vitro_. |
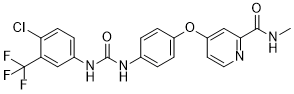
| 分子式 |
C21H16CLF3N4O3
|
|---|---|
| 分子量 |
464.82
|
| 精确质量 |
464.086
|
| 元素分析 |
C, 54.26; H, 3.47; Cl, 7.63; F, 12.26; N, 12.05; O, 10.33
|
| CAS号 |
284461-73-0
|
| 相关CAS号 |
Sorafenib Tosylate;475207-59-1;Sorafenib-d3;1130115-44-4;Sorafenib-d4;1207560-07-3;Sorafenib-13C,d3;1210608-86-8
|
| PubChem CID |
216239
|
| 外观&性状 |
white solid powder
|
| 密度 |
1.5±0.1 g/cm3
|
| 沸点 |
523.3±50.0 °C at 760 mmHg
|
| 熔点 |
202-204°C
|
| 闪点 |
270.3±30.1 °C
|
| 蒸汽压 |
0.0±1.4 mmHg at 25°C
|
| 折射率 |
1.626
|
| LogP |
5.16
|
| tPSA |
92.35
|
| 氢键供体(HBD)数目 |
3
|
| 氢键受体(HBA)数目 |
7
|
| 可旋转键数目(RBC) |
5
|
| 重原子数目 |
32
|
| 分子复杂度/Complexity |
646
|
| 定义原子立体中心数目 |
0
|
| SMILES |
FC(F)(F)C1C=C(NC(NC2C=CC(=CC=2)OC2=CC=NC(C(=O)NC)=C2)=O)C=CC=1Cl
|
| InChi Key |
MLDQJTXFUGDVEO-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C21H16ClF3N4O3/c1-26-19(30)18-11-15(8-9-27-18)32-14-5-2-12(3-6-14)28-20(31)29-13-4-7-17(22)16(10-13)21(23,24)25/h2-11H,1H3,(H,26,30)(H2,28,29,31)
|
| 化学名 |
4-[4-[[4-chloro-3-(trifluoromethyl)phenyl]carbamoylamino]phenoxy]-N-methylpyridine-2-carboxamide
|
| 别名 |
BAY 43-9006; BAY-439-006; BAY439006; BAY-439006; BAY 439006; BAY 549085; trade name: Nexavar; SFN
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 4 mg/mL (8.61 mM) in 2% DMSO + 40% PEG300 + 5% Tween80 + 53% Saline (这些助溶剂从左到右依次添加,逐一添加), 悬浮液;超声助溶。
*生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: 2.08 mg/mL (4.47 mM) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 悬浊液; 超声助溶。 例如,若需制备1 mL的工作液,可将 100 μL 20.8 mg/mL澄清的DMSO储备液加入到400 μL PEG300中,混匀;再向上述溶液中加入50 μL Tween-80,混匀;然后加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.08 mg/mL (4.47 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: ≥ 2.08 mg/mL (4.47 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,你可以将100 μL 20.8 mg/mL澄清的DMSO储备液加入到900 μL玉米油中,混合均匀。 配方 5 中的溶解度: 5%DMSO+45%PEG400+50%H2O: 0.375mg/mL 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.1514 mL | 10.7569 mL | 21.5137 mL | |
| 5 mM | 0.4303 mL | 2.1514 mL | 4.3027 mL | |
| 10 mM | 0.2151 mL | 1.0757 mL | 2.1514 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Prospective, Non-interventional, Post-authorization Safety Study That Includes All Patients Diagnosed as Unresectable Differentiated Thyroid Carcinoma and Treated With Sorafenib
CTID: NCT02185560
Phase: Status: Active, not recruiting
Date: 2024-11-20
The number of nuclei breaking the internal limiting membrane (ILM). A: Controlled group; B: ROP group; C: Vehicle-treated ROP group; D: Low doses sorafenib-treated ROP group; E: Middle doses sorafenib-treated ROP group; F: High dose sorafenib-treated ROP group. |
 |
 |